Research Article - (2022) Volume 10, Issue 10
Determination of the Level of Osteotomy of Radial Neck with Radial Tuberosity as a Most Reliable Reference Point in Radial Head Replacement
Mervinrosario PM*, Vijay Narasimman Reddy and Aravind Ravichandran
*Correspondence: Dr. Mervinrosario PM, Department of Orthopaedics, Sree Balaji Medical College and Hospital, Tamil Nadu, Chennai, India, Email:
Abstract
Aim: To determine the most reliable reference point for radial neck osteotomy in replacement surgery of radial head for unrepairable fractures of head and neck of radius.
Methods: A prospective analysis of 30 patients (16 men and 14 women, with mean age 35.3 years) with modified mason type 3 and 4 fractures treated with radial head replacement between August 2016 and July 2020 was performed. The radial neck was osteotomised at 2 mm above the radial tuberosity. The outcomes were studied based on Mayo Elbow Performance Index (MEPI), Range of Motion (ROM) and Visual Analog Scale (VAS).
Results: The mean MEPI, VAS and ROM at interval of 2 weeks, 6 weeks, 3 months, 6 months, 1 year and 3 years show significant improvement. The mean MEPI score at 3 years is 95 and VAS score is 8.8. The mean flexion is 115, pronation is 55 and supination is 75 at the end of 3 years.
Conclusion: Osteotomy performed at 2 mm proximal to radial tuberosity is associated with good clinical and functional outcomes in most cases. Hence the radial tuberosity is a reliable reference point in radial head replacement surgeries.
Keywords
Radial head replacement, Osteotomy of radial neck, Reference point, Prospective study
Introduction
Radial head fractures account for 20% of the elbow injuries [1]. Most cases are un-displaced, marginal fractures treated by immobilization. Of the displaced and comminuted fractures, the aim is to restore the native radial head and radiocapitellar contact. Reconstruction of radial head using screws or plates should always be attempted if possible. However in unrepairable fractures with unstable elbow, radial head replacement has been performed [2].
Radial head replacement since its inception by speed in 1941 has evolved in design, prosthetic material and techniques to resemble the native head of the radius [3]. Swanson introduced silicone implants which provided suboptimal stability. They were associated with poor outcomes [4]. Silicone implants became obsolete after the emergence of metallic implants in 1994 [5].
Metallic implants were either mono block or modular. Bipolar implants are also available that provides large radiocapitellar contact and decrease pressure across the joint [6].
Radial head is an important valgus stabilizer of elbow joint both in flexion and extension. In cases of associated injuries to coronoid, olecranon and collateral ligaments such as in fracture dislocation, the radial head is vital for the postero lateral stability of elbow [7].
Lengthening of the proximal radius by the prosthesis leads to overstuffing the joint and altered biomechanics and load transmission across the joint. Shortening may cause under stuffing and instability. Studies show that an increase or decrease of 2.5 mm of native radial head is associated with poor outcomes in a radial head replacement [8].
This study comprising of 30 patients who underwent radial head replacement for acute fractures of comminuted radial head fractures was aiming to prove that osteotomy performed 2 mm above the radial tuberosity was used as reference for level of osteotomy of radial neck and was most reliable in reproducing the results.
Materials and Methods
Patient data collection
After approval from the ethical committee, a prospective analysis of 30 consecutive patients (16 men and 14 women) sustained fractures of radial head from August 2016 to July 2020 was performed. The duration of this study was for 5 years. All patients were followed for a minimum of 4 years.
The outcomes of the surgery were reported based on Visual Analog Scale (VAS), Mayo Elbow Performance Index (MEPI) and Range of Motion (ROM).
Visual Analog Scale (VAS) is a 10 point score and a physician based scoring of the pain experienced by patient. Mayo Elbow Performance Index (MEPI) is a 100 point scoring system based on stability, pain, motion and strength.
Range of motion is measured from the degree of flexion and pronosupination available after surgery.
