Research - (2021) Volume 9, Issue 8
Dietary Intervention for Glycaemic Control among Patients with Type 2 Diabetes Mellitus at the Medical Clinic, Teaching Hospital, Batticaloa, Sri Lanka
Sundaresan Thadchanamoorthy, Kisokanth Gnanaselvam*, Kumanan Somasuriyam and Majitha Seyed Ibrahim
*Correspondence: Kisokanth Gnanaselvam, Department of Clinical Nursing, Faculty of Nursing, University Colombo, Sri Lanka,
Abstract
Background: Health education on the proper diet is of paramount importance in the management of type 2 Diabetes Mellitus (T2DM). The study was aimed to assess the effectiveness of health education on low carbohydrate diet and standard recommended diabetic diet among T2DM patients in the medical clinics of Teaching Hospital, Batticaloa District, Sri Lanka Methods: A prospective intervention study was conducted among 135 patients with T2DM. Participants were randomly assigned into control (n=45, group I), an intervention group with a standard diet (n=45, group II), and an intervention group with a low carbohydrate diet (n=45, group III). The primary outcome was glycosylated haemoglobin (HbA1c). ANOVA was used to compare the means among all three groups and p <0.05 was considered statistically significant for all tests. Results: After 3 months, mean HbA1c was significantly lower in group III compared to group I and group II [F (2, 132)=5.28, p=0.006], and the mean difference of HbA1c was declined by 1.07 % in group III. A statistically significant difference was observed in the mean differences of HbA1c level across three groups [F (2, 132)=8.84, p=0.000]. Further, there was no statistically significant difference was observed in the HbA1c level across all three groups at 6 months (>0.05). Conclusions: HbA1c level was significantly reduced among the intervention group with a low carbohydrate diet. Self-management of T2DM through dietary intervention was successful with positive glycaemic control. Sustainability of glycaemic control cannot be possible after the cessation of dietary intervention.
Keywords
Health education, Glycaemic control, Prospective studies, Carbohydrate-restricted diet, Type 2 diabetes mellitus, Glycated haemoglobin A
Introduction
Every year nearly 38 million people die due to noncommunicable diseases (NCD) worldwide and among them, two-thirds live in lower- and middle-income countries [1]. Most of these deaths is due to four common NCDs such as cardiovascular diseases (heart attack and stroke), Diabetes Mellitus (DM), cancer, and chronic respiratory diseases [2]. DM was considered as the most common and worst NCD, associated with significant morbidity and mortality worldwide [3]. World Health Organization (WHO) has declared that the incidence of DM is increasing rapidly worldwide.1 All age global prevalence of DM was estimated to be 2.8% in 2000 and is predicted to be 4.4% in 2030 and currently, 190 million people around the world suffer from DM with over 330 million predicted to have the condition by 2025 and 366 million by the year 2030 [4]. The standardized prevalence for Sri Lankans aged above 20 years was 10.3 % [5]. Further, Type 2 DM (T2DM) accounts for 85–90% of DM worldwide [6] and DM in Sri Lanka seems to be mainly of T2DM [7]. All South Asians have high rates of T2DM [8] and are more likely to develop T2DM at younger ages [9]. The prevalence of DM has been progressively increasing over the years due to a combination of genetic and environmental factors, due to urbanization and industrialization which have led to a sedentary life, physical inactivity, stress, and obesity in Sri Lanka [7].
Traditionally, the treatment of T2DM has been a stepwise introduction of lifestyle modification and dietary control followed by hypoglycaemic agents.6Intensive glycaemic control has been shown to delay or prevent the development of DM-related microvascular complications [10]. However, an estimated 43.2-55.6% of adult with T2DM do not meet the American Diabetes Association target for glycaemic control (HbA1c <7.0%) due to inadequate home glucose monitoring, non-compliance with medications or lifestyle changes, suboptimal patient awareness about the disease, poor dietary habits and limited access to providers for diabetes management [11].
