Research - (2021) Volume 9, Issue 6
Cytomorphological Study of Cervical Smears and Correlation with Cervical Biopsy
Mellonie and Ponnuswamy Karkuzhali*
*Correspondence: Ponnuswamy Karkuzhali, Department of Pathology, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
Since introduction of cytology as a diagnostic tool in the middle of nineteenth century, this branch has made rapid strides in the last one century. There are several studies in literature describing the various patterns observed in Cytomorphological examination of cervical smears and their association with different clinical presentations .Many have also correlated cytology with histopathology findings and pointed out that cytology correlated well with histopathology and has a high sensitivity, specificity & diagnostic accuracy. Cervical cytology has proved over the years to be a good screening tool to diagnose cervical carcinoma and premalignant lesions of cervix. Hence, the purpose of this study is to evaluate the Cytomorphological pattern of cervical smears in symptomatic women attending SBMCH and to compare them with their clinical presentations and histopathological findings wherever available.
Keywords
Cytomorphology, Cervical smears, Cervical biopsy, Cytology, Cervical cancer, Histopathology
Introduction
Cytology is a branch of science which deals with the study of cells. Two main branches of cytology are Aspiration cytology and Exfoliative cytology.
Exfoliative Cytology is the study of the normal and the disease altered desquamated cells from various sites. The rate of desquamation varies with each tissue, its function, and metabolic capacities. There are two types of cellular exfoliation.
Natural spontaneous exfoliation
The physiologically desquamated cells will often show, besides the normal changes of natural ageing the pathological changes as well. Vaginocervical cells in the vaginal pool secretion in the posterior vaginal fomix and mesothelium cells in the effusions of the pleural and abdominal cavities are studied by spontaneous exfoliation.
Artificial exfoliation (surface microbiopsy)
Surface of the mucosa is scraped or tissue is aspirated with a needle and viable cells are traumatically exfoliated before their natural time of shedding.
The study of exfoliative cytology was first described in the middle of nineteenth century [1]. In 1928 George Papanicolaou described tumour cells could be found in cervical smear from a patient with cervical cancer and suggested that examination of cervical smear provided new opportunity to detect cervical cancer [2]. From then on cervical smears were widely used in screening of cervical cancer. Various systems have been used to classify lesions seen in cervical smears. The Bethesda System (2001) is the currently practiced system. Cytomorphological study of cervical smears is highly beneficial mainly because of the following 3 reasons [3]: 1. Unsuspected diseases may be detected with a high degree of sensitivity and specificity. 2. The nature of suspected diseases can be confirmed without trauma 3. The course of the disease or its response to therapy can be monitored.
Some of the advantages of using cytology instead of histopathological examination are as follows.
• Cytological methods are rapid, inexpensive and simple.
• There is no injury to the tissue hence, repetitive sampling can be done.
• Smears cover wider surface than that involved in a biopsy.
• Evaluation of the progression or post treatment regression of a lesion can be done.
• Intimate cellular structures are seen clearly in isolated cell of a smear because of the minimum shrinkage and distortion in such cells.
• Hormonal status can be evaluated by cytological method than biopsy.
• Evaluation of the nature of inflammation or infection can be done.
• Changes due to irradiation and other forms of therapies are often easier to evaluate.
Hence, the purpose of this study is to evaluate the cytomorphological pattern of cervical smears in symptomatic women attending SBMCH and to compare them with their clinical presentations and histopathological findings wherever available.
Materials and Methods
Source of data
A prospective study on 703 women aged 21years and above attending the gynaecology OPD of SBMCH between September 2012 to August 2014 with complaints of white discharge, irregular menstrual bleeding, postmenopausal bleeding and post coital bleeding was done.
Processing
In each case after recording relevant clinical data, cervical smear was taken using Ayre's spatula and stained with pap stain. Cytomorphological features were studied and correlated with clinical features. Normal smears and unsatisfactory smears were not included in the study. Biopsy was available m 199/703 cases. Cyto histopathological correlation was done for these 199 cases.
Method of collection of PAP smear
For preparation of smears the following reagents and equipments were needed.
• Clean glass slides.
• Diamond marking pencil
• Cover slip
• Absolute methanol in Coplin jar as fixative
• Wooden Ayre spatula
• Sterile vaginal speculum
• A pair of sterile gloves.
