Research - (2021) Volume 9, Issue 6
Diagnostic Role of Fibreoptic Bronchoscopy in Sputum Smear Negative Pulmonary Tuberculosis
Modugula Padmapriya, V Suryanarayana and Raja Amarnath G*
*Correspondence: Raja Amarnath G, Department of Pulmonary Medicine, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
The global strategy for Tuberculosis control is prompt diagnosis and treatment of transmissible disease. The mainstay of diagnosis of Pulmonary Tuberculosis is demonstration of AFB in the sputum smears, but not all patients have positive sputum AFB smears despite of clinical and radiological being consistent with Tuberculosis. The prospective, randomized study was designed to study the bronchial washings for microscopy and culture examination for M. tuberculosis and compare with AFB culture of the sputum obtained before bronchoscopy. The Present study focuses on to study the post-bronchoscopy sputum for microscopic examination for acid fast bacilli and to observe if there is any contributory effect to case detection. The present study is done with an aim to verify if the bronchial washings and post bronchoscopic sputum have any additional diagnostic yield in cases of Smear Negative Pulmonary Tuberculosis.
Keywords
Smear negative pulmonary tuberculosis, Bronchoscopy, Sputum, AFB, Granulations
Introduction
Tuberculosis (TB) is a major health problem around the world, with an approximate incidence of 8.6 million and about 0.94 million TB-related deaths in 2012. India has the highest burden of Tuberculosis and as it is affecting mainly the economically productive population, it has an impact on the country's economy. There are studies conducted 1n foreign countries and India also. The differences in incidence and emergence of resistant forms due to inappropriate treatment of Tuberculosis with changing times warrants for reassessment of the role of these diagnostic modalities [1].
The global strategy to control TB is prompt diagnosis, notification, and successful treatment of patients with active, transmissible disease. Early diagnosis of active pulmonary tuberculosis (PTB) is critical for TB control. According to WHO estimates, incidence of TB cases in India in 2012- 2.2 million (176/100 000 population), prevalence is 230/100 000 · Population with a mortality of 0.27 million (22/100 000 population). Among these new cases, 0.6 million are sputum smear positive [2]. One sputum positive patient can infect 10-15 persons in a year if left untreated. Poorly treated patients can develop drug resistance, potentially incurable forms of Tuberculosis and also spread these resistant forms to others, thus increasing the economic burden on the nation.
The initial diagnostic approach to a suspected case of Pulmonary Tuberculosis 1s to demonstrate Mycobacterium tuberculosis bacilli in the sputum. Even after meticulous search, a large portion of patients remain smear negative (22-67%) for TB in spite of clinical and radiological picture being consistent with diagnosis of Pulmonary Tuberculosis [3]. The reason could be inadequate quantity of sputum or poor quality sputum or sputum being diluted with upper respiratory tract secretions. In those cases, even culture of sputum may not be much contributory. The difficulty is further compounded by the fact that conventional culture of mycobacterium requires 6-8 wks [4]. Reaching a decision to treat is a challenge for physicians treating any of these patients. Anti-Tubercular treatment in these cases can be a potential risk for drug toxicity.
There is an added risk of missing or delay in diagnosis of a potentially curable alternative disease. Early diagnosis and proper treatment of Pulmonary Tuberculosis prevents progression of disease, morbidity, spread of disease and all its complications. In such a situation bronchoscopy has been tried to verify whether we can improve positive results for tuberculosis by taking samples from within the bronchial tree. The idea is that during bronchoscopy the most affected segment can be approached and hence the chance of getting a better specimen without contamination can be obtained and the chances of positivity may be improved. Also separate samples can be obtained from various segments or lobes.
Fiberoptic bronchoscopy with bronchial washings and analysis of it for AFB including culture for Mycobacterium tuberculosis has significant role to establish the diagnosis in those cases where the extensive search for AFB in expectorated sputum has repeatedly failed or those cases where sputum expectoration is absent or the sputum induction has failed. A total of 35 patients with suspected Smear Negative Pulmonary Tuberculosis (according to WHO criteria) were enrolled in the present study. A pre bronchoscopic sputum sample is sent for AFB culture for all the patients. These patients were subjected to fiberoptic bronchoscopy after obtaining an informed written consent. Bronchial washings were collected and sent for AFB smear microscopy and AFB culture and post bronchoscopic sputum was sent for AFB smear microscopy. The data collected was analyzed using the statistics software SPSS version 17.0.