Inclusion criteria
• All comminuted un-repairable fractures with or without dislocation
• Both open and closed fractures
• Essex loppresetti injury
• Age between 20 and 80 years
Exclusion criteria
• Un-displaced fractures
• Displaced, uncomminuted fractures
• Comminuted re-constructible fractures
• All radial neck fractures/those extending into metaphysis
• Old fractures
Patient related data, surgery, postoperative course and follow-up data were collected for each patient.
• Patient related data included age, gender, mode of injury, comorbidity, nutritional status and associated injuries to the ipsilateral elbow.
• Surgical data included fracture type, duration of the operation, duration and type of anaesthesia.
• Postoperative data included range of motion, visual analog scale and mayo elbow performance index at follow up of 2 weeks, 6 weeks, and 3 months, 6 months, 1 year and 3 years.
Surgical technique and perioperative management
All the patients included in the study arrived to our casualty and were treated according to advanced trauma life support protocol. Head injuries and vital organ injuries were stabilized by different specialists.
Nature of the injury and the initial treatment given were enquired. Pain scores were noted according to visual analogue scale. Radiographs of the involved elbow and computed tomography scans were taken.
All surgeries were done under general anaesthesia. Torniquet was applied for all cases. Skin preparation was done with beta dine and sterilium.
Kocher approach was used to expose the fracture site. Skin incision was made along the distal most end of lateral border of humerus and radial head. Plane was created between the fibres of extensor digitorum communis and annular ligament and supinator are exposed. Forearm is kept in pronation and supinator is erased from the posterior cortex.
The neck was exposed adequately. The fractured radial head was removed. The neck was osteotomised with a 0.5 mm saw blade at a distance of 2 mm above the radial tuberosity. The medullary canal was prepared adequately. We used titanium implants for all our cases.
The size of the radial head was measured by reconstructing the native radial head. The head was reconstructed with trial implants. The position of the implant was checked under c arm. The correct size of the implant was determined by different trials. The size of the prosthesis is chosen. The prosthesis was replaced after cementation and movements were checked before closure (Figure 1).
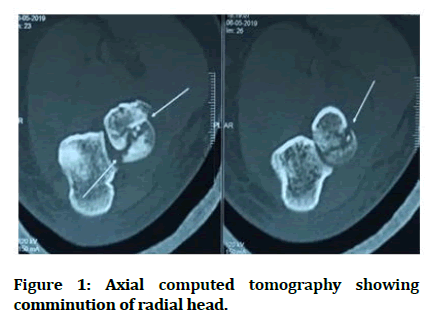
Figure 1: Axial computed tomography showing comminution of radial head.
Results
A total of 30 patients were selected of which 16 were males and 14 were females. The mode of injury is road traffic accident in 5 patients and fall on outstretched hand in 25 patients. The age distribution of the patient was 15 were between age 20 and 30, 6 were between 31 and 40, 6 were between 41 and 50, 1 was between 51 and 60, 2 were between 61 and 70 (Figures 2-7).
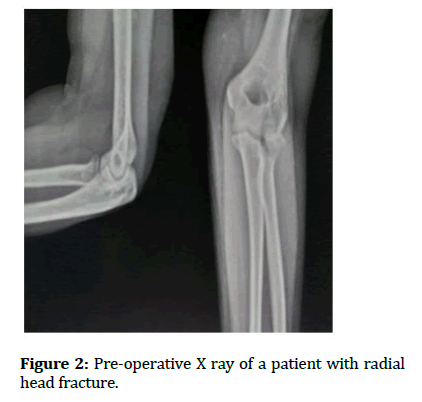
Figure 2: Pre-operative X ray of a patient with radial head fracture.
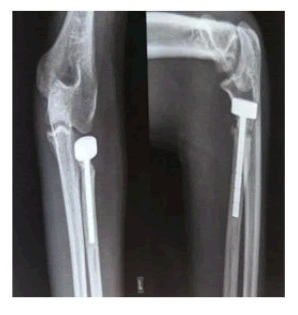
Figure 3: X ray of the elbow after 3 years.