Dietary intervention is of paramount importance in the management of T2DM. Dietary management has become the most reliable support regimen through which a diabetic patient can be benefited [12] and which is a key component in the long-term health and quality of life of T2DM patients [13]. Notably, there are different prescribed diets across countries [14]. Carbohydraterestricted diets (CRDs) have been reported to be an effective diet for glycaemic control in T2DM [15,16] which diet led to a significant reduction in HbA1c levels compared to a standard diet among patients with T2DM [17]. Further, CRDs in which restricting carbohydrate (45% carbohydrate) intake can reduce insulin levels, reduce postprandial Hyperglycemia, and improve insulin sensitivity [18].
Dietary intervention through health education can be provided as part of a comprehensive diabetes selfmanagement and support program [19]. The dietary education related to the management of diabetes has been proved to improve patients’ nutritional status, clinical status, and the effectiveness of treatment, quality of life, daily functioning, and survival [20]. According to the available data, the effectiveness of different diet therapy intervention in improvement of glycaemic control among T2DM patients in the Batticaloa District have not been studied up to date. Thus, the study was aimed to assess the effectiveness of the standard dietary intervention and low carbohydrate diet intervention for glycaemic control through an intervention study in the medical clinics of Teaching Hospital, Batticaloa District, Sri Lanka. This study would help the health care professional to manage T2DM successfully in the Batticaloa district as well as nationwide.
Materials and Methods
This study was an intervention study conducted in the Medical Clinic, Teaching Hospital, Batticaloa (THB), Sri Lanka. The medical clinic at the Teaching Hospital Batticaloa caters to the diabetes population seeking services from this institution. Patients with T2DM, age up to 60 years, who have no concurrent participation in another research study, and who could provide informed consent were included in the study. Patients with type 1 DM, uncontrolled hypertension (blood pressure >180/110 mm hg), and diabetes complications (heart failure, End-stage kidney disease, and amputated patients) were excluded from the study.
The participants were randomly assigned to one of three groups; Group I – Control group; Group II–Intervention group with health education on a standard diet (E); Group III – Intervention group with health education on low carbohydrate diet (E + P). The sample size for each group was calculated using equation [21] as follows. Zα=1.96, Zβ=0.84 corresponding to an alpha error of 0.05, a power of 80%. The investigators anticipate that the proportion of patients HbA1C under control is around 3.5% in intervention group III (17), 2.3% percent in intervention group II [22], and around 0.7% in the control group [23]. The difference in treatment efficacy that the investigators wish to rule out was θ=0.10 (10%). S (Investigators wish to randomize n patients to experimental group and sn to control group) S=1 and calculated sample size for each group were n=45 including 10% of non-response rate. A total of 135 patients were recruited.
Allocation to the group occurred at the time of initial contact by the Research Assistant. Participants were informed of the study using an information sheet and if they were willing to participate in the study, they were then allocated randomly to either a group I, II, or III.
Participants in the control group were received only the usual care at the hospital. They were asked to follow as usual with the usual advice from the doctors. The control group was examined and investigated at baseline, 3 months, and 6 months with no other interaction in between with study staff. For group II, health education on standard diet published by Dietary Guidelines and Nutrition Therapy for Specific Diseases, Nutrition Division, Ministry of Health, Sri Lanka, 2014 [24] was promoted by investigators. There was a one-hour education session at baseline. Afterward, 30 minutes session was held once per month up to 3 months from baseline. For group III, health education on a low carbohydrate diet was conducted by investigators. Low carbohydrate diet instructions as described by Haimoto et al. [17]. There was a one-hour education session at baseline. Afterward, 30 minutes sessions were held once per month up to 3 months from baseline. A meta-analysis of the effect on glycaemic control by self-management education done by Norris et al. stated that the mean total contact time for clinical trials is 9.2 hours which ranges from 1-28 hours and the number of contacts with study participants ranges from 1-36 hours [25].
All interventions were carried out first 3 months for both intervention groups 1 and 2. The next 3 months were a follow-up period without any interventions and interaction by any other study team. Assessments of all variables were made at baseline, 3 months, and 6 months among all three groups. The primary outcome was glycosylated hemoglobin (HbA1c) and the secondary outcomes were BMI, waist circumference, blood pressure, lipid profile (total cholesterol, LDL, HDL, triglycerides).
Ethical considerations
This study was approved by the Ethics Review Committee, Faculty of Health Care Sciences, Eastern University, Sri Lanka (No: E2018/32). Written informed consent was obtained from each participant before the study. The anonymity of the participants and confidentiality of the data was maintained throughout the study.