Materials and Methods
The present study "Diagnostic role of fibreoptic bronchoscopy In sputum smear negative pulmonary tuberculosis" was conducted In the Department of Pulmonary Medicine, Sree Balaji Medical College and Hospital, Chromepet, Chennai after obtaining the approval from Institutional Human Ethical Committee.
Study design
The present study is a prospective observational study.
Study period
The study is carried from November, 2011 to April, 2013.
Sample size
A total of 35 patients were enrolled into the study.
New smear negative cases, clinically and radiological suspected of Pulmonary Tuberculosis were selected in this study. Detailed history of such patients was recorded including history of Anti Tubercular treatment and any pre-disposing factors. Thorough clinical examination was done. Patients were selected on basis of the following inclusion and exclusion criteria.
Inclusion criteria
Patients who are suspected as sputum smear negative pulmonary Tuberculosis on the basis of clinical picture consistent with Pulmonary Tuberculosis.
• Cough with/without expectoration of more than 2 weeks.
• Fever.
• Loss of appetite and loss of weight.
• Hemoptysis, chest pain.
Two sputum smears negative for acid fast bacilli (Spot, early morning sputum sample).
X-ray suggestive of Pulmonary tuberculosis.
• Infiltrations.
• Cavitations.
• Multi nodular fluffy shadows.
Patients of age more than 18yrs.
Patients willing to be included in the study and willing for the investigations.
Exclusion criteria
• Patients who were severely dyspnoeic.
• Recent myocardial infarction, arrhythmias.
• HIV positive patients and HBsAg positive patients.
• Age less than 18 years and more than 75yrs.
• Patients with extra pulmonary tuberculosis.
• Patients with history of taking ATT in the past.
• Patients who are not cooperative for bronchoscopy.
Consent
An informed written consent was taken from all the patients enrolled in the study after a proper health education.
Methods
Patients who were fitting into the inclusion and exclusion criteria were taken in to the study.
The following investigations were done in all the patients.
Routine investigations
• Complete blood picture.
• Erythrocyte sedimentation rate (ESR).
• Random blood sugar.
• Complete urine examination.
• Chest X-ray P.A. view and lateral view.
• ECG.
• HIV, HBsAg.
• Sputum for acid fast bacilli.
• Spot sample.
• Early morning sample.
• Sputum for AFB culture.
Bronchoscopy followed by following investigations
• Bronchial washings for AFB staining (Z-N staining).
• Post bronchoscopes sputum for AFB staining.
• Bronchial washings for AFB culture by BACTEC MGIT.
• Bronchial washings for cytology and cell count.
• Biopsy for histopathological examination (if needed).
Bronchoscope was advanced into the nostril under direct vision with gentle pressure it was passed along the floor of the nose through the widest visible opening between the turbinate’s, For patients who had nasal apertures for shaft of bronchoscope , patients was asked to hold bite block between the teeth and instrument was introduced through the or pharynx. The instrument was advanced with the tip flexed downwards till glottis and larynx were in view , the movement of vocal cords with respiration was noted, 2% lignocaine was pushed through the suction channel of bronchoscope to prevent apposition of vocal cords, while advancing. The tip of bronchoscope was centered with regard to vocal cards and was quickly advanced through the opening once bronchoscope was passed through the cords, 2ml of 2% lignocaine was given and bronchoscope was maneuvered into the normal bronchial tree first and then on the abnormal side. If bilateral lesions were present bronchoscope was maneuvered first on the right side , scope was maneuvered up to segmental bronchi and observed for mucosa! irregularity, ulcerations , granulations and any growth.
Bronchial washing was performed by instilling 0.9% isotonic saline at room temperature through the internal channel of FOB and aspirated into a trap connected to suction tubing. Usually 15-30 ml of fluid was instilled with each washing and about ¼ to ½ of this volume was retrieved in the suction trap.
The collected bronchial washing samples were sent for
• AFB smear microscopy (Z-N staining).
• AFB culture by BACTEC MGIT.
• AFB smear microscopy (Z-N staining).
The post bronchoscopy sputum was not submitted for AFB culture for want of funds.
Results
The following observations were made from the data in the master chart. The observations were presented in the following tables and graphs.