Figure 4: Healed scar after 3 years.
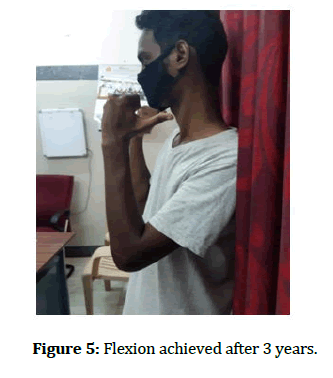
Figure 5: Flexion achieved after 3 years.
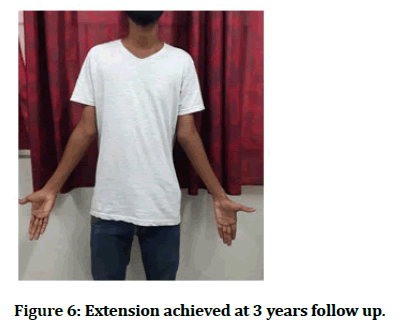
Figure 6: Extension achieved at 3 years follow up.
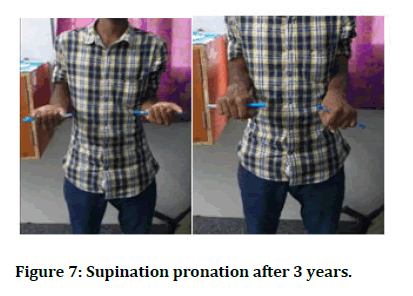
Figure 7: Supination pronation after 3 years.
The mean degree of flexion at 2 weeks, 6 weeks, 3 months, 6 months, 12 months and 3 years is 68.83 ± 12.844, 79.50 ± 11.988, 86.83 ± 13.357, 91.83 ± 14.650, 98 ± 16.167, and 115 ± 15.15 (Table 1).
| Duration | Mean (DEGREES) |
|---|---|
| 2 weeks | 68.83 ± 12.844 |
| 6 weeks | 79.50 ± 11.988 |
| 3 months | 86.83 ± 13.357 |
| 6 months | 91.83 ± 14.650 |
| 12 months | 98 ± 16.167 |
| 3 years | 115 ± 15.15 |
Table 1: The mean degree of flexion.
The mean pronation at 2 weeks, 6 weeks, 3 months, 6 months, 1 year and 3 years are 28.83 ± 12.154, 35.50 ± 10.615, 42.17 ± 10.144, 48.50 ± 11.682, 53.50 ± 13.528 and 55.15 ± 11.28 (Table 2).
| Duration | Mean Pronation (degrees) |
|---|---|
| 2 weeks | 28.83 ± 12.154 |
| 6 weeks | 35.50 ±10.615 |
| 3 months | 42.17 ±10.144 |
| 6 months | 48.50 ± 11.682 |
| 12 months | 53.50 ± 13.528 |
| 3 years | 55.85 ± 12.20 |
Table 2: The mean pronation.
The mean supination at 2 weeks, 6 weeks, 3 months, 6 months, 1 year and 3 years are 47.17 ± 10.059, 53.67 ± 9.908, 60.00 ± 10.171, 68.00 ± 8.469, 73.00 ± 9.879 and 75 ± 8.22 (Table 3).
| Duration | Mean (DEGREES) |
|---|---|
| 2 weeks | 47.17 ± 10.059 |
| 6 weeks | 53.67 ± 9.908 |
| 3 months | 60.00 ± 10.171 |
| 6 months | 68.00 ± 8.469 |
| 12 months | 73.00 ± 9.879 |
| 3 years | 75 ± 8.22 |
Table 3: The mean supination.