Statistical analysis
Analysis of quantitative study data, including assessment of changes in primary and secondary outcomes, was conducted in SPSS, version 21.
A probability of <0.05 was considered statistically significant for all tests. The baseline data of each group were described using frequency distributions and mean with standard deviations (SD).
A statistically significant difference of categorical variables among the 3 groups at baseline was assessed by using the chi-square test.
Continuous variables were tested for normality by using the skewness and kurtosis value of the distribution.
Comparisons of a mean of primary and secondary outcomes between all three groups at baseline, postinterventions, and differences between post-intervention were assessed by using one-way ANOVA.
Observations are normally distributed, homogeneity of variance (the population variances are equal) and the 3 groups are independent random samples were the assumptions of the ANOVA test.
Results
Baseline characteristics of participants
The mean age of the study participants in group I was significantly higher than group II. More than 75% of study participants were females in each group. Mean systolic blood pressure (SBP) was higher in group III when compared to group I and II.
A statistically significant difference was observed in the SBP across the 3 groups (p=0.021). None of the sociodemographic factors showed a statistically significant difference among the 3 groups (p>0.05) except age and SBP (Table1).
| Variables | Group I (n=45) n (%) | Group II (n=45) n (%) | Group III (n=45) n (%) | p value |
|---|---|---|---|---|
| Age (mean ± SD) years | 58.40 (4.68) | 53.04 (9.87) | 57.33 (7.34) | 0.003$ |
| Gender | ||||
| Male | 10 (22.2) | 11 (24.4) | 9 (20.0) | 0.879a |
| Female | 35 (77.8) | 34 (75.6) | 36 (80.0) | |
| Marital status | ||||
| Married | 38 (84.4) | 35 (77.8) | 35 (77.8) | 0.659a |
| Unmarried | 7 (15.6) | 10 (22.2) | 10 (22.2) | |
| Smoking | ||||
| Yes | 4 (8.9) | 2 (4.4) | 3 (6.7) | 0.700a |
| No | 41 (91.1) | 43 (95.6) | 42 (93.3) | |
| Current treatment | ||||
| OHA only | 38 (84.4) | 40 (88.9) | 36 (80.0) | 0.432# |
| Insulin Only | 3 (6.7) | 1 (2.2) | 1 (2.2) | |
| Both | 4 (8.9) | 4 (8.9) | 8 (17.8) | |
| SBP (mean ± SD) | 125.33 (13.75) | 124.00 (12.50) | 131.20 (12.30) | 0.021$ |
| DBP (mean ± SD) | 79.56 (6.01) | 78.44 (7.06) | 80.67 (6.88) | 0.290$ |
| Present comorbidities | ||||
| Hypertension | 30 (66.7) | 31 (68.9) | 22 (48.9) | 0.102a |
| Bronchial Asthma | 9 (20.0) | 9 (20.0) | 8 (17.8) | 0.953a |
| Ischemic Heart Disease | 3 (6.7) | 8 (17.8) | 5 (11.1) | 0.260a |
| Ischemic Stroke | 1 (2.2) | 0 (0.0) | 0 (0.0) | 0.331# |
| Anthropometric details | ||||
| Weight (kg) | 63.20 (10.94) | 67.90 (13.67) | 65.65 (10.33) | 0.169$ |
| Height (cm) | 152.01 (8.26) | 155.18 (11.65) | 153.83 (7.37) | 0.271$ |
| BMI (Kg/m2) | 27.43 (4.91) | 28.28 (5.44) | 27.73 (3.88) | 0.694$ |
| WC (cm) | 93.76 (9.31) | 95.54 (9.85) | 93.93 (17.35) | 0.763$ |
| Laboratory blood results | ||||
| HbA1c (%) | 8.20 (1.45) | 8.43 (1.52) | 8.52 (1.37) | 0.564$ |
| TC (mg/dl) | 180.07 (42.58) | 165.36 (45.10) | 170.40 (34.80) | 0.229$ |
| TG (mg/dl) | 123.64 (42.79) | 125.53 (52.97) | 125.67 (47.70) | 0.975$ |
| HDL (mg/dl) | 47.82 (10.21) | 46.11 (9.67) | 45.69 (9.29) | 0.547$ |
| LDL (mg/dl) | 107.04 (38.35) | 91.38 (36.86) | 96.84 (34.09) | 0.122$ |
| TC/HDL | 3.90 (1.14) | 3.70 (1.20) | 3.82 (1.15) | 0.683$ |
| LDL/HDL | 2.34 (0.97) | 2.04 (0.85) | 2.23 (1.01) | 0.303$ |
Table 1: Sociodemographic and clinical characteristics of participants at baseline among 3 groups.