Patient preparation
• Abstinence from coitus for 24hrs prior to the procedure.
• No intravaginal medication for 1 week prior to the test.
• No lubricants should be used during the procedure.
Collection of Pap smear
For collecting the cervical smear patient was put in the lithotomy position. Vulva was inspected for the lesions .After inspecting and stabilizing the cervix. Ayre's spatula was inserted into the external and gently and firmly rotated at 360° degrees. By doing this procedure material was obtained from squamous columnar junction.
After obtaining, material, it was transferred on a clean glass slide and was uniformly spread using spatula and immediately kept in Coplin jar containing absolute alcohol for fixation. Slide was stained by modified Papanicolaou's stain.
Preparation of Pap stain
Preparation of harris haematoxylin
Haematoxylin powder : 2.0 gm
Ethylene glycol: 250 ml
Aluminum sulphate: 17.6 gm
Distilled water: 750 ml.
Sodium iodate: 0.2gm.
Glacial acetic acid: 20.0 ml.
The ingredients were added in order as written above in a dry clean bottle and the mixture was vigorously shaken for 1 hour at room temperature. The staining solution could be stored over one year.
Preparation of orange G-6 stain
Orange G-6 stock solution
Orange G-6 stain: 9.05gm.
Distilled water: 100 ml.
Orange G-6 working solution
Orange: G-6
Stock solution: 20 ml.
Phosphotungstic acid: 0.l 5 gm.
95% Ethyl alcohol: 980ml.
Orange G-6 working solution was changed every fortnight. The stain was filtered before use and stored in a dark bottle.
Preparation of E.A-36 Stain (Modified) light green stock solution
Light green SF yellowish: 3.17 gm.
Distilled water: 100ml.
Eosin Y stock solution
Eosin Y: 20.8 gm.
Distilled water: 100 ml.
E.A-36 working solution
95% ethyl alcohol: 700 ml
Stock eosin y stock: 20 ml
Light green absolute: 10 ml
Methanol: 250 ml
Phosphotungstic acid: 2 gm
Glacial acetic acid: 20 ml
This working solution was changed every week.
Staining of Pap smear [4]
The fixed slides are transferred directly from the fixative into the following solutions.
80% ethyl alcohol: 10dips
70% ethyl alcohol: l0dips
50% ethyl alcohol: l0dips
Distilled water: 10 dips
Harris haematoxylin: 3 min
Running tapwater: 1 min
0.5% HCL: 5 dips
Running tapwater: 1 min
Dilute solution of lithium carbonate: 1 min
Running tapwater: 1 min
50% ethyl alcohol: 10 dips
70% ethyl alcohol: 10 dips
80% ethyl alcohol: 10 dips
95% ethyl alcohol: 1 min
Orange G-6: 1 min
95% ethyl alcohol: 10 dips
95% ethyl alcohol: 10 dips
EA-36: 4min
95%ethyl alcohol: 10 dips
95% ethyl alcohol: 10 dips
Absolute alcohol: 4min
Xylene: 5 min
Slides are then mounted in DPX.
Results
Nucleus-Blue.
Superficial cell cytoplasm-Pink.
Intermediate and Parabasal cell cytoplasm-Blue-green Red. Blood cells-Orange.
The pap smears thus prepared were studied. Cytohistopathological correlation was done wherever biopsy was available. Available biopsies were fixed in 10% neutral buffered formalin, subjected to gross examination and routine processing. Sections of 4 micron thickness were cut and stained with hematoxylin-eosin stain and then studied.
Hematoxylin and eosin stain [5]
• Deparaffinised slides were immersed in first xylene bath for 3 minutes.
• Then transferred to second xylene bath for 2-3 minutes.
• Immersed in the bath of 70% alcohol for 3 minutes.
• Rinsed in running water for 1 minute and then briefly in distilled water.
• Stained with Harris's haematoxylin for 5-10 minutes and rinsed in tap water.
• Differentiated in 1% acid alcohol by dipping 3-4 times and washed.in tap water briefly.
• Bluing was done with lithium carbonate till sections appeared blue
• Rinsed in tap water for 10-20 mins.
• Stained with acidified 1%aqueous eosin for 30 seconds.
• Washed in running tap water for 1 minute.
