Research - (2021) Volume 9, Issue 1
Dentists Education, Knowledge and Attitudes towards Silver Diamine Fluoride
Saud Ismail Asirri6, Reem H Alsareay7, Raed Abdullah Alamri2, Abdulrahman Yahya Almalki9, Shaker Saad Alshaflot2, Saeed J Alqahtani2, Alanoud M Alazmi8, Mona A Asiri7, Ebtsam M Alshehri2, Elham Ali Abusarhad2, M Zakirulla1*, Mzoon A Rashad6, Sami Mohammed Alawwadh2, Abdulhadi M Alqahtani5, Abeer A Alghothimy5, Albatool Mohammed Alqahtani4, Thamra M Alqahtani3, Hassan I Asiri2 and Ahmed Ali Althuqbi2
*Correspondence: M Zakirulla, Assistant professor, Department of Pediatric Dentistry and Orthodontic Sciences, College of Dentistry, King Khalid university, Saudi Arabia, Tel: +966530518766, Email:
Abstract
Background: This study aims to evaluate the knowledge and attitude among dentists towards Silver Diamine Fluoride (SDF).
Materials & Methods: A cross-sectional study was carried out on the sample size of 101 dental surgeons participated in the study. Written informed consent was obtained from the participants after explaining to them the purpose of the study. The sampling method included in the study is a simple random sampling method. A self-administered structured questionnaire was developed, and the data was collected. Both descriptive and analytical statistical measurements were done.
Results: Most participants, 59 (58%) were said that they did not hear about SDF application in dentistry. 28% agreed that they attended lectures/discussions about SDF. When asked about the participant's source of knowledge about SDF, the primary source of information is from the online internet (32%), followed by academic teaching (25%). However, most participants (31%) agreed to the point that SDF is applied mainly to primary dentition, followed by permanent dentition (21%). When asked about the type of teeth used for SDF, 13% and 27% of participants were agreed to use in anterior teeth and posterior teeth, respectively.
Conclusions: Education and understanding of SDF through their expert development activities. Increasing SDF educational attempts might therefore bring about greater usage of this innovative method of managing cavitated caries lesions, especially in children.
Keywords
Prevention, Silver diamine fluoride, Dental caries, Cariostatic agents, Dentists, Surveys, Questionnaires
Introduction
The prevalence of early childhood caries continues to be saturated in disadvantaged Communities. Standard restorative therapy may neglect to decrease early childhood caries in lots of parts of the world. The most decayed tooth in pre-school kids remained unrestored, specifically within underprivileged communities. The usage of silver diamine fluoride (SDF) has acquired interest because of its usefulness in arresting caries. Medical trials of SDF demonstrated favorable outcomes in arresting dental care caries in pre-school kids. Systematic reviews figured the use of SDF could be a therapeutic choice for caries administration at the cavitation degree among pre-school children, especially people that have poor access to dental hygiene [1]. The side effect of SDF in blackening carious lesions is really a concern, most likely affecting patient's acceptability. Usage of dental hygiene services is markedly reduced among people who have low incomes, low schooling levels, and surviving in rural areas [2]. Additionally, it is difficult for people who have special needs and small children [3]. Dental caries may be the most typical oral disease globally, affecting 60-90% of school children and nearly 100% of adults, often resulting in pain and discomfort [4]. In accordance with new global teeth's health objectives [5], the arrest of oral caries, without using dental care restoration, might meet up with the dependence on the cost-effective, simpleness of execution, and marked advantages. Silver diamine fluoride (SDF) satisfies these needs and may enhance accessibility to teeth's health treatment because it is really a low-price, topical medicament, easily relevant, and found in many nations to arrest oral caries [6].