The mean BMI was slightly higher in group II and III when compared to group I at baseline. Group I, II, and III were not significantly different from each other with regards to mean weight, height, Body Mass Index (BMI), and waist circumference.
At baseline, the mean HbA1c of study participants in each group was similar and there was no statistically significant difference in the mean HbA1c between groups I, II, and III.
Further, mean total cholesterol, LDL and HDL were slightly higher in group I than in group II and III. None of the laboratory blood results showed a statistically significant difference among the 3 groups (p<0.05) at baseline (Table1).
Effectiveness of intervention after 3 months of intervention
After 3 months of intervention, the mean HbA1c was lower in group III compared to group I and group II. The mean HbA1c was statistically significant across the groups [F (2, 132)=5.28, p=0.006]. In addition, even though, there was no statistically significant difference in mean BMI and waist circumference, group III had lower BMI and waist circumference compared to other groups. In addition, total cholesterol and LDL cholesterol was lower in group II compared to group I and III. The mean systolic and diastolic blood pressure was lower in group II when compared to group I and III (Table 2).
| Variables | Group I (n=45) | Group II (n=45) | Group III (n=45) | p value$ |
|---|---|---|---|---|
| HbA1c (%) | 7.89 (1.25) | 8.46 (1.87) | 7.46 (1.17) | 0.006 |
| BMI (Kg/m2) | 27.63 (5.20) | 28.31 (5.30) | 26.57 (3.86) | 0.226 |
| WC (cm) | 95.38 (10.13) | 95.83 (18.16) | 94.73 (12.77) | 0.934 |
| SBP (mmHg) | 123.78 (11.93) | 122.89 (12.75) | 126.64 (14.57) | 0.368 |
| DBP (mmHg) | 79.07 (5.96) | 77.33 (7.20) | 77.71 (8.28) | 0.489 |
| TC (mg/dl) | 174.16 (43.42) | 158.51 (43.84) | 168.49 (39.46) | 0.21 |
| Triglyceride (mg/dl) | 124.47 (30.41) | 118.42 (41.00) | 117.78 (38.26) | 0.677 |
| HDL (mg/dl) | 47.93 (11.29) | 46.53 (12.15) | 46.89 (10.02) | 0.827 |
| LDL (mg/dl) | 96.89 (36.22) | 85.73 (33.14) | 100.96 (34.78) | 0.103 |
Table 2: Comparison of primary and secondary outcomes variables at 3 months of intervention among the 3 groups (mean ± SD).
After 3 months of intervention, the mean difference of HbA1c was declined by 1.07 % in group III. A statistically significant difference was observed in the mean differences of HbA1c level across the groups (F (2, 132)=8.84, p=0.000) (Figure 1).
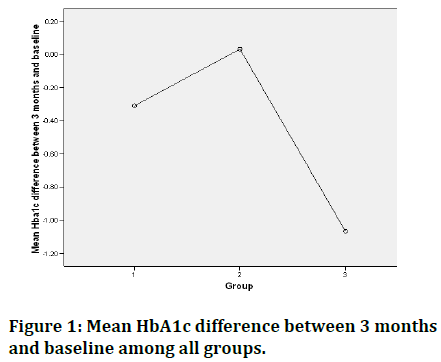
Figure 1. Mean HbA1c difference between 3 months and baseline among all groups.
The higher mean reduction in BMI (1.17 Kg/m2) was observed in group III, but was increased by 0.21 Kg/m2 in group I. Further, the mean difference of BMI was significantly different across the groups (F (2, 132)=5.23, p=0.007).
The mean waist circumference was increased more in group I compared to II and III after 3 months of intervention.
The mean reduction of SBP and DBP was higher in group III when compared to group I and II.