• Dehydrated by passing through 3 baths of absolute alcohol.
• Passed through xylene for 15-20 seconds.
• Mounted in DPX.
Results
In the present study cervical smear examination of 703 women aged 21 years and above attending the gynaecology OPD of SBMCH between September 2012 to August 2014, with complaints of white discharge, irregular menstrual bleeding, postmenopausal bleeding and post coital bleeding was done. Normal smears and unsatisfactory smears were not included in the study. Cytomorphological features were studied and correlated with clinical features. Biopsy was available in 199/703 cases. Cyto-histopathological correlation was done for the same.
The following observations were made: Of the 703 pap smears screened, cases (89.2%) were inflammatory smears, 37 cases (5.3%) were LSIL, 15 cases (2.2%) were HSIL, 7 cases (0.9%) were ASCUS and 17 cases (2.41%) were atrophic smears (Table 1).
| Lesion in cytology | No. of cases | Percentage |
|---|---|---|
| Inflammatory smears | 627 | 89.20% |
| ASCUS | 7 | 0.90% |
| LSIL | 37 | 5.30% |
| HSIL | 15 | 2.20% |
| Atrophy | 17 | 2.40% |
| Total | 703 | 100% |
Table 1: Distribution of lesions in cervical smear.
Of the 627 inflammatory smears, 541(86.3%) showed nonspecific inflammation and 86(13.7%) showed specific inflammation. 86 specific inflammatory smears included, 40cases (6.4%) of Trichomonas vaginalis, 27(4.3%) cases of Candidia albicans and 19(3.0 %) cases of Bacterial vaginosis (Table 2).
| Nonspecific inflammation | 541 smear (86.3%) |
|---|---|
| Specific inflammation | |
| Trichomonas vaginalis | 40 smears (6.4%) |
| Candida albicans | 27 smears (4.3%) |
| Bacterial vaginosis | 19 smears (3.0%) |
| Total inflmmatory smears | 627 smears |
Table 2: Distribution of inflammatory smears.
Distribution of cases according to age
Out of the 703 cases in the present series, highest number of 238 cases (33.8%) belonged to 31-40 years age group (Figure 1).
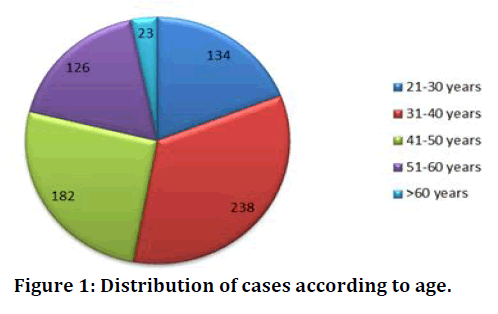
Figure 1. Distribution of cases according to age.
Clinical presentation (vs.) lesions in cytology
Peak incidence of 72.1 % of patients with inflammatory smears presented with complaint of white discharge.
Clinical complaint (vs.) lesions in cytology
Most common presenting complaint in women with LSIL & HSIL was also white discharge , the next common presentation for LSIL was irregular menstrual bleeding (18.9%) & HSIL was post-menopausal bleeding (20%). Women with ASCUS smears presented in 2 forms. 71.4% of women with ASCUS presented with post-menopausal bleeding and 28.6% presented with irregular menstrual bleeding (Table 3).
| Clinical presentation | Inflammatory smears | ASCUS | LSISL | HSIL | Atrophic smear |
|---|---|---|---|---|---|
| White discharge (491) | 452 (72.1%) | - | 19 (51.4%) | 9 (60%) | 11 (64.7%) |
| Irregular menstural bleeding (156) | 145 (23.1%) | 2 (28.6%) | 7 (18.9%) | 2 (13.3%) | - |
| Post-menopausal bleeding (37) | 17 (2.7%) | 5 (71.4%) | 6 (16.2%) | 3 (20%) | 6 (35.3%) |
| Post coital bleeding (19) | 13 (2.1%) | - | 5 (13.5%) | 1 (6.7%) | - |
| Total (703) | 627 | 7 | 37 | 15 | 17 |
Table 3: Clinical complaint (vs.) lesions in cytology.
