Research - (2022) Volume 10, Issue 12
Does Maxillomandibular Advancement (MMA) for Obstructive Sleep Apnea (OSA) Negatively Affects Facial Appearance?
*Correspondence: Basem T Jamal, Department of Oral & Maxillofacial Surgery/Head and Neck Surgical Oncology, King Abdulaziz University, Jeddah, Saudi Arabia, Email:
Abstract
Introduction: Maxillomandibular advancement (MMA) is a known surgical option in the management of obstructive sleep apnea that results in a widening of the posterior airway by stretching the oropharyngeal soft tissues. While MMA has a high success rate of 85-95%, such large advancements can change the facial esthetics. The aim of the present study is to examine the rate of satisfaction with facial aesthetics after an intervention with MMA. Materials & Methods: Retrospective analysis of the records of patients who underwent MMA by the author was reviewed. The parameters assessed included age, medical history, preoperative apnea/hypopnea index (AHI), jaw skeletal classification, and satisfaction with facial esthetic. All patients underwent MMA with an advancement of the maxilla ranging from 8-10mm with a counter-clockwise rotation to further expand the airway, the mandible following the maxilla while keeping the patient occlusion and a Genioglossus advancement ranging from 8-10mm. Results: Six patients’ records were reviewed. All patients were males and the average ago was 42. All patients had severe obstructive splee apnea with a mean AHI of 58.6. Four of the patients were satisfied with the change in their facial appearance postoperatively. The two class II patients were indifferent about the facial change and so no patient was dissatisfied with their facial appearance. Conclusion: The study supports the literature findings that MMA for OSA rarely negatively affects patients' perceptions of their facial appearance.
Keywords
MMA, OSA, Facial appearance
Introduction
The term obstructive sleep apnea (OSA) refers to a sleep disorder in which there are episodes of partial (hypopnea) or complete (apnea) reductions in breathing while asleep. The incidence of OSA in men ranges from 2 to 4% [1,2], among women from 1 to 2% [3], and in adults from 5 to 25% [4,5]. Several adverse health effects are associated with OSA in adults, including cardiovascular, neurological, and endocrine complications. Untreated disease can have a significant impact on one's overall health and quality of life over the long term [6].
One of the surgeries proposed to treat obstructive sleep apnea is maxillomandibular advancement (MMA). It results in a widening of the posterior airway by stretching the oropharyngeal soft tissues and MMA achieves that via advancement of the facial skeleton [7]. MMA has a success rate of 85-95% [8]. With such large advancements, facial esthetics will change and patients' demographics and backgrounds can influence whether these changes are advantageous or unfavorable [9].
In the present study, the aim is to examine the rate of satisfaction with facial aesthetics after an intervention with MMA.
Materials and Methods
Retrospective analysis of the records of patients who undergo MMA by the author was reviewed. The parameters assessed included age, medical history, preoperative apnea/hypopnea index (AHI), jaw skeletal classification, and satisfaction with facial esthetics. All patients underwent MMA with an advancement of the maxilla ranging from 8-10mm with a counter-clockwise rotation to further expand the airway, the mandible following the maxilla while keeping the patient occlusion and a genioglossus advancement ranging from 8-10mm. the patients had a brief ICU stay ranging from 1-2 days followed by observation at the regular floor before discharge.
Table 1 shows the patient information. Figure 1 shows panoramic x-rays before and after MMA. Figure 2 shows cephalometric x-rays before and after MMA illustrating the change in airway volume following the procedure.
| Patient | Age | AHI | Medical History | Jaw skeletal classification | satisfaction |
|---|---|---|---|---|---|
| 1 | 62 | 58 | CAD-CABG | Class I | Satisfied |
| 2 | 50 | 62 | CAD-CABG | Class I | Satisfied |
| 3 | 39 | 58 | HTN | Class II | Indifferent |
| 4 | 35 | >60 | Otherwise healthy | Class I | Satisfied |
| 5 | 32 | 60 | Otherwise healthy | Class II | Indifferent |
| 6 | 36 | 54 | Otherwise healthy | Class I | Satisfied |
Table 1: Summary of patients AHI and facial appearance satisfaction.
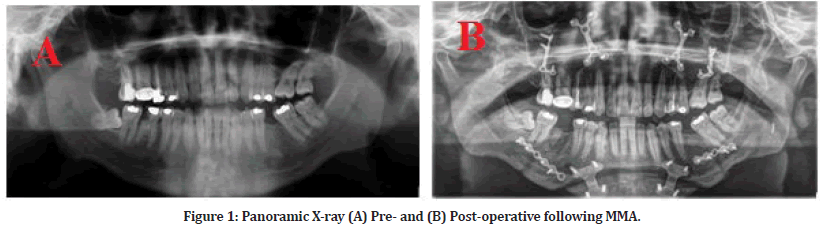
Figure 1: Panoramic X-ray (A) Pre- and (B) Post-operative following MMA.