Further, even though, there was no statistically significant difference in a mean reduction of triglyceride level, group III had much reduction of triglyceride level when compared to group I and II (Table 3).
| Variables | Group I | Group II | Group III | p value $ |
|---|---|---|---|---|
| (n=45) | (n=45) | (n=45) | ||
| HbA1c (%) | -0.31 (0.82) | + 0.03 (1.26) | -1.07 (1.59) | 0 |
| BMI (Kg/m2) | +0.21 (0.90) | +0.04 (1.66) | -1.17 (3.30) | 0.007 |
| WC (cm) | +1.90 (3.21) | + 0.29 (15.48) | +0.80 (19.10) | 0.869 |
| SBP (mmHg) | -1.56 (9.75) | - 1.11 (8.58) | -4.56 (17.17) | 0.362 |
| DBP (mmHg) | -0.49 (5.63) | -1.11 (4.38) | -2.96 (9.88) | 0.228 |
| TC (mg/dl) | -5.91 (26.73) | -6.78 (31.17) | -1.91 (28.03) | 0.688 |
| Triglyceride (mg/dl) | +0.82 (37.66) | -7.11 (43.85) | -10.53 (34.94) | 0.369 |
| HDL (mg/dl) | +0.11 (9.82) | +0.42 (11.04) | +1.20 (9.18) | 0.869 |
| LDL (mg/dl) | -59.11 (38.09) | -44.84 (35.80) | -49.96 (35.10) | 0.173 |
Table 3: Mean differences of primary and secondary outcomes variables between 3 months of intervention and baseline among the 3 groups.
Effectiveness of intervention after 6 months
The Respondent rate was 84.4% (n=38) in group I, 95.6% (n=43) in group II and 86.7% (n=39) in group III at 6 months of intervention. The mean HbA1c level was similar among all three groups at 6 months of intervention. Further, there was no statistically significant difference was observed in the HbA1c level across all three groups. In addition, the mean SBP level was lower among group II when compared to group I and III. There was a statistically significant difference in mean SBP values across the three groups (p=0.014). Also, the mean SBP level was lower among group III when compared to group I and II. There was a statistically significant difference in mean SBP values across the three groups (p=0.036) (Table 4).
| Variables | Group I | Group II | Group III | p value$ |
|---|---|---|---|---|
| (n=38) | (n=43) | (n=39) | ||
| HbA1c (%) | 8.34 (1.96) | 8.67 (2.19) | 8.02 (1.38) | 0.297 |
| BMI (Kg/m2) | 28.06 (4.98) | 27.41 (4.48) | 26.02 (4.42) | 0.385 |
| WC (cm) | 114.78 (36.76) | 96.30 (10.36) | 94.60 (9.98) | 0.41 |
| SBP (mmHg) | 135.26 (17.87) | 125.58 (14.85) | 126.05 (15.75) | 0.014 |
| DBP (mmHg) | 82.11 (11.43) | 78.37 (10.89) | 75.13 (12.74) | 0.036 |
| TC (mg/dl) | 168.97 (58.49) | 154.00 (37.82) | 163.51 (38.44) | 0.372 |
| Triglyceride (mg/dl) | 122.21 (44.39) | 117.16 (57.23) | 127.36 (67.92) | 0.725 |
| HDL (mg/dl) | 41.32 (13.41) | 40.84 (10.87) | 42.64 (14.98) | 0.816 |
| LDL (mg/dl) | 107.03 (45.32) | 87.19 (29.72) | 95.15 (33.61) | 0.054 |
Table 4: Comparison of mean of outcomes variables after 6 months of intervention among the 3 groups (mean ± SD).