Age wise distribution of clinical presentation
Peak incidence of irregular menstrual bleeding (62.8%) & a peak incidence of post coital bleeding (63.2%) were observed in 31-40 years age group (Table 4).
| Age (years) | White discharge | Irregular menstural bleeding | Post coital bleeding | Post-menopausal bleeding |
|---|---|---|---|---|
| 21-30 (134 Cases) | 98 (19.9%) | 30 (19.2%) | 6 (31.6%) | Nil |
| 31-40 (238 Cases) | 127 (25.9%) | 98 (62.8%) | 12 (63.2%) | 1 (2.7%) |
| 41-50 (182 Cases) | 144 (29.3%) | 19 (12.2%) | 1 (4.5%) | 18 (48.7%) |
| 51-60 (Cases) | 105 (21.4%) | 9 (5.8%) | Nil | 12 (32.4%) |
| Above 60 (23 Cases) | 17 (3.5%) | Nil | Nil | 6 (16.2%) |
| Total (703 Cases) | 491 (69.8%) | 156 (22.2%) | 19 (2.7%) | 37 (5.3%) |
Table 4: Agewise distribution of clinical presentation.
Age wise distribution of lesions in cytology
Peak incidence of HSIL (40%) was between 51-60 years (Table 5).
| Age (years) | Inflammation | ASCUS | LSISL | HSIL | Atrophic smear |
|---|---|---|---|---|---|
| 21-30 | 128 (20.4%) | Nil | 5 (13.6%) | 1 (6.7%) | Nil |
| 31-40 | 230 (36.7%) | Nil | 7 (18.9%) | 1 (6.7%) | Nil |
| 41-50 | 159 (25.4%) | 4 (57.11%) | 14 (37.8%) | 5 (33.3% | Nil |
| 51-60 | 98 (15.6%) | 2 (28.6%) | 9 (24.3%) | 6 (40%) | 11 (64.7%) |
| Above 60 | 12 (1.9%) | 1 (14.3%) | 2 (5.4%) | 2 (13.3%) | 6 (35.3%) |
| Total | 627 (89.2%) | 7 (0.9%) | 37 (5.3%) | 15 (2.2%) | 17 (2.4%) |
Table 5: Age wise distribution of lesions in cytology.
Age wise distribution of lesions in cytology
Peak incidence of ASCUS (57.1%) and LSIL (37.8%) was between 41-50 years.
Distribution of lesions in histopathology
Out of 703 patients in the present series cervical biopsy was available in 199 cases. Of which 125 cases(62.81%) were chronic cervicitis, 40cases(20.10%) were CIN-1, 6 cases (3.01%) were CIN-2, 9cases (4.52%) were CIN-3 and 3 cases ( 1.52%) were invasive cervical carcinoma (Table 6).
| Lesion in histopathology | No. of cases | Percentage |
|---|---|---|
| Normal | 16 | 8.10% |
| Chronic cervicitis | 125 | 62.80% |
| CIN-I | 40 | 20.10% |
| CIN-2 | 6 | 3% |
| CIN-3 | 9 | 4.50% |
| Squamous cell carcinoma | 3 | 1.50% |
| Total | 199 | 100.00% |
Cyto-histopathological correlation of cervical smears
Out of 199 biopsies available for correlation, 177/199 cervical smears correlated correctly with histopathology (Table 7).
| Cytological diagnosis | No. of cases | Histopathological diagnosis | No. of cases | No. of cases correlated |
|---|---|---|---|---|
| Inflammation | 140 | Chronic cervicitis | 124 | 124/140 |
| Normal | 16 | |||
| ASCUS | 7 | CIN-1 | 6 | 7-Jul |
| Chronic cervicitis | 1 | |||
| LSIL | 37 | CIN-1 | 34 | 34/37 |
| CIN-2 | 3 | |||
| HSIL | 15 | CIN-2 | 3 | 15-Dec |
| CIN-3 | 9 | |||
| Carcinoma | 3 | |||
| Total | 177/199 | |||
Table 7: Cyto-histopathological correlation of cervical smears.
Smear shows superficial and intermediate cells and Trichomonas vaginali s organism, seen as a discrete, faintly greyish-blue body; round or oval in shape in an acute inflammatory background (Figure 2). Smear shows squamous cells in acute inflammatory background. budding yeast & hyphae of Candida albicans is seen (Figure 3). Smear shows superficial and intermediate cells in an acute inflammatory background with mild shift in bacterial flora. Presence of clue cell 1s diagnostic of Bacterial vaginosis (Figure 4). Smear shows scattered basal cells and few parabasal cells with a dried background (Figure 5).