Previous studies about SDF have concentrated primarily on its medical efficacy [7,8]. Using SDF at 38% concentration has been impressive inside the arrest and prevention of carious lesions [9]. SDF contains silver ions that become antimicrobial and bactericidal brokers within lesions by destroying bacterial membranes, denaturing proteins, and inhibiting DNA replication [10]. The fluoride ions in SDF help create fluorapatite, a far more acidresistant enamel that may prevent additional demineralization of tooth structure. Applying SDF to occlusal, facial, and lingual areas has been shown to reach your goals in arresting caries in multiple clinical trials [7,9]. While an individual application of SDF seems insufficient for sustained results, annual and semi-annual re-applications have already been shown to be highly effective. SDF treatment could be a promising technique to manage dental care caries in small children and those who've unique needs. Geriatric individuals with higher anxiety or specific needs, along with other patient populations may possibly also benefit significantly from its software [11,12]. Considering public health, SDF may become a significant tool in the administration of caries lesions, avoiding discomfort and pain, either used as the definitive or temporary therapy, mainly in places where the demand is fantastic, with lengthy queues of waiting. This study aims to evaluate the knowledge and attitude among dentists towards Silver Diamine Fluoride.
Materials and Methods
The current study was a cross-sectional survey. The sample included was 101 (74 males and 27 females) dental students, general dentists, and specialists in the College of Dentistry King Khalid University, Abha, Saudi Arabia. Online informed consent was obtained from the participants, and the questionnaire form after explaining to them the purpose of the study. The sampling method included was a simple random sampling method. A self-administered questionnaire was designed to evaluate the knowledge and attitude among dentists towards Silver Diamine Fluoride. Data was collected through an online survey form to avoid direct interaction with the participants and to prevent cross-contamination in this COVID pandemic situation. Ethical approval for performing the survey was obtained from the Institutional review board (IRB/KKUCOD/ ETC/2019-20/070) of College of Dentistry King Khalid University.
The questionnaire was formulated and comprised of two parts: The first portion includes the questions related to the demographic information of participants, such as age, sex, and educational level (Student, dentists, specialists). The other part of the questionnaire comprised 11 questions with the multiple-choice question was prepared, and piloting was done to obtain information about knowledge and attitude among dentists towards Silver Diamine Fluoride.
A self-administered structured questionnaire was developed and tested among a convenience sample of 10 patients, who were interviewed to gain feedback on the overall acceptability of the questionnaire in terms of length and language clarity; according to their feedback, the questions were corrected. Face validity was also be assessed before the start of the study. Both descriptive and analytical statistical measurements were used to describe the main variables by SPSS 18 (IBM Corporation, Armonk, New York, USA) software.
Results
A total of 101 (74 males and 27 females) dental students, general dentists, and specialists responded to the questionnaire. 93% of study subjects were of 20-30 years, 6% were of 31- 40 years, 1% were of 41-50 years, and 0% were >50 years (Table 1). The distribution of study samples according to a level of education was shown in Table 1. Knowledge and attitude among dentists towards Silver Diamine Fluoride were shown in Table 2.
| Gender | n (101) | % |
|---|---|---|
| Male | 74 | 73.30% |
| Female | 27 | 26.70% |
| Age | ||
| 20-30 years | 94 | 93.10% |
| 30-40 years | 6 | 5.90% |
| 40-50 years | 1 | 1% |
| >50 years | 0 | 0% |
| Education level | ||
| Undergraduate student | 52 | 51.50% |
| General dentist | 45 | 44.60% |
| Specialist | 4 | 3.90% |
| n=Number; %=Percentage | ||
Table 1: Distribution of study sample according to age, gender, and level of education.
