Research - (2021) Volume 9, Issue 6
Doppler Study in Gestational Hypertension and Perinatal Outcome-A Prospective Study
A Padmaja Rani, K Saraswathi and K Vani*
*Correspondence: K Vani, Department of Obstetrics & Gynecology, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
A prospective, randomized study was designed to study the variation in the Uterine, Umbilical and Middle Cerebral artery blood flow pattern in Gestational Hypertension and Preeclampsia. The Present study focuses on to evaluate the efficacy of Doppler velocimetry in early diagnosis of fetal hypoxia and to decide about the time and mode of termination in gestational hypertension and preeclampsia.
Keywords
Gestational hypertension, Preeclampsia, Uterine, Cerebral artery, Doppler velocimetry
Introduction
Hypertension is a common medical disorder of pregnancy approximately 70% of which are primigravidas. Preeclampsia is characterized by an imbalance between prostacycline and thromboxane production [1-4], as well as failure of the second wave trophoblastic invasion of the endometrio-myometrial vasculature. The result is abnormal uteroplacental blood flow, and this has led to the idea of using color Doppler in the evaluation and management of PIH patients. Doppler ultrasound evaluation of the mother and fetus with the study of blood flow indices provides non-invasive assessment to study uteroplacental circulation and fetoplacental circulation and hemodynamic changes and adaptation in the fetal organs in response to hypoxemia; with this, the degree of placen 1 dysfunction can be studied to know the severity of the disease.
Doppler is useful in selecting the patients for induction and trial of labor, also helps in making decisions when to intervene without increasing fetal risk. This in its effect contributes to lowering maternal morbidity and also neonatal morbidity and lowers the incidence of Caesarean sections and admission to NICU care, and incidence of prematurity. Among high risk patients, several studies suggested a significant decrease in neonatal morbidity and mortality when Doppler evaluation was a part of fetal surveillance [5]. Quality of life for both mother and the new-born has now rightly become our top priority in the field of obstetrics. It is apparent that no greater services can be provided, than ensuring that each new born is well born. The common cause of maternal morbidity and mortality are Hypertensive disorders complicating pregnancy, Haemorrhage and Infection form the deadly triad that contribute greatly to maternal morbidity and mortality. Hypertensive disorders completing pregnancy has been a recognized pathological entity since the time of Hippocrates and ancient Greeks [1]. Hypertensive disorders in pregnancy are one of the major causes of maternal and perinatal mortality and morbidity. It is one of the commonest medical disorders diagnosed by obstetricians in clinical practice [2]. It is said that pregnancy induced hypertension (PIH) contributes to death of a woman every 3 minutes worldwide3.According to National Centre for Health Statistics, Gestational hypertension was identified in 3.7% of pregnancies. It is one of the commonest medical disorders diagnosed by obstetricians in clinical practice [2].
Pregnancy is a high-flow, low resistance state of cardiovascular haemostasis associated with remarkable hemodynamic changes. A progressive fall of vascular resistance in the uterine, placental and umbilical arteries is evident with increasing gestational age, producing high end-diastolic flow. In uteroplacental circulation the main uterine artery is a branch of the internal iliac artery. At the level of the internal os of cervix, it bifurcates into the descending (cervical) and ascending (corporal) branches. At the uterine tubal junction, the ascending branch anastomoses with the ovarian artery to form an arterial arcade. The tortuous accepting uterine artery gives off approximately eight branches of arcuate arteries, which then traverses the outer one-third of the myometrium. The impedance to blood flow in both uterine arteries decreases gradually from early pregnancy until the end of second trimester. More dramatic changes occur in the second trimester, when the uterus begins to grow rapidly, thereby uncoiling the main uterine and spiral arteries. Between 26 and 28 weeks of gestation, uterine arteries reach their maximal dilatation and minimal resistance [6-37].
The uteroplacental flow increases throughout pregnancy from approximately 50 ml/min during early pregnancy up to 450-600 ml/min near term. During normal pregnancy, the trophoblastic cells enter the lumen of the spiral arteries, partially replacing the endothelium and progressing down up to the level of the endometrium. By 16-22 weeks gestation, trophoblasts migrates along the entire length (intramyometrial portion) of the spiral arteries and strips it of its muscular elastic coat [38].
This transformation leads to formation of a low resistance vascular system, progressing from the radial artery into the intervillous spaces; the pressure falls about 70 to 80 mm Hg in the former to 10 mm Hg in the latter. In fetoplacental circulation during fetal life oxygenation is carried out in placenta. The tortuous umbilical cord is the lifeline of fetus. It has two umbilical arteries and one umbilical vein. A considerable amount of oxygenated blood returning from the placenta through the umbilical vein is directed through the ductus venosus to the inferl:"vf vena cava into the right atrium, through the foramen ovale, this oxygenated blood is directed to the left atrium and then to the left ventricle. Blood from the right ventricle is ejected either into the pulmonary circulation or through the ductus arteriosus into the descending aorta.