The study population consisted of 24 males (68.57%) and 1(31.4%) females. The male and female ratio of the study population was about 2:1. The youngest patient was aged 19 years and oldest 68 years. Mean age of the study population was 42.8years. The mean age of males was 44.20years and that of females was 39. 7 years. Mean age of males was more than that of females. Most of the patients (11) came under the age group of 25-34. In this age group also the male to female ratio is almost 2: l (same as that of the study population) . The age and sex distribution of the patients was presented in Table 1.
| Age (In years) | Males | Females | Total | |
|---|---|---|---|---|
| Number | Number | Number | Percent | |
| <24 | 1 | 1 | 2 | 5.7 |
| 25-34 | 7 | 4 | 11 | 31.4 |
| 35-44 | 5 | 2 | 7 | 20 |
| 45-54 | 4 | 2 | 6 | 17 |
| 55-64 | 4 | 1 | 5 | 14 .3 |
| 65-74 | 3 | 1 | 4 | 11.4 |
| Total | 24 | 11 | 35 | |
Table 1: Age and sex distribution of patients.
Symptoms
The symptoms of the patients with the percentages are presented in Table 2.
| Symptoms | Number of Patients | Percentage |
|---|---|---|
| Cough | 32 | 91.4 |
| Fever | 24 | 68.6 |
| Loss of appetite and weight | 20 | 57 |
| Hemoptysis | 6 | 17 |
| Chest pain | 5 | 14.3 |
Table 2: Symptoms of patients.
Cough was the most common symptom (91.4%) followed by fever (68.6%) and loss of appetite and weight (57%). The other symptoms included haemoptysis (17%), and chest pain (14.3%). Haemoptysis was found to be common in males (5 /6 patients) and most of them had symptoms for less than 4 wks duration at the time of presentation. 4 out of 6 patients with haemoptysis belonged to the age group 25-34yrs.
Duration of illness
The duration of illness of the patients 1s shown in Table 3 and Figure 1 below.
| Duration of illness | Number of patients | Percentage |
|---|---|---|
| 2 wks | 6 | 17.14% |
| >2wks- upto 4 wks | 17 | 48.60% |
| >4wks-upto 6wks | 0 | 0% |
| >6wks-upto 8wks | 1 | 2.90% |
| >8wks-upto | 6 | 17.14% |
| 4months | ||
| >4months-upto 6 | 2 | 5.70% |
| months | ||
| 2:6months | 3 | 8.60% |
Table 3: Duration of illness.
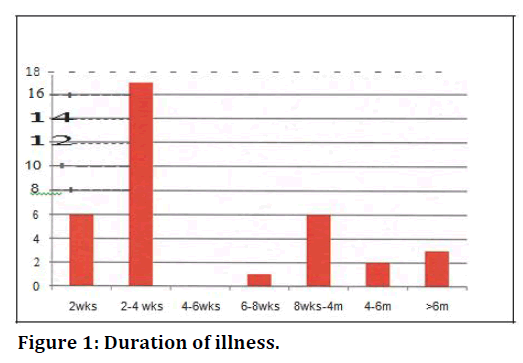
Figure 1. Duration of illness.
Radiological manifestations
Table 4 and Figure 2A and Figure 2B below show the radiological manifestations of the patients. Of the 35 patients, 32 (91.3 %) patients had unilateral lesions and 3 (8.6%) had bilateral lesions. Of the 32 patients with unilateral lesions, 19(54.3%) had right sided lesion and 13(37.1 %) had left sided lesion. Four patients (11.5%) had cavitatory lesions and all four patients have nilateral cavity (right sided in 3 patients and left sided in 1 patient). Bronchoscopic findings are mentioned in Table 5 and Figure 3.
| Radiological Manifestations | Number | Percentage | ||
|---|---|---|---|---|
| Site of Lesion | Right | 19 | 54 .3 | |
| Left | 13 | 37.1 | ||
| Bilateral | 3 | 8.6 | ||
| Total | 35 | |||
| Type of lesion | Cavitatory | Single | 3 | 8.6 |
| Multiple | 1 | 2.9 | ||
| Total | 4 | 11.5 | ||
| Non-Cavitatory | Diffuse infiltration | 10 | 28.6 | |
| Localised infiltration | 21 | 60 | ||
| Total | 31 | 88.6 | ||
Table 4: Radiological manifestations.
| Findings | Number of Patients with the finding (out of 35 patients) | Percentage |
|---|---|---|
| Congestion with hyperemia | 30 | 85.7 |
| Erosion, Granulation | 3 | 8.6 |
| Segmental bronchial | 8 | 22.9 |
Table 5: Bronchoscopic findings.
