Research - (2020) Advances in Dental Surgery
Decision Tree Analysis on Management of Deep Carious Lesion
Shree Ranjan Pandey and Nivedhitha MS*
*Correspondence: Nivedhitha MS, Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Science, Saveetha University, Chennai, India, Email:
Abstract
An ongoing active carious lesion is the main cause of dental pain, this is often associated with presence of dental cavities, presence of adherent plaque-based biofilm, lack of aesthetics and associated structural and functional problems. To further prevent the spread of the active carious lesion restorative intervention is of great significance. The tooth structure preservation is important to have a positive response when pulpal sensibility tests are performed, in addition to this carious tissue removal should be adapted accordingly to cause minimal damage to the remaining dentin structure, this can be done by employing a minimally invasive approach. The removal of the carious tissue depends on the proximity of the lesion to the pulp, pulpal sensibility responses, the extent of the remaining supragingival tooth structure and the operator control-based factors like moisture control and access. The removal of the soft dentine is recommended in deep carious lesion, avoiding the pulpal exposure followed by sealing of the dentinal tubules beneath the adhesive restoration. The modern technologies of air abrasion, the use of chemo mechanical agents, and rotary plastic burs are the recent advancement in soft tissue caries removal. Avoiding the pulpal exposure must be the key factor in managing such lesions, with healthy enamel/dentine margins at the cavity periphery and by using adhesive restorative biomaterials is very critical to manage such lesions.
Keywords
Carious lesion, Dental pain, Demineralised dentine, Dentine removal, Calcium hydroxide
Introduction
Clinicians must justify the decisions taken in the management of such lesions, to the patient and to ethically themselves. These decisions should be morally and ethically justified, be well documented and must be effectively communicated to the patient. The following are the most important reasons for placing the restoration in the diseased tooth to further stop the progression of active carious lesion. A restoration when placed efficiently eradicates a hard to clean plaque biofilm-based stagnation site which provides an easily cleanable tooth surface that would encourage patients to keep an optimal oral hygiene procedure disturbing the structure of plaque formation [1]. These procedures relieve the acute pain caused by reversible pulpitis. A restoration further helps in recreating the structural and the functional integrity of the arch while providing the aesthetic outcome [2]. The traditional rationale of removing all the diseased tissue has been challenged as the excessive removal of the tooth structure further caused the poor prognosis of the tooth. This outdated concept of complete removal of the entire tooth structure was over destructive in nature when considering the viability of the tooth structure. The removal of the carious lesion should be done in a specific monitored way with the associated challenges with it. While removing the specific carious lesion several challenges must be considered which help enhance the prognosis of partially decayed tooth structure.
The first and the foremost being the knowledge of the histological tissue being treated enamel, denine or pulp. The other relevant factors being the chemistry behind the adhesive bioactive and the materials which are bio-interactive to restore the optimum tooth structure and the practical operative technologies which are of invasive nature which offer to remove minimal tooth structure selectively with addition of factors which enhance the prognostic outcome like moisture control , instrument accessibility etc. [3].
An appreciation of such factors helps the oral healthcare practitioner to provide a better outcome as compared to the traditional mechanical approach of the dental surgeon which included predetermined shapes and sizes of the conventional cavity designs. These traditional methodologies were governed by the properties of the restorative material as opposed to the histological progression of the disease process [4].
These underlying principles are critical to preserve the pulpal sensibility of the tooth, tooth structure preservation and this leads to the increase in the clinical longevity of the functional tooth restoration complex [5].
The amount of carious tissue to be removed is an important factor to heal the remaining tooth structure. The carious dentine has two major components. The first being closer to the enamel of the tooth structure which is more infected and the deeper lying demineralised caries affected zone [6]. The more peripheral zone which is contaminated with caries being closer to the enamel-dentinal junction. This area is irreversibly damaged, necrotic, and softened by the longstanding heavy bacterial contamination and the proteolytic denaturation of collagen followed by the long-standing acid demineralisation of its inorganic component [7].
The underlying deeper lying demineralized dentine which is the caries affected zone is reversibly zone, but with the potential to undergo biological repair by the dentin-pulp complex, under the correct conditions. This zone also suffers from bacterial contamination but to a significantly lesser extent than the overlying contaminated dentine and the collagen is not completely denatured and is therefore repairable [8].