After 6 months of intervention from the baseline, the mean difference of HbA1c was declined by 0.33 % in group III, but it was increased in group I and II. There was no statistically significant difference was observed in the mean differences of HbA1c level across the groups (p>0.05). The higher mean reduction in BMI (1.12 Kg/m2) was observed in group II but was increased by 0.12 Kg/m2 in group I and it is not statistically significant. A statistically significant difference was observed in the mean difference of systolic blood pressure across all three groups (F(2,117)=7.125, p=0.001). Similarly, the mean DBP was declined by 5.38 mmHg in group III but increased by 2.37 mmHg in the control group (group I). Further, a statistically significant difference was observed in mean differences of DBP across all three groups [F (2, 117)=3.965, p=0.022] (Table 5).
| Variables | Group I | Group II | Group III | p value $ |
|---|---|---|---|---|
| (n=38) | (n=43) | (n=39) | ||
| HbA1c (%) | + 0.13 (1.13) | + 0.18 (1.66) | -0.33 (1.04) | 0.174 |
| BMI (Kg/m2) | +0.12 (3.35) | -1.12 (3.33) | -1.01 (2.78) | 0.165 |
| WC (cm) | +2.09 (13.54) | - 1.36 (8.54) | +0.93 (16.73) | 0.372 |
| SBP (mmHg) | +9.21 (17.84) | +1.63 (18.24) | -5.84 (16.27) | 0.001 |
| DBP (mmHg) | +2.37 (10.76) | 0.00 (12.53) | -5.38 (13.75) | 0.022 |
| TC (mg/dl) | -11.24 (64.45) | -10.23 (35.39) | -5.08 (20.22) | 0.799 |
| Triglyceride (mg/dl) | -0.74 (33.54) | -6.27 (61.90) | -2.97 (53.46) | 0.888 |
| HDL (mg/dl) | -5.89 (11.00) | -5.51 (8.63) | -2.25 (13.30) | 0.282 |
| LDL (mg/dl) | +1.58 (40.45) | -3.14 (23.87) | +0.03 (19.67) | 0.757 |
Table 5: Mean differences of outcomes variables between 6 months and baseline of intervention among the 3 groups (mean ± SD).
Discussion
The rising epidemic of the increasing prevalence of T2DM and its complications worldwide has been partly attributed to poor dietary habits. This study was conducted to evaluate the effectiveness of a standard dietary intervention and low carbohydrate diet intervention for glycaemic control concerning HbA1c improvement among T2DM patients. The study demonstrated that good glycaemic control among patients with T2DM with reduced HbA1c levels by the health education intervention on a low carbohydrate diet. After 3 months of intervention, the mean difference of HbA1c was declined by 1.07 % in the intervention group with a low carbohydrate diet compared to the control group. The improvement of HbA1c by 1.07% in the present low carbohydrate intervention is clinically significant. According to UKPDS, each 1% reduction in HbA1c level is associated with a 37% reduction in microvascular complications, 14% of reduction in myocardial infarctions, and 21% reduction in diabetesrelated death [26]. At the same time, significant improvement of HbA1c is also associated with substantial improvement in short-term symptoms, quality of life, health, and economic benefits [27]. Similarly, a study conducted to assess the effects of a lowcarbohydrate diet on glycaemic control in outpatients with T2DM found that the low carbohydrate diet over 6 months led to a remarkable reduction in HbA1c levels [17]. In contrast to these findings, a study conducted to assess the effectiveness of an intensive nutritional Intervention in patients with T2DM found that there was no difference was detected between usual care and intervention groups regarding changes in body weight, HbA1c, or other outcome measures, at post-intervention or 1-year follow-up [22].
A meta-analysis study has emphasized that there was a significant reduction in HbA1c level among those who had received low glycaemic (GI) diets (low carbohydrate) compared to high GI diets [28] and a Sri Lankan study concluded that low carbohydrate diets as better choices for the better glycaemic control [29]. Not surprisingly, low carbohydrate diet intervention was most effective in improving mean systolic and diastolic blood pressure (reduced by nearly 5 mmHg) from baseline to 6 months in this study. Drop-in blood pressure has been shown to significant improvement in clinical [30]. A 10 mmHg reduction in SBP and DBP has translated into significant long-term cost-effectiveness [31]. Further, 10 mmHg reduction is associated with a 44% reduction in stroke risk, an increase in life expectancy by 0.47 years, and discounted quality-adjusted a significant reduction of 5 mmHg in SBP among low carbohydrate diet intervention participants compared to the control group. It revealed that low carbohydrate diet intervention participants would be beneficial in improving diabetes outcomes by controlling cardiovascular risk factors.