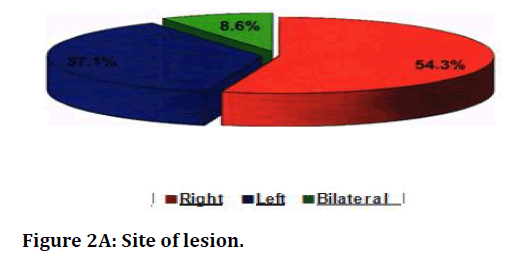
Figure 2A. Site of lesion.
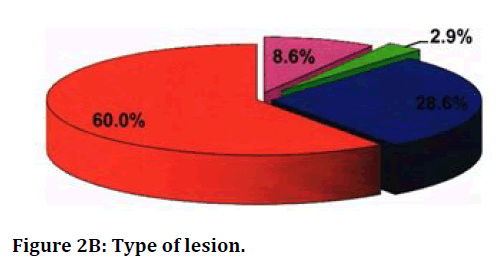
Figure 2B. Type of lesion.
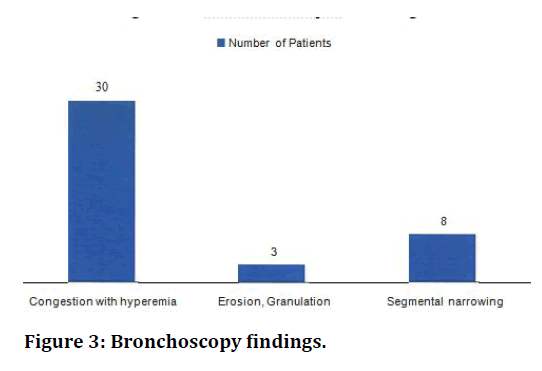
Figure 3. Bronchoscopy findings.
Results of the investigations performed on bronchoscopic specimens
In the patients included in the study, we had sent a sputum sample for AFB culture before doing the bronchoscopy (pre bronchoscopic sputum sample). During bronchoscopy, bronchial washings were obtained and these samples were sent for AFB smear microscopy and AFB culture. Also we had collected the 24 hr sputum after bronchoscopy (post bronchoscopy sputum) and sent the sample for AFB smear microscopy. The results of all samples were shown in Table 6 below. The sputum samples collected before bronchoscopy was positive for culture for AFB in 7 patients out of the 35 patients. The AFB culture of the sputum samples collected before bronchoscopy was positive in 7 patients. The AFB smear microscopy of bronchial washings was positive in 8 patients. All these 8 patients whose bronchial washings had a positive result in AFB smear microscopy had AFB cultures of bronchial washings also positive. Apart from these 8 patients, the AFB culture of bronchial washings was positive in 13 more patients (total patients with positive AFB culture of bronchial washings is 21).The microscopic examination of post bronchoscopic sputum yielded acid fast bacilli in 6 patients. In 15 patients, pulmonary tuberculosis was confirmed by bronchial washing samples alone. In 9 patients out of the 35 patients included in this study, none of the analysed samples gave a positive yield for AFB. Of these 9 patients, granuloma was found in bronchoscopy in one patient and the histopathological examination revealed a Tubercular granuloma.
| Sample and investigation | No. of patients with positive yield (Out of 35) |
|---|---|
| Bronchial washing AFB Smear microscopy | 8 |
| Bronchial washing AFB Culture | 21 |
| Post Bronchoscopy sputum AFB Smear microscopy | 6 |
Table 6: Results of the investigations performed on sputum obtained before bronchoscopy, bronchial wash samples and post bronchoscopy sputum.