The mean visual analog scale of the patients at 2 weeks, 6 weeks, 3 months, 6 months, 12 months and 3 years is 5.06 ± 1.43, 7.6 ± 0.93, 8.13 ± 1.04, 8.26 ±1.04, 8.73 ± 1.08, 8.86 ±1.16 (Table 4).
| Duration | Mean VAS |
|---|---|
| 2 weeks | 5.06 ± 1.43 |
| 6 weeks | 7.6 ± 0.93 |
| 3 months | 8.13 ± 1.04 |
| 6 months | 8.26 ± 1.04 |
| 12 months | 8.73 ± 1.08 |
| 3 years | 8.86 ± 1.16 |
Table 4: The mean visual analog scale of the patients.
The mean MEPI score at 2 weeks, 3 months, 6 months, 12 months and 3 years are 52.6 ± 11.8, 64 ± 13.1, 72.83 ±14.5, 82.33 ± 14.2, 90.16 ±15.7, 95.85 ± 12.20 (Table 5).
| Duration | Mean MEPI score |
|---|---|
| 2 weeks | 52.6 ± 11.8 |
| 6 weeks | 64 ± 13.1 |
| 3 months | 72.83 ± 14.5 |
| 6 months | 82.33 ± 14.2 |
| 12 months | 90.16 ± 15.7 |
| 3 years | 95.85 ± 12.20 |
Table 5: The mean MEPI score.
Discussion
Radial head fractures account for 20% of the injuries around elbow [1]. In our study, the females were more than males and 50% people are young age between 20 and 30 years of age.
Fracture was associated with dislocation in 3 patients (10%), MCL injury in 2 patients (6%), coronoid fracture in 2 patients (6%) and essexlopresetti type in 1 patient (3%).
The average time interval between fracture and surgery is 14.5 hours in our study. Radial head replacement in comminuted radial head fractures with or without dislocation has good outcomes.
Recent studies by Grewal, et al. retrospectively reviewed 26 patients using a modular, metallic, mono block replacement with a loose press-fit stem and showed high satisfaction, mean DASH 24.4 and mean Mayo Elbow Performance Index (MEPI) of 83, and no revision surgery at two years.
In 2007, Job N Doornberg, et al. in their study of 27 radial head un-repairable fractures, has shown intentionally placed loose modular stems with metal spacer has shown favourable outcomes in unstable elbow fractures [8].
In 2007, Jijhun Zhao with titanium implants of radius shows excellent results in 5 patients, good in 4 patients and fair in 1 patient in a study involving 10 patients with a mean follow up of 23.7 years [9-12].
In 2012, Zunkiewicz, et al. evaluated 29 patients treated using a bipolar prosthesis with a loose stem and a mean follow-up of 34 months, and reported a mean MEPI score of 92 with only two patients requiring further surgery.
The Mayo Elbow Performance score (MEPI) was used for analysing the clinical outcome in our study. In our study, the flexion-extension has improved from 68 ± 12 degrees at 2 weeks to 98 ± 16 degrees at 1 year and 115 ± 15.15 at 3 years. Similarly, supination has also increased from 47.17 ± 10.059 degrees (2 weeks) to 73.00 ± 9.879 degrees (3 years).
The mean score of pronation at 2 weeks and 3 years are 28.83 ± 12.154 degrees (2 weeks) and 53.50 ± 13.528 degrees (3 years). The mean MEPI score has increased from 52 at 2 weeks to 95 at the end of 3 years. The VAS score has also increased from 5.6 at 2 weeks to 8.8 at the end of 3 years [13-15].
Chronic pain was reported in one case in our study, the visual analogue score is 5 at the end of 3 years. It is a complex injury with dislocation and coronoid fracture. The major limitation of our study is the limited number of cases and the lesser duration of study. The advantage of our study is that it is a single centre trial and the population was a representative of the local population of our region.
Conclusion
In our study, the neck was osteotomised at 2 mm above the radial tuberosity. The functional outcomes according to MEPI score, Visual Analog Score (VAS) and Range of Motion were better in our study compared to previous studies. Hence we recommend radial tuberosity as a most reliable reference point for radial neck osteotomy.