The wet and soft nature of the dentine makes it is an inferior substrate for the adhesion. Therefore, the coronal restoration will not last on such a weakened dentin. The deeper layer of dentine, the affected dentin offers a better adhesive mechanism to the restorative material due to its adhesive bonding potential [9].
The contaminated dentine is moist and sticky in nature and soft to a sharp dental explorer whereas demineralised dentine is leatherier and tackier in consistency. The demineralised dentine ultimately blends into the harder and starchy consistency of deeper underlying sound dentine. Carious dentine removal can be guided by the propylene dye indicator. These dyes acted as a clinical visual marker for removal of carious dentine [10]. The modern materials have ability to detect the sulphur based biological products indicating increased bacterial load present in the infected dentine, also upcoming caries detection systems highlight use of hydrazine based covalent esterification interactions specifically designed for carious dentine removal.
Therefore the carious dentine removal cannot be answered by histology and bacterial presence alone and a lot of factors have to be taken into consideration such as the size of the specific tooth lesion, oral cavity conditions, patient and dentist factors have to be considered. We have numerous highly cited publications on welldesigned clinical trials and lab studies [11-26]. This has provided the right platforms for us to pursue the current study. Our aim was to formulate a decision tree for the management of deep carious lesions.
Depth of lesion
The depth of lesion is a critical process as the extent of the advancement of lesion is a critical process in pathology of the disease. Traditional belief systems were erroneous as they focused on the fact that it is essential to remove all the diseased tooth structure even if it’s in close proximity to the pulp, this approach was dependent on the fact that bacterial count was high in the lesions in close proximity to the pulp. This aggressive removal of the carious lesion which was at close proximity to pulp causes the failure of the pulp sensibility tests and leading to unnecessary and fatal vital pulpal exposures. When such vital pulpal exposures occur, it must be managed using Calcium Hydroxide under the procedure of direct pulp capping. Various Systematic reviews and clinical studies indicate that it leads to long term loss of pulpal viability [27].
The contemporary methodology indicates that the unnecessary cavity exposure should be minimized by leaving a layer of affected unproblematic dentine, as the bacteria present in this layer of dentin which is adjacent to pulp will be killed off due to lack of nutritional supply to thrive when sealed by a restoration [28]. Therefore, the contemporary approach of caries removal not only removes the bacteria and prolongs the life of pulp but also maintains the longevity of the tooth structure by enhancing the life of the restoration (Figure 1).
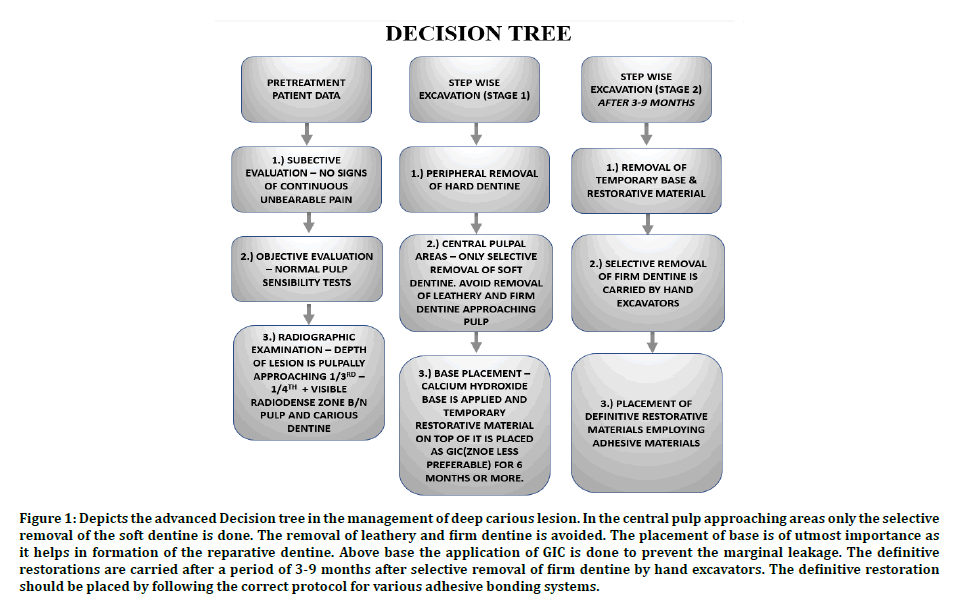
Figure 1: Depicts the advanced Decision tree in the management of deep carious lesion. In the central pulp approaching areas only the selective removal of the soft dentine is done. The removal of leathery and firm dentine is avoided. The placement of base is of utmost importance as it helps in formation of the reparative dentine. Above base the application of GIC is done to prevent the marginal leakage. The definitive restorations are carried after a period of 3-9 months after selective removal of firm dentine by hand excavators. The definitive restoration should be placed by following the correct protocol for various adhesive bonding systems.