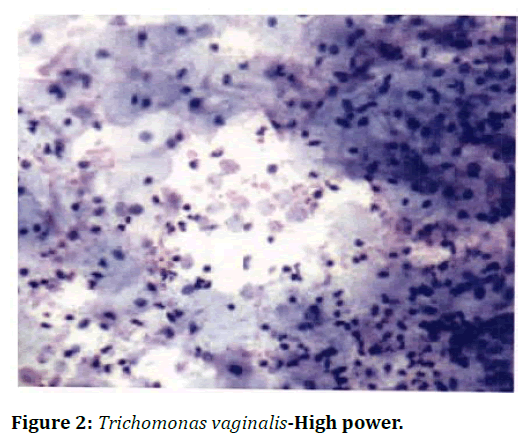
Figure 2. Trichomonas vaginalis-High power.
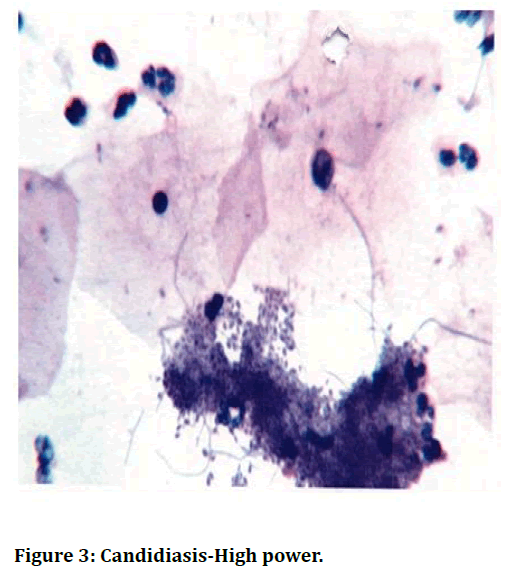
Figure 3. Candidiasis-High power.
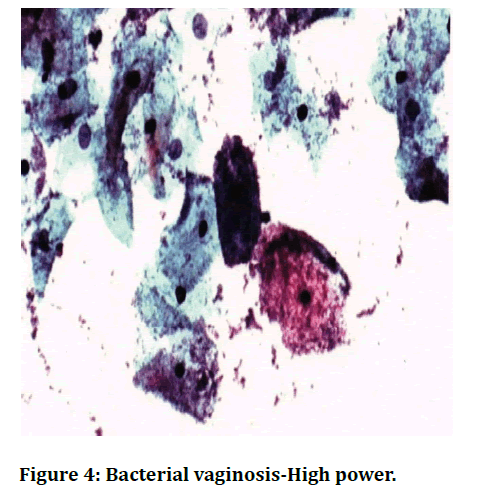
Figure 4. Bacterial vaginosis-High power.
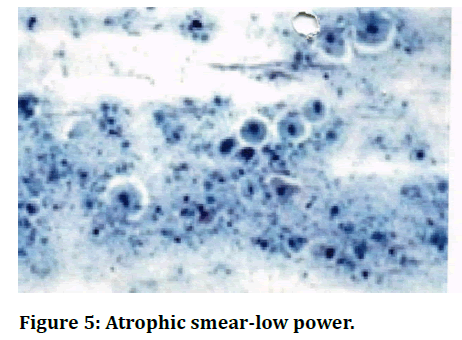
Figure 5. Atrophic smear-low power.
• Of the 703 pap smears screened , 627 cases (89.2%) were inflammatory smears, 37 cases(5.3%)were LSIL, 15cases(2.2%) were HSIL, 7 cases (0.9%) were ASCUS and 17 cases (2.41%) were atrophic smears.
• Of the 627 inflammatory smears, 541(86.3%) showed nonspecific inflammation and 86(13.7%) showed specific inflammation. 86 specific inflammatory smears included
• , 40 cases (6.4%) of Trichomonas vaginalis, 27(4.3%) cases of Candidia albicans and 19(3.0%) cases of Bacterial vagmosis.