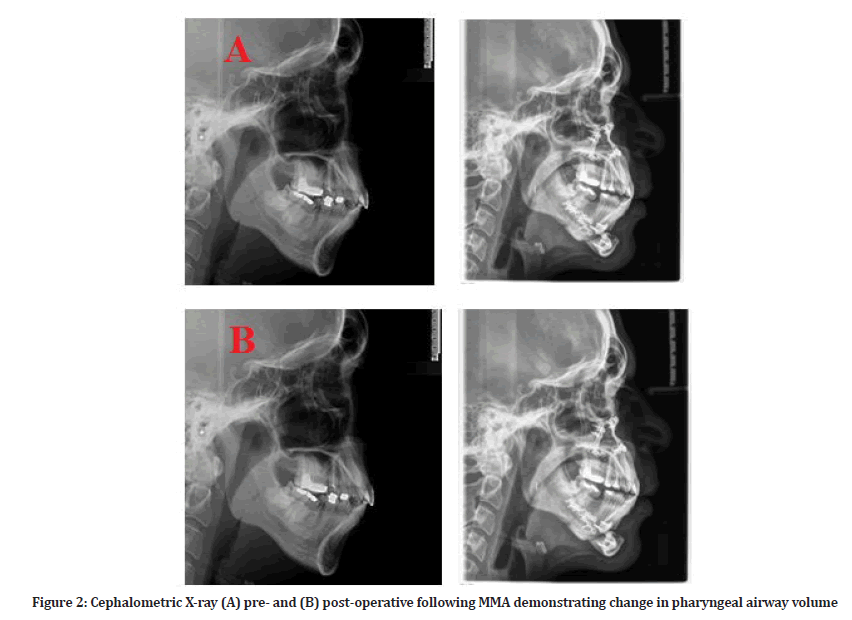
Figure 2: Cephalometric X-ray (A) pre- and (B) post-operative following MMA demonstrating change in pharyngeal airway volume.
Results
Six patients’ records were reviewed. All patients were males and the average ago was 42. All patients had severe obstructive sleep apnea with a mean AHI of 58.6. Five of the patients underwent MMA as the first line of treatment for their OSA. One of the patients had phase 1 treatment in the form of genioglossus advancement but with persistent symptoms, MMA was later performed.
Two of the patients had coronary artery disease (CAD) and coronary artery bypass graft (CABG) performed prior to the surgery as a result of uncontrolled hypertension. One patient had hypertension and the remaining patients were otherwise healthy except for the symptoms associated with severe OSA ranging from excessive daytime fatigue, insomnia, sexual dysfunction, and marital discord. 2 of the patients had a jaw class II skeletal classification with protrusive maxilla preoperatively and were at higher risk of having unfavorable facial esthetic results postoperatively.
All patients reported improvement in their OSA symptoms postoperatively. Four of the patients were satisfied with the change in their facial appearance postoperatively and the two class II patients were indifferent about the change. They did not report dissatisfaction or concern about the change and all patients indicated they would recommend this surgery to other patients.
Discussion
MMA is designed to increase the pharyngeal volume and the size of the airway; however the soft tissues of the face and therefore the appearance of the face will also change as a result of the jaw skeletal movement. The soft tissues of the face follow the skeletal advancement up to 90% in the anteroposterior dimension [9,10]. A large maxillary advancement may result in unaesthetic changes that include significant upturning of the nasal complex and considerable fullness of the nasolabial region [11-13].
The patients seeking treatment for OSA are not interested in esthetic facial improvement; however they are concerned about the possibility of deformity as a result of this treatment modality. A balance must be achieved between the therapeutic goals and the aesthetic outcomes in order to maximize patient satisfaction.
There have been some studies that have assessed the perception of facial aesthetic outcomes following MMA surgery for OSA with overall positive results [11]. Sixty-nine percent of patients were satisfied or neutral with the outcome of their surgery, according to Islam et al [14]. Li et al. [15] study reported 90% patient satisfaction with the aesthetic outcome. According to a study by Emanuele, et al. only 9% of patients reported a decrease in their attractiveness as a result of MMA surgery [16]. In the literature, a range of 9 to 31% of patients has expressed dissatisfaction with their appearance following surgery [17].
The current study shows similar findings to the existing literature, with all patients indicating either positive or neutral response to their facial appearance following surgery. Different cultures have different beauty standards, but a pronounced jaw line and prognathic mandible are considered attractive features for both men and women nowadays and MMA accomplishes just that.