The use of adhesive materials like Glass ionomer based liners used below the amalgam restoration or the use of Calcium silicate based cements with antibacterial properties [29] has the ability to bond and seal chemically to the remaining dentine offers a seal chemically to the remaining dentine affords a potential to seal so permitting the arrest of the carious process and tissue rejuvenation takes place via regenerative response of the pulp-dentine complex [30]. In shallow cavity the carious tissue removal is less challenging (Figure 1).
A fine balance must exist between the choice of the restorative material and amount of the affected dentine remaining. As the carious lesion is more towards the pulp it’s been found that modern alloplastic materials used for restoration have greater strength than the underlying dentine. In cases of shallow cavity the modern materials are to be used which have greater strength to keep coronal structure intact and in cases of deep cavity the restorative materials to be used should have the quality to ensure maximal pulpal survival.
Extent of viable restorable tooth structure
The functional and aesthetic restorability of the tooth is of great significance. A minimally invasive approach is preferred as it not only preserves natural tooth structure [31] but also saves operator time and patient time also. A lesser surface area of the restoration used to treat the small cavitation will allow to have a cleanable restorative margin which will be accessible through the various oral hygiene measures [32].
Pulpal sensibility
The signs and symptoms of acute cariogenic tissue tend to resolve if the carious lesion is sealed by a restoration after proper excavation. This shifts the balance away from the bacterial invaders affecting the pulp towards the restorative material which further heals the dentinal pulp complex [33].
Patient’s caries susceptibility
An adequately restored tooth will not have a good prognosis if the generalized carious susceptibility of the oral cavity is high. An adequately motivated patient towards the proper oral hygiene measures will have greater chance to keep the oral cavity in a disease-free state and ensures long term survival of the restoration. However, it must be kept in mind that all restorations placed in unsuitable high-risk oral environments will always be compromised to a significant clinical degree. The restorative procedures cannot cure the dental caries on their own [34].
Clinical factors
Ability to remove the infected dentine through various means depends on a lot of factors. Adequately controlled moisture control environment is needed, so that the dentine is sealed completely beneath the restoration, this can be done using rubber dam isolation [35]. Appreciation of final margin of cavity must be done as adequate oral hygiene measures would change according to location of margin, if its supragingival or subgingival. Appropriate manipulation of the restorative material as set by the manufacturer so that the restorative material reaches its maximal potential while maintaining the correct powder liquid ratio [36].
Adequately skilled and experienced operator for such procedures is also required to offer a better prognostic outcome. While performing the procedures of minimally invasive carious tissue removal it has been found that frequent recall of the patient and monitoring the tooth structure regularly, while giving oral health care instructions to the patient plays a significant role in longevity of the restoration and maximizes the life of the tooth [37].
An adequately restored tooth will not have a good prognosis if the generalized carious susceptibility of the oral cavity is high. An adequately motivated patient towards the proper oral hygiene measures will have greater chance to keep the oral cavity in a disease-free state and ensures long term survival of the restoration. However, it must be kept in mind that all restorations placed in unsuitable high-risk oral environments will always be compromised to a significant clinical degree. The restorative procedures cannot cure the dental caries on their own [38] (Figure 2).