Reference
- Duckworth AD, Clement ND, Jenkins PJ, et al. The epidemiology of radial head and neck fractures. J Hand Surg Am 2012; 37:112-119
- Ikeda M, Sugiyama K, Kang C, et al. Comminuted fractures of the radial head. Comparison of resection and internal fixation. J Bone Joint Surg Am 2005; 87:76-84.
- Speed K. Ferrule caps for the head of the radius. Surg Gynecol Obstet 1941; 73:845-850.
- Mackay I, Fitzgerald B, Miller JH. Silastic replacement of the head of the radius in trauma. J Bone Joint Surg Br 1979; 61-B:494-497.
- Judet T, Garreau de Loubresse C, Piriou P, et al. A floating prosthesis for radial-head fractures. J Bone Joint Surg Br 1996; 78:244-249.
- Moungondo F, El Kazzi W, van Riet R, et al. Radiocapitellar joint contacts after bipolar radial head arthroplasty. J Shoulder Elbow Surg 2010; 19:230-235.
- Amis A. A. Axial forearm forces, forearm rotation, andradial head prosthesis. Presented at : The Elbow :International congress and instructional course, Dusseldorf, Germany, 2000.
- Van Glabbeek F, Van Riet RP, Baumfeld JA, et al. Detrimental effects of overstuffing or understuffing with a radial head replacement in the medial collateral-ligament deficient elbow. J Bone Joint Surg Am 2004; 86:2629-2635.
- Doornberg JN, Parisien R, van Duijn PJ, et al. Radial head arthroplasty with a modular metal spacer to treat acute traumatic elbow instability. J Bone Joint Surg Am 2007; 89:1075-1080.
- Zhao J, Yang S, Hu Y. The early outcomes with titanium radial head implants in the treatment of radial head comminuted fractures. J Huazhong Univ Sci Technolog Med Sci 2007; 2:681-683.
- Zunkiewicz MR, Clemente JS, Miller MC, et al. Radial head replacement with a bipolar system: a minimum 2-year follow-up. J Shoulder Elbow Surg 2012; 21:98–104.
- Beingessner DM, Dunning CE, Gordon KD, et al. The effect of radial head excision and arthroplasty on elbow kinematics and stability. J Bone Joint Surg Am 2004; 86:1730-1739.
- van Riet RP, van Glabbeek F, de Weerdt W, et al. Validation of the lesser sigmoid notch of the ulna as a reference point for accurate placement of a prosthesis for the head of the radius: a cadaver study. J Bone Joint Surg Br 2007; 89:413-416.
- Doornberg JN, Linzel DS, Zurakowski D, et al. Reference points for radial head prosthesis size. J Hand Surg Am 2006; 31:53–57.
- Moskowitz rw. Osteoarthritis: Diagnosis and Medical/surgical Management. Lippincott Williams and Wilkins 2007.
Author Info
Mervinrosario PM*, Vijay Narasimman Reddy and Aravind Ravichandran
Department of Orthopaedics, Sree Balaji Medical College and Hospital, Tamil Nadu, Chennai, IndiaCitation: Mervinrosario PM, Vijay Narasimman Reddy, Aravind Ravichandran, Determination of the Level of Osteotomy of Radial Neck with Radial Tuberosity as a Most Reliable Reference Point in Radial Head Replacement, J Res Med Dent Sci, 2022, 10 (10): 056-061.
Received: 29-Jul-2022, Manuscript No. JRMDS-22-57715; , Pre QC No. JRMDS-22-57715(PQ); Editor assigned: 01-Aug-2022, Pre QC No. JRMDS-22-57715(PQ); Reviewed: 16-Aug-2022, QC No. JRMDS-22-57715; Revised: 30-Sep-2022, Manuscript No. JRMDS-22-57715(R); Published: 10-Oct-2022