• Out of 703 pap smears studied, highest number of 238 cases (33.8%) was between 31-40 years & lowest number of 23 cases (3.3%) was above 60 years
• Most common clinical presentation was white discharge (69.8%) followed by irregular menstrual bleeding (22.2%)
• In the present study, peak incidence of 35.5% of inflammatory smears was between 31-40 years.
• Peak incidence of ASCUS (57.15%) and LSIL (37.83%) was between 41-50 years.
• Peak incidence of HSIL (40%) was between 51-60 years.
• Majority (72.l %) of patients with inflammatory smears presented with complaint of white discharge. Most common presenting complaint in women with LSIL & HSIL was also white discharge, the next common presentation for LSIL was irregular menstrual bleeding (18.9%)& HSIL was postmenopausal bleeding (20%)
• 71.4% of women with ASCUS presented with postmenopausal bleeding and 28.6% presented with irregular menstrual bleeding.
• Out of 199 biopsies available for correlation, 177 cervical smears correlated with histopathology.
Discussion
Cervical smear examination is a rapid, cost-effective & atraumatic method for screening of cervical lesions. In the present study cervical smear examination for 703 women aged 21 years and above , attending the gynaecology OPD of SBMCH between September 2012 to August 2014 with complaints of white discharge, irregular menstrual bleeding, postmenopausal bleeding and post coital bleeding was done. Normal smears and unsatisfactory smears were not included in the study. Cytomorphological features were studied & correlated with clinical features. Out of 703 cervical smears 199 biopsies were available for correlation. In rest of the cases biopsy was not available as biopsy was not clinically indicated. Cyto-histopathalogical correlation was done for these 199 cases.
Pattern of cytomorphological lesions
In the present study out of the 703 cervical smears screened, 627 (89.2%) were inflammatory smears, 37 (5.3%) were LSIL, 15 (2.2%) were HSIL, 7 (0.9%) were ASCUS and 17 (2.4%) were atrophic smears. Of the 627 inflammatory smears, 541(86.3%) showed non-specific inflammation and 86 (13.7%) showed specific inflammation. 86 specific inflammatory smears included, 40 cases (6.4%) of Trichomonas vaginalis, 27 (4.3%) cases of Candidia albicans and 19 (3.0%) cases of Bacterial vaginosis. Similar study was conducted by Sardana et al (1994) in which out of 63,265 cervical smears studied, 52,636 (83.2%) were inflammatory smears, 2647 (4.1%) were mild dysplasia, 756 (1.2%) were moderate dysplasia and 947 (1.5%) were severe dysplasia [6]. Misra JS et al conducted a study on 19,449 women, of which 16575 (85.3%) were inflammatory smears, 936 (4.3%) were LSIL, 370 (1.9%) were HSIL, 972 (5.1%) were Trichomonas vaginalis, 769 (3.9%) were Candida albicans, 489 (2.5%) were Bacterial vaginosis & 436 (2.1%) were atrophic smears [7]. In 2013, a study conducted in high risk women by Jothi R et al showed that among the pap smears screened 180 (8%) were normal, 102 (4.5 %) unsatisfactory, 1786 (79 .4%) inflammatory smears, l16 (5.3%)LSIL, 54 (2.5%) HSIL, 45 (2%) atrophic & 3 (0.9%) frank carcinoma [8].
Clinical presentation (vs.) cytological lesions
In the present study (2014), out of 703 women, 491 (69.84%) presented with white discharge, 156 (22.19%) with irregular menstrual bleeding, 19 (2.7%) with postcoital bleeding and 37 (5.26%) with postmenopausal bleeding. In our study the most common clinical presentation was white discharge 491 cases (69.8%) followed by irregular menstrual bleeding 156 cases (22.2%) also the most common presenting complaint of women with inflammatory smears was white discharge (72.1%). Other than the observation that the most common presenting complaint in women with LSIL & HSIL was also white discharge, the next common presentation for LSIL was irregular menstrual bleeding (18.9%) & HSIL was post-menopausal bleeding (20%). Out of 7 women with ASCUS smears 5 (71.4%) presented with post-menopausal bleeding and 2 (28.6%) presented with irregular menstrual bleeding. Chhabra et al conducted a cytomorphological study of cervical PAP smears in 1812 patients who presented with complaints of white discharge, irregular menstrual bleeding, postmenopausal bleeding and postcoital bleeding [9] and he concluded that white discharge was associated with inflammatory smears and post-menopausal bleeding was common in precancerous lesions of cervix. Misra et al conducted a study in 1574 symptomatic women of which 1152 (73.2%) presented with white discharge, 355 (22.6%) presented with menorrhagia, 46 (2.9%) with contact bleeding and 21 (1.3%) with postmenopausal bleeding [7], again concluding that white discharge was the most common clinical presentation in women subjected to cervical smear examination. Also inflammatory smear was common in women with white discharge whereas intraepithelial lesion was common in women with post-menopausal bleeding. In 2013 in a study conducted by Bolla Chandrasekhar Reddy et al revealed a high increase of LSIL and frank carcinoma commonly observed in those women presenting with bleeding problems (irregular menstrual bleeding/postmenopausal bleeding) [10].