The AFB culture of the sputum samples obtained before bronchoscopy (pre bronchoscopic sputum) was positive in 7 patients and negative in 28 patients whereas AFB culture of bronchial washings was positive in 21 patients and negative in 14 patients. These results were consolidated and depicted in Table 7 below. Among the 21 patients with positive yield in bronchial washings AFB culture, a few also have positive yield on prebronchoscopic sputum. This showed that the AFB culture of bronchial washings gave a positive yield in more number of cases than the AFB culture of pre bronchoscopic sputum.
| Sample | No. of patients with positive yield (out of 35) |
|---|---|
| Pre bronchoscopy sputum AFB culture | 7 |
| Bronchial washings AFB culture | 21 |
Table 7: Comparison of AFB culture of sputum obtained before bronchoscopy and afb culture of bronchial washings.
The AFB smear microscopy of bronchial washings was positive in 8 patients and negative in 27 patients. The AFB smear microscopy of post bronchoscopy sputum was positive in 6 patients and negative in 29 patients. These findings were consolidated in the following Table 8.
| Sample | No. of patients with positive yield (Out of 35) |
|---|---|
| Microscopic examination of Bronchial washings smear for AFB |
8 |
| Microscopic examination of Post bronchoscopy sputum smear for AFB |
6 |
Table 8: Comparison of the results obtained from AFB smear microscopy of bronchial washings and AFB smear microscopy of Post bronchoscopy sputum.
Yield of bronchoscopy
Immediate yield of TB by bronchoscopy=8/3 5x100=22.8% (Smearmicroscopy of bronchial washing were positive 1n 8 patients only). Exclusive diagnosis by bronchoscopy=20 /35 x 100= 45 . 7% (Includes those patients who have AFB positivity on bronchial washings and/or post bronchoscopy sputum and the patient with TB granuloma. Excludes the 7 patients with positive prebronchoscopic sputum AFB culture and the 8 pa tients with all samples negative)
Yield of post bronchoscopy sputum= 6/35 X 100 =17.14%
Bronchial washing yield
If total patients with AFB positivity in bronchial washings = 21 /35 X 100=60% (21 patients had positive results 1n AFB culture of bronchial washings). Exclusive AFB positivity by bronchial washings=15/35 x 100=42.8% (In which pre bronchoscopy sputum sample and post bronchoscopy sputum samples were negative and only bronchial washings were positive for TB).
Immediate AFB positivity of Bronchial washing=8/35 x 100=22.8% (AFB smear microscopy of bronchial washings was positive in 8 patients and gave the diagnosis of TB immediately).
Correlation statistics
Correlation with duration of illness: of the 21 patients who had positivity in AFB cultures of bronchial washings, 17 have symptoms for less than 2 months (P value-0.126) (Table 9).
| Duration of illness in months | Bronchial wash AFB culture | Total | |
|---|---|---|---|
| Positive | Negative | ||
| Below 2 | 17 | 7 | 24 |
| 2-6 | 4 | 5 | 9 |
| Above 6 | 0 | 2 | 2 |
Table 9: Correlation between duration of illness and bronchial washing results.
Correlation between age and AFB culture of bronchial washings
Among the 21 patients with positive results in AFB culture of bronchial wash, 8 patients belonged to the age group 25-34 yrs. (p value - 0.188) .Two patients in this study were under the age group l 8-24yrs and both the patients have positive results in AFB culture of Bronchial washings. This data is shown in Table 10 below.
| Age group (yrs) | Bronchial wash AFB culture positive | Bronchial wash AFB culture negative | Total |
|---|---|---|---|
| 18-24 | 2 | 0 | 2 |
| 25-34 | 8 | 3 | 11 |
| 35-44 | 5 | 2 | 7 |
| 45-54 | 2 | 4 | 6 |
| 55-64 | 1 | 4 | 5 |
| 65-74 | 3 | 1 | 4 |
Table 10: Correlation between age group and AFB culture of bronchial wash.
Correlation between radiological lesions and AFB culture of bronchial washings
The correlation statistics revealed that the AFB cultures of bronchial washings were positive in 57.9% (11/19) patients with right sided lesions. The AFB cultures of bronchial washings were positive in 69.2% (9/13) patients with left sided lesions (p=0.670). These observations are given in Table 11 below.
| Side of lesion | Bronchial wash AFB culture positive | Bronchial wash AFB culture negative | Total |
|---|---|---|---|
| Right | 11 | 8 | 19 |
| Left | 9 | 4 | 13 |
| Bilateral | 1 | 2 | 3 |
Table 11: Correlation between side of the lesion and AFB culture of bronchial washings.