Understandably, patients with class II skeletal deformity with existing maxillary protrusion are not expected to have improved facial esthetics following MMA. Even so, these two patients were indifferent to the resulting facial appearance, indicating an increased benefit from surgery over any potential cosmetic change.
Conclusion
Finally, the study supports the literature findings that MMA for OSA rarely negatively affects patients' perceptions of their facial appearance. In fact, most patients report an improvement in their facial appearance as a result of this procedure.
References
- Knudsen TB, Laulund AS, Ingerslev J, et al. Improved apnea-hypopnea index and lowest oxygen saturation after maxillomandibular advancement with or without counterclockwise rotation in patients with obstructive sleep apnea: A meta-analysis. J Oral Maxillofac Surg 2015; 73:719–726.
- Boyd SB, AS Walters, Y Song, et al. Comparative effectiveness of maxillomandibular advancement and uvulopalatopharyngoplasty for the treatment of moderate to severe obstructive sleep apnea. J Oral Maxillofac Surg 2013; 71:743-751.
- Holty JEC, Guilleminault C. Maxillomandibular advancement for the treatment of obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med Rev 2010; 14:287–297.
- Campbell, Reynolds G, Trengrove H, et al. Mandibular advancement splint titration in obstructive sleep apnoea. Sleep and Breath 2008; 13:157–162.
- Yu CC, Hsiao HD, Lee LC, et al. Computational fluid dynamic study on obstructive sleep apnea syndrome treated with maxillomandibular advancement. J Craniofac Surg 2009; 20:426-430.
- Rohde K, Verse T. Sleep disordered breathing. Sur Sleep Disord Breath 2010; 1–3.
- Schendel SA, Broujerdi JA, Jacobson RL. Three-dimensional upper-airway changes with maxillomandibular advancement for obstructive sleep apnea treatment. Am J Orthod Dentofacial Orthop 2014; 146:385–393.
- Rojo-Sanchis C, Almerich-Silla JM, Paredes-Gallardo V, et al. Impact of bimaxillary advancement surgery on the upper airway and on obstructive sleep apnea syndrome: A meta-analysis. Sci Rep 2018; 8:5756.
- Cohen-Levy J, Petelle B, Vieille E, et al. Changes in facial profile after maxillomandibular advancement surgery for obstructive sleep apnea syndrome. Int Orthod 2013; 11:71–92.
- Joss CU, Joss-Vassalli IM, Kiliaridis S, et al. Soft tissue profile changes after bilateral sagittal split osteotomy for mandibular advancement: A systematic review. J Oral Maxillofac Surg 2010; 68:1260-1269.
- Li KK, RW Riley, NB Powell, et al. Maxillomandibular advancement for persistent obstructive sleep apnea after phase I surgery in patients without maxillomandibular deficiency. Laryngoscope 2000; 110:1684-1688.
- Islam S, Aleem F, Ormiston IW. Subjective assessment of facial aesthetics after maxillofacial orthognathic surgery for obstructive sleep apnoea. Br J Oral Maxillofac Surg 2015; 53:235–238.
- Gil APS, Machado-Fernández A, Guijarro-Martínez R, et al. Le fort I osteotomy and soft tissue response: A retrospective cohort study comparing three different techniques. J Craniomaxillofac Surg 2022; 50:107–113.
- Islam S, Uwadiae N, Ormiston IW. Orthognathic surgery in the management of obstructive sleep apnoea: experience from maxillofacial surgery unit in the United Kingdom. Br J Oral Maxillofac Surg 2014; 52:496–500.
- Li KK, RW Riley, Powell NB, et al. Patient's perception of the facial appearance after maxillomandibular advancement for obstructive sleep apnea syndrome. J Oral Maxillofac Surg 2001; 59:377-380.
- Emanuele AD. Quality of life and subjective outcomes following maxillomandibular advancement surgery for the treatment of obstructive sleep apnea. Electron Thesis Diss Repos 2015.
- Beranger T, Garreau E, Ferri J, et al. Morphological impact on patients of maxillomandibular advancement surgery for the treatment of obstructive sleep apnea-hypopnea syndrome. Int Orthod 2017; 15:40–53.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Department of Oral & Maxillofacial Surgery/Head and Neck Surgical Oncology, King Abdulaziz University, Jeddah, Saudi ArabiaReceived: 14-Nov-2022, Manuscript No. jrmds-22-79750; , Pre QC No. jrmds-22-79750(PQ); Editor assigned: 16-Nov-2022, Pre QC No. jrmds-22-79750(PQ); Reviewed: 30-Nov-2022, QC No. jrmds-22-79750(Q); Revised: 05-Dec-2022, Manuscript No. jrmds-22-79750(R); Published: 12-Dec-2022