Age (vs.) cytological lesions
In the present study, peak incidence of 35.5% of inflammatory smears was observed in 31-40 years age group. Peak incidence of ASCUS (57.15 %) and LSIL(37.83 %) was observed in 41-50 years age group and Peak incidence of HSIL(40% ) was observed in 51-60 years age group. Several studies in literature correlated with the present study. Reagan (1956) reported that the mean age at which LSIL was detected to be 41.4 years [11]. Misra JS et al (1997) reported in their study, a high incidence of cervical dysplasia in women between 31-40 years of age (4.1%) [7]. In 2003 , P Sasieni et al conducted a study on 1305 women aged 20-69 years and concluded that 3-yearly screening offers additional protection (84%) over 5-yearly screening (73%) against cervical cancers at ages 40-54 years [12], thus concluding the high incidence of squamous intraepithelial lesions being picked up between 40 - 54 years [13]. National Cancer Registry Programme, ICMR has mentioned that in India, age specific rates for Squamous Intraepithelial Lesions are highest in the age group of 50 to 59 years with average age of occurrence being 50.3 years [9]. Misra JS et al (2004) reported in their study, a high incidence (64.7%) of inflammatory smears in women between 31-40 years of age [7]. In 2009, Peter Sasieni et al revealed that screening was associated with a 60% reduction of cancers in women aged 40, increasing to 80% at age 64 [14]. Thus establishing high incidence cervical intraepithelial lesions in age group of 40 - 64 years. In 2014 Alexandra Castafion et al concluded that, screening between 50 to 64 years decreased the incidence of cervical cancer by 75%, thus emphasizing the high incidence of intraepithelial lesions being detected in 50-64 years [15].
Cyto-histopathological correlation
In the present series of 703 cases, 199 cases biopsy was available for correlation. In rest of the cases biopsy was not available because the lesion was benign on cervical cytology or biopsy was not clinically indicated. Out of the 199 biopsies available for correlation 177 cases showed correlation. Among the remaining 22 cases showing diagnostic discordance, 16 were reported as inflammatory smear on cytology but turned out to be normal on biopsy. This may be because inflammation in the smear might have come from vaginitis or the inflammation had subsided by the time biopsy was taken. Also 3 cases reported as LSIL turned out to be CIN-2 on biopsy. These 3 cases were actually HSIL which had been underdiagnosed as LSIL on PAP smear. Gupta. S et al (2004) in his study observed that 26% of HSIL cases were underdiagnosed as LSIL on cervical smears. The major confounding factors responsible for under interpretation on cytology included air drying artefacts and metaplastic maturation of abnormal cells [16]. Three cases reported as HSIL on cervical smear turned out to be Squamous cell carcinoma on biopsy. Possible explanation may be pointed out from the study conducted by Subhalakshmi et al [17] in 2013 which revealed that to diagnose carcinoma; presence of tumour diathesis in the background is the only differentiating feature separating HSIL from carcinoma. Since there is only a thin line of 'demarcation between HSIL and carcinoma at cytology level, it was suggested that a special phrase may be added as and when necessary to HSIs 'HSIL-with features suspicious of invasion'. Though these 6 cases have been underdiagnosed in cervical smear, the intraepithelial lesions have still been picked up in the cervical smear and the patients were rightly directed to undergo cervical biopsy for confirmation. Hence cervical smear still continues to be a good screening tool.