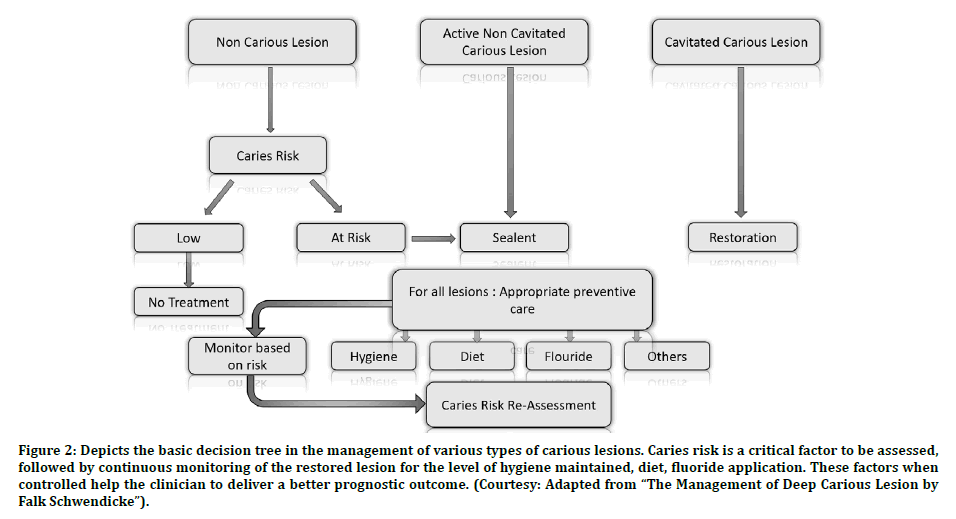
Figure 2: Depicts the basic decision tree in the management of various types of carious lesions. Caries risk is a critical factor to be assessed, followed by continuous monitoring of the restored lesion for the level of hygiene maintained, diet, fluoride application. These factors when controlled help the clinician to deliver a better prognostic outcome. (Courtesy: Adapted from “The Management of Deep Carious Lesion by Falk Schwendicke”).
In the modern approach the application of a liner or base beneath the restoration is not advocated except in cases where there is direct pulpal proximity of the lesion. In such cases GIC liner or calcium silicate cement is used beneath the restoration to protect the pulp tissue. In cases of direct pulpal exposure where the lesion is small, the application of Calcium Hydroxide or bioactive Calcium Silicate cements are used [39].
These materials are not self-sufficient as they are affected by etching procedures done while performing the placement of final restoration, so in these cases these materials should be protected by use of GIC above it followed by final restoration.
While removing the carious tissue, it’s imperative to assess the tooth radiographically, so that the remaining dentine thickness [40] can be assessed. In order to accomplish better salability of the restoration the cavity margin should extend on sound enamel or sound dentine structure even if a little extra healthy tooth tissue has to removed, as once the adequate sealing of the restoration has taken place the further bacterial ingress [41] through the saliva will be stopped and the preexisting bacteria beneath the restoration will die as the nutrient supply would be cut off [42].
How to selectively remove carious tissue
This part of the article discusses the clinical tools methods available to remove the deeper carious lesion. As can be seen from Table below, there are several Tooth-cutting/carious tissue removal technologies, the substrates acted upon and their mechanism of action.
Clinical technologies available for removing carious dentin and preparing teeth
Clinicians of the dental field get optimal training at the dental school for using dental burs in slow speed and get the skill to use air turbine operated handpieces. Additionally, the skill of spoon excavation is also learned. A careful combination of these varied skills can be extremely beneficial for the better prognostic outcome of the tooth which have deep carious lesion by aiding in removal of carious infected soft dentine. Recently slow speed polymer burs [43] are being used in order to remove the carious dentine , these burs have intrinsic hardness equivalent to that of carious dentine, because of this phenomenon the deeper layers of the dentine are prevented from aggressive cutting action.