| Questions | Males (n)-74 | % | Females (n)-27 | % | Total (n)-101 | % |
|---|---|---|---|---|---|---|
| Q1. Heard about Silver Diamine Fluoride (SDF) Application in dentistry? | ||||||
| Yes | 25 | 33.80% | 17 | 62.96% | 42 | 41.58% |
| No | 49 | 66.20% | 10 | 37.04% | 59 | 58.42% |
| Q2. Attended lectures/discussions about Silver Diamine Fluoride (SDF)? | ||||||
| Yes | 22 | 29.70% | 7 | 25.90% | 29 | 28.70% |
| No | 52 | 70.30% | 20 | 74.10% | 72 | 71.30% |
| Q3. Type of lesion is SDF is used for? | ||||||
| Enamel Lesion | 27 | 36.50% | 10 | 37% | 37 | 36.63% |
| Dentin Lesion | 6 | 8.10% | 2 | 7.40% | 8 | 7.92% |
| Both Enamel and Dentin Lesion | 25 | 33.80% | 15 | 55.60% | 40 | 39.61% |
| With or without lesion | 16 | 21.60% | 0 | 0% | 16 | 15.84% |
| Q4. Type of teeth used for SDF application? | ||||||
| Anterior | 11 | 14.90% | 2 | 7.40% | 13 | 12.90% |
| Posterior | 22 | 29.70% | 5 | 18.50% | 27 | 26.70% |
| Both | 41 | 55.40% | 20 | 74.10% | 61 | 60.40% |
| Q5. It is an alternative to removing tooth structure by a dental drill in order to place restorative material | ||||||
| Agree | 34 | 45.95% | 14 | 51.90% | 48 | 47.50% |
| Disagree | 10 | 13.51% | 4 | 14.80% | 14 | 13.90% |
| Don’t know | 30 | 40.54% | 9 | 33.30% | 39 | 38.60% |
| Q6. Many patients (or parents of patients) would not accept treatment of dental caries with SDF due to the permanent black staining of the carious lesion. | ||||||
| Agree | 31 | 41.90% | 9 | 33.30% | 40 | 39.60% |
| Disagree | 9 | 21.20% | 4 | 14.80% | 13 | 12.90% |
| Don’t know | 34 | 45.90% | 14 | 51.90% | 48 | 47.50% |
| Q7. SDF does not require the use of local anesthesia | ||||||
| Agree | 33 | 44.60% | 16 | 59.30% | 49 | 48.50% |
| Disagree | 13 | 17.60% | 2 | 7.40% | 15 | 14.90% |
| Don’t know | 28 | 37.80% | 9 | 33.30% | 37 | 36.60% |
| Q8. Possible Barriers to the Use of SDF | ||||||
| Scientific knowledge | 35 | 47.30% | 13 | 48.10% | 48 | 47.50% |
| Inadequate training | 26 | 35.10% | 10 | 37% | 36 | 35.60% |
| Cost | 29 | 39.20% | 5 | 18.50% | 34 | 33.70% |
| The Tooth-staining | 35 | 47.30% | 14 | 51.60% | 49 | 48.50% |
| Patient acceptance | 28 | 37.80% | 16 | 59.30% | 44 | 43.60% |
| Does not restore shape and function | 16 | 21.60% | 6 | 22.20% | 22 | 21.80% |
| Does not arrest caries | 11 | 14.90% | 3 | 11.10% | 14 | 13.90% |
| Q9. Application protocol interval for SDF | ||||||
| A single application | 17 | 22.97% | 7 | 25.90% | 24 | 23.80% |
| 6-month reapplication | 12 | 16.22% | 5 | 18.50% | 17 | 16.80% |
| Annual reapplication | 9 | 12.16% | 1 | 3.70% | 10 | 9.90% |
| 4 weekly Application | 4 | 5.41% | 0 | 0% | 4 | 3.96% |
| Don’t know | 32 | 43.24% | 14 | 51.90% | 46 | 45.54% |
| n=Number; %=Percentage | ||||||
Table 2: Knowledge of dentists towards silver diamine fluoride (SDF).
Most participants, 59 (58%) were said that they did not hear about SDF application in dentistry. 28% agreed that they attended lectures/ discussions about SDF. When asked about the participant's source of knowledge about SDF (Figure 1), the primary source of information is from the online internet (32%), followed by academic teaching (25%). However, most participants (31%) agreed to the point that SDF is applied mainly to primary dentition, followed by permanent dentition (21%) (Figure 2). When asked about the type of teeth used for SDF, 13% and 27% of participants were agreed to use anterior teeth and posterior teeth, respectively. Nearly half of the participants agreed that SDF is an alternative to removing tooth structure by a dental drill to place restorative material. 40% agreed that the main reason for many patients would not accept the treatment of dental caries with SDF was causing permanent black staining of the carious lesion. The main barriers reported to the use of SDF among those that did not use it was a tooth staining (49%), followed by scientific knowledge (48%). Unfortunately, nearly half of the participants (45%) said that they do not know regarding the application protocol interval for SDF, followed by only 24% who said that it's a single application of SDF.