Among the patients with cavitations lesions, the AFB cultures of bronchial washings were positive in 75% (3/4) of patients. The AFB cultures of bronchial washings were positive in 58% (18/31) of patients with infiltrating lesions (p=0.784). This is depicted in Table 12.
| Type of lesion | Bronchial wash AFB culture positive | Bronchial wash AFB culture negative | Percentage positivity |
|---|---|---|---|
| Single cavity | 2 | 1 | 66.7 |
| Multiple cavity | 1 | 0 | 100 |
| Total cavitating lesis | 3 | 1 | 75 |
| Diffuse infiltrates | 5 | 5 | 50 |
| Localised infiltrates | 13 | 8 | 61.9 |
| Total infiltrating lesions | 18 | 13 | 58 |
Table 12: Correlation between type of lesion and bronchial wash AFB culture results.
Discussion
The mean duration of illness was 10.3 weeks, ranging from 3 to 24 months.
Symptoms of the patients
In present study 91.4% patients had cough, 68.6% had fever, 57%of patients had symptoms like loss of appetite, loss of weight, 17% had haemoptysis and 14.3% had chest pain.
Comparing to other studies, observed cough in 68%, fever in 70%, haemoptysis 1n 28%, and constitutional symptoms in 30% of patients. In Kulpati et al [4] study, 55% patients had cough, 50% fever, 20% had haemoptysis and 40% had constitutional symptoms. In Purohit et al [5] in this study observed, all patients had cough as major symptom, 64% had fever 36% had haemoptysis and 38% had constitutional symptoms. The symptomatology of patients in our study was comparable with the above studies.
Bronchoscopy findings
In present study 85.7% of cases showed congestion with hyperemia of bronchial mucosa on bronchoscopy, 8.6% of patients had erosion , ulceration and granulation on bronchoscopy, while segmental narrowing was observed in 22.9% patients. Some cases had multiple findings on bronchoscopy.
Kulpati et al [4] observed coating of mucosa of involved segments with yellowish white secretions in almost all patients and also revealed mild to moderate hyperemia after bronchial wash. Segmental bronchus was narrowed in 20% patients, and ulceration was seen in 20% patients.
Purohit et al [5] reported that ulceration was seen in 64% of patients and 60% had frothy secretion from the bronchus . A moderate hyperemia of bronchial mucosa was observed in all the patients.
Similar observation was made by Panda et al [6], in their study 44% had normal bronchial mucosa, 21% had unhealthy mucosa with granulat io ns, 35% had mucopurulent discharge from bronchus , 5% had growth , 3% had external compression and 3% had bleeding from bronchus and some cases had multiple findings.
Yield of bronchoscopy samples
Danek et al. [7] and Purohit et al [5] demonstrated acid fast bacilli in bronchial wash smear in 34% and 42% respectively whereas in study by Kulpa ti et al [4] 40% were positive. In our study 22.8% were positive. All these were confirmed by positive culture. The results of stained smear examination of bronchial washing was confirmed by culture in 100% of cases in the present study, which is comparable to the studies by Kuti et al [4] (100%), Danek et al. [7] (95 %) , Sarkar et al. [8] (7%) respectively. In present study the positive culture rate was 60% only similar to that reported by Kulpati et al [4]. Kvale et al [9] could grow AFB only in one third of the patients of suspected tuberculosis.
Kulpati et al [4] reported the exclusively positive diagnostic results were provided by culture of prebronchoscopic sputum and bronchoscopic aspirate in 5% and 10% respectively while in our study these results were 8.5% and 42.8% respectively.
Wallace et al. [10] and Danek et al. [7] had reported 95% culture positivity of specimens obtained by flexible fiberoptic bronchoscopy and therefore negative culture provided strong evidence against tuberculosis. In our study the culture positivity of the specimen obtained by flexible fiberoptic bronchoscope was 60%. This disparity might be because the transbronchial biopsy and post bronchoscopy sputum AFB culture was not done in our study. Post bronchoscopy sputum studies provide collaborative evidence in sputum smear negative pulmonary tuberculosis. In various previous studies flexible fiberoptic bronchoscopy in combination with trans bronchial lung biopsy provided early diagnosis in 60% to 85% of smear negative pulmonary tuberculosis. In our study flexible fiberoptic bronchoscopy provided the diagnosis of Tuberculosis in 68.57% of patients which is similar to the previous studies.