Modern research focuses on the use of Bio-Bur [44] which are burs coated with ions/particles. These burs selectively remove the irreversibly damaged necrotic tissue. Also, these burs act as a carrier to direct bio-active/interactive healing chemistry for the tissues at need. Ultrasonic and sonic instrumentation [45] use principle of probe tip oscillation with the mechanism of implosion to dissociate the dental hard tissues. Laser involves the use of high energy water-based photo ablation of hard tissues. Laser involves stricter control while removing the carious lesion. The challenges being expensive cost and inability to selectively remove dentine. Other chemically based cavity disinfection methods include photo-activated disinfection (PAD) [46] where tolonium chloride is introduced into the cavity, absorbed by the residual bacteria in the cavity walls and then this chemical is activated using light of a specific wavelength causing cell lysis and death, and ozone treatment of caries [47] (gaseous ozone infused into lesions causing bacterial death).
Air-abrasion
Air abrasion (Table 1) is a seven-decade old dental operative technique used for removal of enamel and dentine during cavity preparation, that predates the air turbine handpiece. Air abrasion works on principle of minimally invasive tooth preparation using aluminum oxide. The major drawback using these systems is that they do not provide the operator a sense of tactile feedback, resistance and fail to provide appropriate fine cutting depth as compared to modern dental technology. The air abrasion technology is highly operator sensitive, so it makes the removal of the carious lesion approaching the pulp highly challenging. Other studies have shown that the air abrasion has specific operating parameters which are set by the clinician like air pressure, powder flow rate, reservoir volume, and nozzle diameter and working distance. It has been reported that the air abrasion has good patient acceptance. The reason for good patient acceptance is lack of vibration, no release of heat, and reduced need for local anesthesia [48].
| Mechanism | Substrate affected | Tooth-cutting technology |
|---|---|---|
| Mechanical, rotary | Sound or carious enamel and dentin | SS, CS, diamond, TC and plastic burs a |
| Mechanical, non-rotary | Sound or carious enamel and dentin | Hand instruments (excavators, chisels), Air-abrasion b, air-polishing c, ultrasonics, sono-abrasion |
| Chemomechanical | Carious dentin | Caridex™, Carisolv™ gel (amino acid based), Papacarie® gel (papain-based), pepsin-based solutions/gels |
| Photo-ablation | Sound or carious enamel and dentin | Lasers |
| Others | Bacteria | Photo-active disinfection (PAD), ozone |
| SS stainless steel, CS carbon steel, TC tungsten carbide | ||
| aWorks only on carious dentin | ||
| bAlumina powder, non-selective; bioactive glass powder, selective for carious enamel | ||
| cSodium bicarbonate used for stain removal. | ||
Table 1: Modern Tooth Cutting/Carious Removal Technologies (Courtesy: Adapted from the management of deep carious lesion by Falk Schwendicke).
The advantage of air abrasion technology is that the micro abrasive roughened enamel surface formed after air abrasion is devoid of weak enamel prisms and therefore the adhesive bonding of the overlying restoration takes place efficiently. The disadvantage being that lack of difference between the speeds of device while removing and enamel or dentine compounded with lack of tactile sensitivity often over removes the tooth structure. The innovation in the air abrasive technology is addition of a water shrouded air abrasion system that reduces the dust contamination in the dental operatory.
The other ones being the recent innovative product called as the Bioglass powder which is used in conjunction with air abrasion system. Bioglass powder is bioactive glass powder used to remove extrinsic enamel stain, desensitize exposed dentine. This Bioglass powder has an intrinsic selectivity towards the demineralised enamel and composite restoration. It has also been found that this technology has favorable outcome while managing white spot lesion as it helps to remineralise these lesions [49]. Other powders used with air abrasion systems are sodium bicarbonate and glycerine derivatives.
Chemomechanical carious tissue removal
Chemo mechanical solutions help in breakdown of collagen already softened by carious process. The chemomechanical solutions (include hypochlorite, chloramines, enzymatic pepsin, and papain).
Initially Caridex system [50] was formulated in 1970s but due to its very slow onset of action and longer treatment time the Carisolv System (Table 1) was formulated in late 1990s. This hypochlorite/amino acid-based gel system is used with special non-cutting hand instruments. This system provides greater tactile sensitivity to the operator, so permitting selective dentin removal. The average time for the Carisolv system [51] to act is approximately five minutes which has good patient acceptance. This time duration is approximately equivalent to that taken by the rotary cutting instruments. The Carisolv gel has papain-based gel which is fabricated in laboratory, specifically designed nylon brushes, and plastic disposable hand instruments that help in caries excavation (Figure 3).