But, the present study did not reveal any advantage from an intensive standard diet invention carried out based on Dietary Guidelines and Nutrition Therapy for Specific Diseases, Nutrition Division, Ministry of Health, Sri Lanka, 2014 [24] among T2DM patients in terms of changes in glycaemic control, body weight and BMI when compared to control group. Similarly, a study conducted in Greece to assess the effectiveness of the intensive nutritional intervention in patients with T2DM found that there was no difference detected between the control group and intervention groups regarding HbA1c improvement [22]. Patients’ readiness to change their dietary habits has been recognized as one of the factors that may affect clinical improvement. Thus, this kind of nutritional intervention should aim at both providing knowledge and motivating patients to increase their likelihood of following the recommended course of action.
The importance of adopting healthy eating habits has been identified as an essential measure for the prevention of acute and chronic complications in patients with T2DM. Further, the patients’ knowledge of appropriate dietary management about self-care was expanded through this intervention, which would enable them to manage their lives more effectively. This indeed helps to improve attitudes and encourage healthy dietary habits which would improve effective HbA1c control and improved BMI.
Limitations of the study were that changes in self-care behaviors of patients with T2DM due to intervention were not measured objectively as it was difficult to assess the human behaviors as it would be self-reported. Besides, changes in the medication are not studied. Some of the changes in HbA1c are possibly due to the change in the medication either reduction or omission or even addition of medication.
Conclusion
Low carbohydrate diet intervention led to a remarkable reduction in HbA1c levels from baseline to 3 months which indicated the feasibility and sustainable efficacy of the nutritional intervention, coupled with health education among the patients with T2DM. Selfmanagement of diabetes among patients with T2DM through dietary intervention was successful with positive outcomes on glycaemic control and other clinical parameters (p<0.05). Sustainability of glycaemic control after the cessation of dietary intervention cannot be possible (p>0.05) when follow-up is not guided by any resource person. Regular dietary educational programs should be arranged in every clinic to provide dietary instructions and reinforcement should be given to the patients who had improved their glycaemic control by following the dietary advice to motivate other patients also.
Acknowledegements
The authors convey their sincere thanks to the individuals who participated in this study.
Author's Contribution
KTS helped study design/planning, study conduct, and writing and revising the paper. GK helped study design/ planning, study conduct, data analysis, and writing and revising the paper. SK helped study design/planning, study conduct, and revising paper. SIM helped study design/planning, study conduct, and revising paper.
Funding
This work was funded by the Research and publication committee, Eastern University, Sri Lanka.
Conflicts of Interest
The authors have declared that no competing interest exists.
References
- http://apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf;jsessionid=8C44FB53591C2F5F8C0E43FE5CEA0CC9?sequence=1
- https://www.who.int/ncds/surveillance/steps/STEPS-report-2015-Sri-Lanka.pdf
- Siyambalapitiya S, Gunathilake G, Perera I. Exercise: An essential component of diabetes management. Sri Lanka J Diabetes Endocrinol Metabol 2012; 2:57â??60.
- Wild S, Roglic G, Green A, et al. Global prevalence of diabetesâ??Estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27:1047â??1053.
- Katulanda P, Constantine GR, Mahesh JG, et al. Prevalence and projections of diabetes and pre-diabetes in adults in Sri Lanka-Sri Lanka Diabetes, Cardiovascular Study (SLDCS). Diabetes Med 2008; 25:1062-1069.
- American Diabetes Association. Standards of medical care in diabetes: Classification and diagnosis of diabetes. Diabetes Care 2017; 40:S11â??S24.
- Wijesuriya MA. Prevalence of diabetes in Sri Lanka. Ceylon Med J 1997; 17:1- 4.
- Banerji MA, Faridi N, Atluri R, et al. Body composition, visceral fat, leptin, and insulin resistance in Asian Indian men. J Clin Endocrinol Metab 1999; 84:137-144.
- Mather HM, Chaturvedi N, Fuller JH. Mortality and morbidity from diabetes in South Asians and Europeans: 11-year follow-up of the Southall Diabetes Survey, London, UK. Diabetes Med 1998; 15:53-59.
- Knowler WC, Barrett-Connor E, Fowler SE, et al. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England J Med 2002; 346:393-403.
- Stone RA, Sevick MA, Rao RH, et al. The diabetes tele-monitoring study extension: An exploratory randomized comparison of alternative interventions to maintain glycaemic control after withdrawal of diabetes home tele-monitoring. J Am Med Informatics Assoc 2012; 19:973â??979.