Bronchial washings with other parameters
In the present study we have observed that AFB cultures of bronchial washings were positive 1n more number of patients with age less than 35yrs.It has been observed that AFB culture of bronchial washings was positive in 69.2% of patients with left sided lesions on radiograph and in 57.9% of patients with right sided lesions. Bronchial washing AFB cultures were found to be positive in 75% of patients with cavitation’s lesions as compared to 58% in case of patients with in filtrations.
Comparison of bronchoscopy results with that of AFB cultures of pre bronchoscopy sputum
In the study population, AFB culture of the pre bronchoscopy sputum was positive in 7 patients only. An additional 20 patients were diagnosed with Tuberculosis with the help of bronchoscopy (positive results on bronchial washing AFB smear microscopy/ AFB culture, AFB smear microscopy of post bronchoscopy sputum, HPE of the granuloma). Among these patients, AFB smear microscopy of bronchial washing was positive in 8 patients thus providing an immediate diagnosis of Tuberculosis and aiding the physician to start the course of ATT immediately and thus helping in reducing the transmission rates.
Conclusion
The following conclusions were drawn after analysis of the data in the study: Fibreoptic bronchoscopy is helpful in confirming the diagnosis of Tuberculosis in a substantial number of smear negative Pulmonary Tuberculosis cases. It has been observed that among the various methods of samples collected (prebronchoscopic sputum, bronchial washings, post bronchoscopic sputum samples) the bronchial washings gave maximum positivity for AFB by microscopy and culture examination. B smears copy of post bronchoscopy sputum gave an exclusive diagnosis of Tuberculosis in one patient only. Hence it is inferred that it didn't have any significant contributory effect. Though the fibre optic bronchoscopy might not be useful for routine use in the diagnosis of Tuberculosis, it proved to be useful in a few selected cases in special situations. Hence the study needs to be supported by a large sample size and the inclusion of post bronchoscopy sputum AFB culture and trans bronchial biopsy might be contributory.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The encouragement and support from Bharath Institute of Higher Education and Research, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- http://www.who.int/gho/tb/epidemic/cases_deaths/en/index.html
- https://www.who.int/teams/global-tuberculosis-programme/data
- Narain R, Subbarao MS, Chandrasekhar P, et al. Micrscopy positive and microscopy negative cases of pulmonary tuberculosis. Am Rev Respir Dis 1971; 103:761-3.
- Kulpati DDS, Heera HS. Diagnosis smear negative pulmonary tuberculosis by flexible fibreoptic bronchoscopy. Indian J Tuber 1986; 33:179-82.
- Purohit SD, Sisodia RS Gupta PR, et al. Fiberoptic bronhoscopy in the diagnosis of smear negative pulmonary tuberculosis. Lung India 1983; 1:143-146 .
- Panda BN, Rajan KE, Jena J, et al. Diagnostic yield from flexible fibreoptic bronchoscopy in sputum smear negative pulmonary tuberculosis cases. Ind J Tub 1995; 42:207-209.
- Danek SJ, Bower JS. Diagnosis of pulmonary tuberculosis by flexible fiberoptic bronchoscopy. Am Rev Respir Dis 1979; 119:677-679.
- Sarkar SK, Sharma GS, Gupta PR, et al. Fiberoptic bronchoscopy in the diagnosis of pulmonary tuberculosis. Tubercle 1980; 61:97-99.
- Kvale PA, Johnson MC, Wroblewski DA. Diagnoses of tuberculosis, routine cultures of bronchial washings are not indicated. Chest 1979; 76:140-42.
- Wallace JM, Deutsch AL, Harrell JH, et al. Bronchoscopy and transbronchial biopsy in evaluation of patients with suspected active tuberculosis. Am J Med 1981; 70:1189-1194.
Author Info
Modugula Padmapriya, V Suryanarayana and Raja Amarnath G*
Department of Pulmonary Medicine, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Modugula Padmapriya, V Suryanarayana, Raja Amarnath G,Diagnostic Role of Fibreoptic Bronchoscopy in Sputum Smear Negative Pulmonary Tuberculosis, J Res Med Dent Sci, 2021, 9(6): 375-483
Received: 08-May-2021 Accepted: 23-Jun-2021