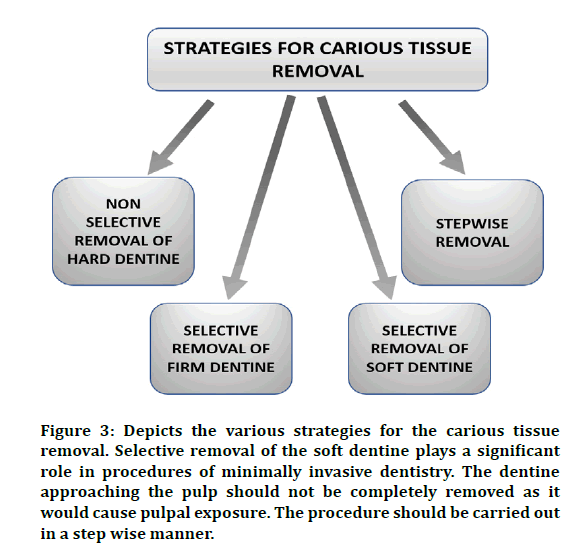
Figure 3: Depicts the various strategies for the carious tissue removal. Selective removal of the soft dentine plays a significant role in procedures of minimally invasive dentistry. The dentine approaching the pulp should not be completely removed as it would cause pulpal exposure. The procedure should be carried out in a step wise manner.
Conclusion
Sufficient evidence exists according to the review of literature about the clinical and scientific evidence for tissue removal in cavitated lesions. In cavity lesions which are not deep, the restorative material prolongs the life of the tooth structure. In the carious lesions that are deep, the extent of removal is governed using minimally invasive approach that prolong the longevity of the pulp. The preservation of the coronal tooth tissue which is not highly infected is critical to enhance the longevity of tooth structure.
The complete removal of infected soft carious dentine is of greater importance to increase the life of tooth, except in cases that are deeply carious and could lead to pulpal exposure. The assessment of such tooth should be done by though clinical examination, pulpal vitality assessment of inflammatory response and ability of the restorative material that it may seal the cavity margins at the periphery completely. The peripheral removal of the lesion should extend till sound dentine is reached, in such cases inadequate enamel margins may be found. It is at this tooth restoration interface that peripheral seal is achieved and prevents histological spread of caries. Modern biomaterials offer adequate seal as they can penetrate micromechanically into mineral and collagenous components of the enamel and dentine, respectively. The contemporary adhesives involving such impermeable seal also provide bactericidal and insulating properties. As these are very efficient materials a need of separate insulating base is not required these days. A thorough and in-depth knowledge of modern materials is restorative dentistry is critical for dealing with such kinds of variable carious lesions. Patient Co-operation is of great concern as long term prognosis of the restoration depends on the patient's motivation to perform the oral hygiene procedures meticulously.
References
- Rosan B, Lamont RJ. Dental plaque formation. Microbes Infection 2000; 2:1599–1607.
- https://patentimages.storage.googleapis.com/d5/7e/8b/b73d55e81b93e4/US5549476.pdf
- Murdoch-Kinch CA, McLean ME. Minimally invasive dentistry. J Am Dent Assoc 2003; 134:87–95.
- Jokstad A, Mjör IA. Cavity designs for class II amalgam restorations. A literature review and a suggested system for evaluation. Acta odontologica Scandinavica 1987; 45:257–273.
- Alghaithy RA, Qualtrough AJE. (2017) Pulp sensibility and vitality tests for diagnosing pulpal health in permanent teeth: A critical review. Int Endodont J 2017; 50135–142.
- Aminzade A, Aminzadeh A, Khosravi, K. (2002) Infra-red and Raman spectroscopic studies of infected and affected dentine. Iranian J Chem CHEM Engineer 2002; 21:87-90.
- Qi YP, Li N, Niu LN, et al. Remineralization of artificial dentinal caries lesions by biomimetically modified mineral trioxide aggregate. Acta Biomaterialia 2012; 8:836–842.