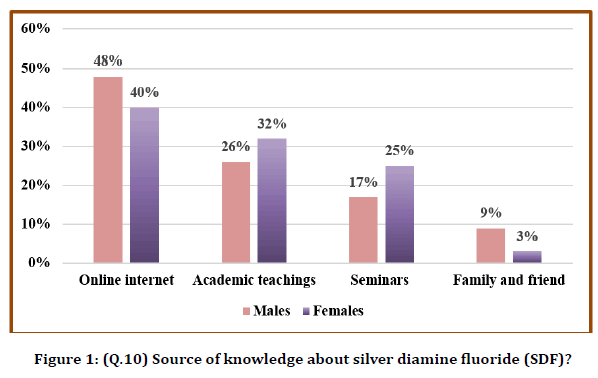
Figure 1. (Q.10) Source of knowledge about silver diamine fluoride (SDF)?
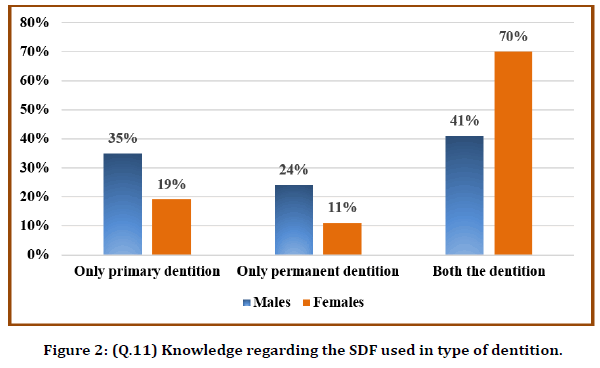
Figure 2. (Q.11) Knowledge regarding the SDF used in type of dentition.
Discussion
SDF is a topically applied liquid that is utilized to take care of tooth hypersensitivity and arrest cavitated carious lesions [13]. Lesion arrest may be accomplished by painting the cavitated lesion with the SDF liquid without eliminating any infected soft dentin [14]. SDF can serve alternatively, particularly for individuals who cannot tolerate traditional dental care, and can decrease the need for dental hygiene to be executed under general anesthesia, using its related health threats [15]. Pertaining to the mechanism of action, silver particles act on proteins, making sure the antibacterial activity of SDF [16]. Regardless of antimicrobial effectiveness, silver contaminants, however, have the effect of causing blackening of carious enamel and dentin. It is an issue since this adverse impact may affect the sufferers' acceptability and become a substantial impediment to the usage of SDF. Indeed, a study of directors of pediatric residency programs in the USA found that bad parental acceptance was probably the most frequently reported barrier to utilize SDF [17].
The safety of making use of silver fluoride solution in pre-school kids had once been doubted, and the large fluoride concentration was the primary concern.18 Up to now, no severe side-effect has been reported [18]. It has been predicted that each application of 38% SDF solution only consists of 0.2 mg fluoride, which is far under the probably toxic dosage of 5 mg/kg. The SDF panel of the American Academy of Pediatric Dentistry (AAPD) backs using 38% SDF in arresting the cavitated caries lesions of primary teeth for the extensive caries management program as a conditional suggestion with low-quality evidence [19].
Chibinski et al. in a systematic evaluation, showed that SDF would be 89% far better than other alternative remedies or placebo in arresting dental care caries in primary dentition [20]. The experts discovered that 38% of SDF application is most reliable in comparison to a no-treatment (unfavorable control) or perhaps a placebo in the principal tooth for arresting dentine caries. Over half of the participants agreed that lots of children would not usually accept treating dental caries with SDF because of the permanent dark staining of the carious lesion. This can be an assumption by participants who believe that individuals are usually biased by the significance of esthetic appearance. Tesoriero's research was performed in New York, where most of the mother and father were more comfortable with SDF therapy on a posterior tooth, however, not on an anterior tooth [21].