In the present study cervical smear's sensitivity is 88.1%, specificity is 91.5% Positive predictive value is 86.7 % & diagnostic concordance rate is 88.9%. Several authors have reported variable results on cytohistopathological correlation. It is difficult to compare the available data which has been published over a long span of time as uniform terminology was not employed. Studies with results similar to the present study have been tabulated.
Conclusion
Cervical cytology is used for hormonal study and to detect exfoliated cancer cells from uterine cervix ever since the introduction by Papanicolaou in 1941. Cervical cytology is a good screening modality for the early detection of cancer cells (i.e.) early detection of cervical cancer. The present study shows peak incidence of ASCUS, LSIL between 31-40 years and peak incidence of HSIL between 41-50 years & emphasises the importance of screening women particularly in these age groups by cervical cytology. The diagnostic concordance rate of 88.8% proves that there is good correlation between cervical cytology and histopathology. Thus, screening of woman by cervical smear examination proves to be a simple and cost effective method for early detection of premalignant and malignant cervical lesions.Funding
No funding sources.Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Coleman DV, Evans DMD. Biopsy and pathology and cytology of the cervix. Chapman and Hall Ltd., London, 1st Edition 1988; 3-237.
- https://onlinelibrary.wiley.com/doi/abs/10.1002/path.1711500413
- Naib Z M. Exfoliative cytology. 3rd Edn.
- Bancroft J.D and Stevens A. Theory and practice of histological techinques, 3rd Edn, 471-480.
- https://www.elsevier.com/books/theory-and-practice-of-histological-techniques/bancroft/978-0-443-10279-0
- Sardana S, Sodhani P, Agarwal SS, et al. Epidemiologic analysis of Trichomonas vaginalis infection in inflammatory smears. Acta cytologica 1994; 38:693-7.
- Misra JS, Pandey S, Singh U, et al. Significance of inflammatory smears in cervical Cytology. J Cytol 2004; 21:20-22.
- Jothi R,Gupta P, Roa R, et al. Correlation between colposcopy, cytology and histopathology among high risk patients for cervical cancer in perimenopausal women in Himachal Pradesh. Indian J South Asian Feder Menopause Soc 2013; 1:21-23.
- Chhabra Y, Bal GB, Janet K, et al. Histomorphological study of cervical PAP smears for pre -cancerous and cancerous lesions. J Cytol 2003; 20:64-67.
- Bolla Chandrasekhar Reddy, AR Rao, KV Phani Madhavi, et al. Study of cervical cytology in menopausal women- In a maternity and general hospital, Hyderabad, Andhra Pradesh". J Evolution Med Dent Sci 2013; 2:6824-6830.
- Reagan JW, Hamonic MJ. Dysplasia of uterine cervix. Ann NY cancer. Am J Epidemiol 1989; 130:486-96.
- Sasieni P, Adams J, Cuzick J. Benefit of cervical screening at different ages: evidence from the UK audit of screening histories. Br J Cancer 2003; 89:88-93.
- Misra JS, Das K, Harish A. Cytological studies in women complaining of leucorrhea. J Cytol 1997; 14:11.
- Peter Sasieni, Alejandra Castanon, Jack Cuzick, et al. Effectiveness of cervical screening with age: population based case-control study of prospectively recorded data. BMJ 2009; 339:b2968.
- Castafi6n A, Landy R, Cuzick J, et al. Cervical Screening at age 50-64 years and the risk of cervical cancer at age 65 years and older: Population-based case control study. PLoS Med 2014; 11:el001585.
- Gupta Sanjay, Sodhani P. Why is high grade squamous intraepithelial neoplasia under-diagnosed on cytology in a quarter of cases? Analysis of smear characteristics in discrepant cases. Indian J Cancer 2004; 41:104-108.
- Mukhopadhyay S, Ray S, Dhar S, et al. Evaluation of the category high-grade squamous intraepithelial lesion in The bethesda system for reporting cervical cytology. J Cytol 2013; 30:33-35.
Author Info
Mellonie and Ponnuswamy Karkuzhali*
Department of Pathology, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Mellonie, Ponnuswamy Karkuzhali, Cytomorphological Study of Cervical Smears and Correlation with Cervical Biopsy, J Res Med Dent Sci, 2021, 9(6): 414-422
Received: 08-May-2021 Accepted: 23-Jun-2021