- Karanja L. Dieticiansâ?? knowledge of diabetic management and patients recovery rate. Sch J Appl Med Sci 2015; 3:431â??435.
- Moran, M. The evolution of the nutritional management of diabetes. Proc Nutr Soc 2004; 63:615â??620.
- Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr 2013; 97:505-516.
- Westman EC, Feinman RD, Mavropoulos JC, et al. Low-carbohydrate nutrition and metabolism. Am J Clin Nutr 2007; 86:276-284.
- Accurso A, Bernstein RK, Dahlqvist A, et al. Dietary carbohydrate restriction in type 2 diabetes mellitus and metabolic syndrome: Time for a critical appraisal. Nutr Metab 2008; 5:9-16.
- Haimoto H, Iwata M, Wakai K, et al. Long-term effects of a diet loosely restricting carbohydrates on HbA1c levels, BMI and tapering of sulfonylureas in type 2 diabetes: A 2-year follow- up study. Diabetes Res Clin Pract 2008; 79:350-356.
- Boden G, Sargrad K, Homko C, et al. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. Ann Intern Med 2005; 142:403-11.
- Evert AB, Boucher JL, Cypress M, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2014; 37:S120-S142.
- Williamson AR, Hunt AE, Pope JF, et al. Recommendations of dietitians for overcoming barriers to dietary adherence in individuals with diabetes. Diabetes Educ 2002; 26:272â??279.
- Donner A. Approaches to sample size estimation in the design of clinical trials-A review. Statistics Med 1984; 3:199-214.
- Yannakoulia M, Poulia K, Mylona1 E, et al. Effectiveness of an intensive nutritional intervention in patients with type 2 diabetes mellitus: Results from a pilot study. Review Diabetic Studies 2007; 4:226-230.
- Fan R, Xu M, Wang J, , et al. Sustaining effect of intensive nutritional intervention combined with health education on dietary behavior and plasma glucose in type 2 diabetes mellitus patients. Nutrients 2016; 8:560.
- https://www.google.lk/webhp?sourceid=chrome-instant&rlz=1C1CHZL_enLK682LK682&ion=1&espv=2&ie=UTF-8#q=Dietary+Guidelines+%26+Nutrition+Therapy+for+Specific+Diseases,
- Norris SL, Lau J, Smith SJ, et al. Self-management education for adults with type 2 diabetes: A meta-analysis of the effect on glycaemic control. Diabetes Care 2002; 25:1159â??71.
- Stratton IM, Adler AI, Neil HA, et al. Association of glycemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ 2000; 321:405â??412.
- Holtrop JS, Hickner J, Dosh S, et al. Sticking to itâ??diabetes mellitus, a pilot study of an innovative behavior change program for women with type 2 diabetes. Am J Health Educ 2002; 33:161-166.
- Thomas DE, Elliott EJ. The use of low-glycaemic index diets in diabetes control. Br J Nutr 2010; 104:797-802.
- Pirasath S, Balakumar B, Arasaratnam, V. Glycaemic Index of Sri Lankan Meals. J Blood Disorders Transf 2015; 6:254.
- Philis-Tsimikas A, Formann A, Ocana LL, et al. Peer led diabetes education programs in high risk Mexican Americans improve glycaemic control compared with standard approaches: a Project Dulce promotora randomized trial. Diabetes Care 2011; 34:1926â??31.
- Gabbay RA, Lendel I, Saleem TM, et al. Nurse case management improves blood pressure, emotional distress and diabetes complication screening. Diabetes Res Clin Prac 2006; 71:28-35.
Author Info
Sundaresan Thadchanamoorthy, Kisokanth Gnanaselvam*, Kumanan Somasuriyam and Majitha Seyed Ibrahim
1Department of Clinical Sciences, Faculty of Health Care Sciences, Eastern University, Sri Lanka2Department of Clinical Nursing, Faculty of Nursing, University Colombo, Sri Lanka
3Teaching Hospital, Batticaloa, Sri Lanka
4Teaching Hospital, Batticaloa, Sri Lanka
Received: 14-Jul-2021 Accepted: 25-Aug-2021