Nevertheless, one barrier to SDF make use of will be that it discolors the dental caries lesion black. Furthermore, Yee et al. discovered that the portion of arrested cavitated lesions reduced over an interval of two years following a single initial program, recommending that re-application is essential as time passes [22]. Applying SDF twice yearly has been proven to be somewhat far better than once annually. When used two times per year, the 38% SDF solution had the successful price of 84.8% for arresting caries. Furthermore, there appears to be a dose-reaction to the potency of SDF, with a 38% SDF solution being far better when compared to a 12% SDF solution [22]. Regarding recommendations for the frequency of SDF applications, some authors used the solution annually, among others sixmonthly. The use of a 38% SDF solution is an easy and low-cost technique that does not need the cooperation of the children or the complex coaching of medical specialists. This approach could be of excellent utility instead of more costly preventive strategies in communities with restricted resources.
Research involving pediatric dentistry residency program directors discovered that noncompliant patients were good candidates for therapy with SDF [17]. Besides that, nearly all participants disagreed that SDF ought to be found in permanent teeth in comparison with primary teeth. This is often explained by the truth that SDF darkens the tooth, which is better to recognize in a short-term tooth, and since there is proof that SDF works more effectively in the primary tooth than permanent teeth [23]. Interestingly, although lesions within posterior teeth experienced a lower potential for getting arrested than anterior teeth [4], a lot more than one-third of the participants inside our survey reported the usage of SDF limited to posterior teeth, and 5.6% used it limited to anterior teeth. It might be related to the truth that dentists nevertheless possess prejudice to the usage of SDF in anterior teeth due to aesthetic, and to higher acceptability of the parents to the use of SDF in the posterior tooth to the prior ones [24].
Conclusion
Education and understanding of SDF through their expert development activities, with more knowledge they will use SDF within their clinical practice. Increasing SDF educational attempts might bring about more significant usage of this innovative method of managing cavitated caries lesions, especially in children. The mostcited barrier to utilize of SDF was tooth staining connected with caries arrest.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Wilson TG. Silver diamine fluoride receives new FDA designation. Decisions Dent 2016; 2:10.
- Yee R, Holmgren C, Mulder J, et al. Efficacy of silver diamine fluoride for arresting caries treatment. J Dent Res 2009; 88:644-647.
- Mattos-Silveira J, Floriano I, Ferreira F, et al. Children's discomfort may vary among different treatments for initial approximal caries lesions: preliminary randomized controlled clinical trial. Int J Clin Pediatr Dent 2015; 25:300-304.
- Zhi QH, Lo ECM, Lin HC. Randomized clinical trial on effectiveness of silver diamine fluoride and glass ionomer in arresting dentine caries in pre-school children. J Dent 2012; 40:962-967.
- Tan HP, Lo ECM, Dyson JE, et al. A randomized trial on root caries prevention in elders. J Dent Res 2010; 89:1086-1090.
- Dos Santos VE, de Vasconcelos FM, Ribeiro AG, et al. Paradigm shift in the effective treatment of caries in schoolchildren at risk. Int J Dent 2012; 62:47-51.
- Chu CH, Lo ECM, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res 2002; 81:767-770.
- Yee R, Holmgren C, Mulder J, et al. Efficacy of silver diamine fluoride for arresting caries treatment. J Dent Res 2009; 88:644-647.
- Targino AG, Flores MA, dos Santos VE, et al. An innovative approach to treating dental decay in children. A new anti-caries agent. J Mater Sci Mater Med 2014; 25:2041-2047.
- Mei ML, Li QL, Chu CH, et al. The inhibitory effects of silver diamine fluoride at different concentrations on matrix metalloproteinases. Dent Mater 2012; 28:903-908.
- Quock RL, Patel SA, Falcao FA, et al. Is a drillless dental filling possible? Med Hypotheses 2011; 77:315-317.
- Clarkson BH, Exterkate RA. Non-invasive dentistry: A dream or reality? Caries Res 2015; 1:11-17.
- Gao SS, Zhao IS, Hiraishi N, et al. Clinical trials of silver diamine fluoride in arresting caries among children: A systematic review. Clin Trans Res 2016; 1:201-210.
- Chu CH, Lo ECM, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res 2002; 81:767-770.
- Nelson T, Scott JM, Crystal YO, et al. Silver diamine fluoride in pediatric dentistry training programs: survey of graduate program directors. Pediatr Dent 2016; 38:212-217.