- Rivera EM, Yamauchi M. Site comparisons of dentine collagen cross-links from extracted human teeth. Archives of Oral Biol 1993; 38:541–546.
- Nakabayashi N, Takeyama M, Kojima K, et al. Studies on dental self-curing resins (20)-adhesion mechanism of 4-META/MMA-TBB resin to dentine. J Japan Society Dent Apparatus Materials 1982; 23:34–39.
- Demarco FF, Matos AB, Matson E, et al. Dyes for caries detection influence sound dentin bond strength. Operative Dent 1998; 23: 294–298.
- Govindaraju L, Neelakantan P, Gutmann JL. Effect of root canal irrigating solutions on the compressive strength of tricalcium silicate cements. Clin Oral Investigations 2017; 21(2), pp. 567–571.
- Azeem RA, Sureshbabu NM. Clinical performance of direct versus indirect composite restorations in posterior teeth: A systematic review. J Conservative Dent 2018; 21:2–9.
- Jenarthanan S, Subbarao C. Comparative evaluation of the efficacy of diclofenac sodium administered using different delivery routes in the management of endodontic pain: A randomized controlled clinical trial. J Conservative Dent 2018; 21:297–301.
- Manohar MP, Sharma S. A survey of the knowledge, attitude, and awareness about the principal choice of intracanal medicaments among the general dental practitioners and nonendodontic specialists. Indian J Dent Res 2018; 29:716–720.
- Nandakumar M, Nasim I. Comparative evaluation of grape seed and cranberry extracts in preventing enamel erosion: An optical emission spectrometric analysis. J Conservative Dent 2018; 21:516–520.
- Teja KV, Ramesh S, Priya V. Regulation of matrix metalloproteinase-3 gene expression in inflammation: A molecular study. J Conservative Dent 2018; 21:592–596.
- Janani K, Sandhya R. A survey on skills for cone beam computed tomography interpretation among endodontists for endodontic treatment procedure’, Indian journal of dental research: Official publication of Indian Society for Dental Research 2019; 30:834–838.
- Khandelwal A, Palanivelu A. Correlation between dental caries and salivary albumin in adult population in Chennai: An In Vivo study Brazilian Dent Sci 2019; 22:228–233.
- Malli Sureshbabu N, Selvarasu K, Nandakumar M, et al. Concentrated growth factors as an ingenious biomaterial in regeneration of bony defects after periapical surgery: A report of two cases. Case Reports Dent 2019; 7046203.
- Poorni S, Srinivasan MR, Nivedhitha MS. Probiotic strains in caries prevention: A systematic review. J Conservative Dentistry 2019; 22:123–128.
- Rajakeerthi R, Ms N. Natural Product as the Storage medium for an avulsed tooth–A Systematic Review. Cumhuriyet Dent J 2019; 22:249–256.
- Rajendran R, Kunjusankaran RN, Sandhya R, et al. Comparative evaluation of remineralizing potential of a paste containing bioactive glass and a topical cream containing casein phosphopeptide-Amorphous calcium phosphate: An in Vitro Study. Pesquisa Brasileira Odontopediatria Clinica Integrada 2019; 19:1–10.
- Ramarao S, Sathyanarayanan U. CRA Grid-A preliminary development and calibration of a paper-based objectivization of caries risk assessment in undergraduate dental education. J Conservative Dent 2019; 22:185–190.
- Siddique R, Nivedhitha MS. Effectiveness of rotary and reciprocating systems on microbial reduction: A systematic review. J Conservative Dent 2019; 22:114–122.
- Siddique R, Sureshbabu NM, Somasundaram J, et al. Qualitative and quantitative analysis of precipitate formation following interaction of chlorhexidine with sodium hypochlorite, neem, and tulsi. J Conservative Dent 2019; 22:40–47.
- Siddique R, Nivedhitha MS, Jacob B. Quantitative analysis for detection of toxic elements in various irrigants, their combination (precipitate), and para-chloroaniline: An inductively coupled plasma mass spectrometry study. J Conservative Dent 2019; 22:344–350.
- Zander HA. Reaction of the pulp to calcium hydroxide. J Dent Res 1939; 18(4), pp. 373–379.
- Meraji N, Nekoofar MH, Yazdi KA, et al. Bonding to caries affected dentine. Dent Materials 2018; 34:e236–e245.
- Vazquez-Garcia F, Tanomaru-Filho M, Chávez-Andrade GM, et al. Effect of silver nanoparticles on physicochemical and antibacterial properties of calcium silicate cements. Brazilian Dental J 2016; 27:508–514.
- Duque C, de Cássia Negrini T, Sacono NT, et al. Clinical and microbiological performance of resin-modified glass-ionomer liners after incomplete dentine caries removal. Clin Oral Investigations 2009; 13:465–471.
- Christensen GJ. The advantages of minimally invasive dentistry. J Am Dent Assoc 2005; 136:1563–1565.
- White JM, Eakle WS. Rationale and treatment approach in minimally invasive dentistry. J Am Dent Assoc 2000; 131:13–19.
- Jafarzadeh H, Abbott PV. Review of pulp sensibility tests. Part I: general information and thermal tests. Int Endodont J 2010; 43:738–762.
- Ripa LW, Leske GS, Varma AO. Longitudinal study of the caries susceptibility of occlusal and proximal surfaces of first permanent molars. J Public Health Dent 1988; 48:8–13.
- Knight GT, Berry TC, Barghi N, et al. Effects of two methods of moisture control on marginal microleakage between resin composite and etched enamel: a clinical study. Int J Prosthodont 1993; 6:475–479.
- Voruganti K. Dental materials: Properties and manipulation. Br Dent J Nature Publishing Group 2008; 204:160–160.
- Andlaw RJ. Oral hygiene and dental caries-A review. Int Dent J 1978; 28:1–6.
- Twetman S, Fontana M. Patient caries risk assessment. Monographs Oral Sci 2009; 21:91–101.
- Weiner R. Liners and bases in general dentistry Australian Dental J 2011; 56:11–22.
- Murray PE, Smith AJ, Windsor LJ, et al. Remaining dentine thickness and human pulp responses. Int Endodont J 2003; 36:33–43.
- Friedman S, Komorowski R, Maillet W, et al. In vivo resistance of coronally induced bacterial ingress by an experimental glass ionomer cement root canal sealer. J Endodont 2000; 26:1–5.
- Pinna R, Maioli M, Eramo S, et al. Carious affected dentine: its behaviour in adhesive bonding. Australian Dent J 2015; 60:276–293.
- Prabhakar A, Kiran NK. Clinical evaluation of polyamide polymer burs for selective carious dentin removal. J Contemporary Dent Practice 2009; 10:26–34.
- Schwendicke F, Innes N. Removal strategies for carious tissues in deep lesions. Management Deep Carious Lesions 2018; 15–35.
- Banerjee A, Watson TF, Kidd EA. Dentine caries excavation: a review of current clinical techniques. Br Dent J2000; 188:476–482.
- Deepak BS, Mallikarjun Goud K, Nishanth P. Photo activated disinfection in Restorative Dentistry: A technical review. J Dent 2014; 16–18.
- Burke FJT. Ozone and caries: A review of the literature. Dent Update 2012; 271–278.
- Banerjee A, Watson TF. Air Abrasion: Its uses and abuses. Dent Update 2002; 29:340–346.
- Farooq I, Tylkowski M, Müller S, et al. Influence of sodium content on the properties of bioactive glasses for use in air abrasion. Biomed Materials 2013; 8:065008.
- Beeley JA, Yip HK, Stevenson AG. Chemochemical caries removal: a review of the techniques and latest developments. Br Dent J 2000; 188:427–430.
- Hamama HH, Yiu CK, Burrow MF, et al. Systematic review and meta-analysis of randomized clinical trials on chemomechanical caries removal. Operative Dent 2015; 40:167–178.
Author Info
Shree Ranjan Pandey and Nivedhitha MS*
Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Science, Saveetha University, Chennai, IndiaCitation: Shree Ranjan Pandey, Nivedhitha MS, Decision Tree Analysis on Management of Deep Carious Lesion, J Res Med Dent Sci, 2020, 8 (7): 64-71.
Received: 23-Sep-2020 Accepted: 14-Oct-2020 Published: 21-Oct-2020