- Mei ML, Lo ECM, Chu CH. Arresting dentine caries with silver diamine fluoride: What's behind it? J Dent Res 2018; 97:751-758.
- Nelson T, Scott JM, Crystal YO, et al. Silver diamine fluoride in pediatric dentistry training programs: survey of graduate program directors. Pediatr Dent 2016; 38:212‐217.
- Chu CH, Lo EC. Promoting caries arrest in children with silver diamine fluoride: A review. Oral Health Preventive Dentistry 2008; 6:315-321.
- Crystal YO, Marghalani AA, Ureles SD, et. al. use of silver diamine fluoride for dental caries management in children and adolescents, including those with special health care needs. Pediatr Dent 2017; 39:135–145.
- Chibinski AC, Wambier LM, Feltrin J, et al. Silver diamine fluoride has efficacy in controlling caries progression in primary teeth: A systematic review and meta-analysis. Caries Res 2017; 51:527–541.
- Tesoriero J, Lee A. Parental acceptance of silver diamine fluoride. Paper presented at: American Academy of Pediatric Dentistry Annual Session 2016.
- Yee R, Holmgren C, Mulder J, et al. Efficacy of silver diamine fluoride for arresting caries treatment. J Dent Res 2009; 88:644-647.
- Llodra JC, Rodriguez A, Ferrer B, et al. Efficacy of silver diamine fluoride for caries reduction in primary teeth and first permanent molars of schoolchildren: 36-month clinical trial. J Dent Res 2005; 84:721-724.
- Crystal YO, Janal MN, Hamilton DS, et al. Parental perceptions and acceptance of silver diamine fluoride staining. J Am Dent Assoc 2017; 148:510-518.
Author Info
Saud Ismail Asirri6, Reem H Alsareay7, Raed Abdullah Alamri2, Abdulrahman Yahya Almalki9, Shaker Saad Alshaflot2, Saeed J Alqahtani2, Alanoud M Alazmi8, Mona A Asiri7, Ebtsam M Alshehri2, Elham Ali Abusarhad2, M Zakirulla1*, Mzoon A Rashad6, Sami Mohammed Alawwadh2, Abdulhadi M Alqahtani5, Abeer A Alghothimy5, Albatool Mohammed Alqahtani4, Thamra M Alqahtani3, Hassan I Asiri2 and Ahmed Ali Althuqbi2
1Assistant professor, Department of Pediatric Dentistry and Orthodontic Sciences, College of Dentistry, King Khalid university, Abha, Saudi Arabia2Intern, College of Dentistry, King Khalid university, Abha, Saudi Arabia
3General Dentist, Private Dental Clinic, Abha, Saudi Arabia
4General Dentist, Ministry of Health, Muhayel Dental Center, Muhayel, Aseer, Saudi Arabia
5General Dentist, Abha Maternity Children Hospital, Abha, Saudi Arabia
6General Dentist, Ministry of Health, Bariq Health Center Abha, Saudi Arabia
7General Dentist, Ministry of Health, Albirk-Aseer, Saudi Arabia
8General Dentist, Ministry of Health, Najran, Saudi Arabia
9Department of Preventive Dental Sciences, Division of Pediatric Dentistry, Teaching Assistant at College of Dentistry, Jazan University, Jazan, Saudi Arabia
Citation: Meer Zakirulla, Ahmed Ali Althuqbi, Hassan Ibrahim Ahmed Asiri, Hussain Almubarak, Mohammed Ibrahim, Thamra Mohamed M Alqahtani, Hanin Mathkar Ali Al-Qahtani, Abeer A Alghothimy, Abdulhadi M Alqahtani, Mzoon Ali Mohammed Rashad, Saud Ismail Asirri, Abdulrahman Yahya Almalki, Elham Ali Abusarhad, Saeed J Alqahtani, Shaker Saad Alshaflot, Dentists' Education, Knowledge and Attitudes towards Silver Diamine Fluoride, J Res Med Dent Sci, 2021, 9 (1): 186-191.
Received: 01-Dec-2020 Accepted: 23-Dec-2020