The blood returns to the fetus by the umbilical vem, emptying into the portal sinus. Then the major portion of the blood passes through ductus venosus to inferior vena cava, just before it enters into the right atrium. Blood flow through the fetal heart is "parallel" rather than "serial" because of the presence of ductus arteriosus between the pulmonary trunk and the aorta. Both the ventricles eject blood into the aorta simultaneously rather than blood moving first through the right ventricle, then the pulmonary circulation, and finally the left ventricle as in the adult. The blood returns to the fetus by the umbilical vein, emptying into the portal sinus. Then the major portion of the blood passes through ductus venosus to inferior vena cava, just before it enters into the right atrium. About 50% of inferior vena caval hlpod passes directly through the foramen ovale into the left atrium to mix up with pulmonary blood and then enters the left ventricle. Well oxygenated blood from the left ventricle is directed through the ascending aorta to supply the coronary arteries and the upper body organs, thus preferentially perfusing the brain. This blood enters pulmonary artery, which is in direct continuity with descending aorta via ductus arteriosus and perfuses the lower body and placenta.
The fetal cerebral blood flow is of a high impedance, low flow circulation. It is a more sensitive parameter of fetal oxygenation status than umbilical blood flow. The increase in the diastolic component as the pregnancy progresses is interpreted as decrease in cerebral resistance due to brain development. This increase in diastolic component begins later in the cerebral arteries (at approximately 25 weeks) than in umbilical arteries (approximately 15 weeks) [39-46].
Materials and Methods
This is a prospective study conducted on hundred patients with clinically diagnosed pregnancy induced hypertension for the evaluation of the effectiveness of Doppler studies in hypertension complicating pregnancy with relevance to perinatal outcome undertaken at Sree Balaji Medical College and Hospital, Chromepet, Chennai, in the Department of Obstetrics and Gynaecology, during the period from August 2010 to September 2012.
Inclusion criteria
All antenatal cases more than 26 weeks of gestation clinically diagnosed as pregnancy induced hypertension.
Exclusion criteria
• All antenatal cases with chronic hypertension.
• All antenatal cases less than 26 weeks of gestation clinically diagnosed as pregnancy induced hypertension.
• All antenatal cases with abnormal Doppler findings without pregnancy induced hypertension.
• Intrauterine death at the time of first Doppler examination.
• Patients who cannot be followed up.
The first scan was performed in each case, as soon as the patient was registered in order to avoid any influence of treatment on Doppler sonogram. The gestational age was confirmed by menstrual history and ultrasound examination and was followed by color Doppler examination.. Consent was taken from the patient or the guardian.
Method of study
In all patients, a thorough general and obstetric history was elicited and a complete general and obstetric examination was done. All the patients were monitored and for four hourly blood pressure recordings, daily urine analysis, twice weekly blood urea and uric acid and fundus examination. Liver function tests, platelet count, electrolytes, complete hemogram were done once in a week. These investigations were repeated as and when necessary till delivery. Fetal surveillance was done with daily fetal movement count, twice weekly NST and modified Biophysical profile. Further management was done depending upon the severity of preeclampsia and condition of the cervix. USG and Doppler flow velocimetry of umbilical, uterine artery and middle cerebral artery were studies at term, and the mode of delivery, fetal outcome werestudied documented and analysed.
Doppler study was performed in a prospective study. In the obstetric examination, uterine fundal height and abdominal girth were measured. Fetal heart rate counted.
IUGR was diagnosed if there is > 2cm difference in Symphysio fundal height to the clinical gestational age.
Procedure
The patient was explained about the non-invasive/ atraumatic nature of the procedure. Synthetic ultra-gel was applied liberally over the abdomen to get a good acoustic coupling. The instruments used were Hitachi EUB 5500, Hitachi EUB 7000, Philips Envisor HD C-1.3 Color Doppler ultrasound machine with a convex transducer of2-5: Ml-Iz frequency. Doppler wave form was obtained after localising the vessels by B-mode real time scanner. Pulsed Doppler was used to get the Doppler signals after localising the vessels. The maximum Doppler shift frequencies were obtained and various ratios were calculated from each vessel. Doppler examination was done when foetus was in apnoeic state to avoid the influence of fetal respiration on Doppler signals.
Identification of various arteries and their criteria
Uterine artery
Color Doppler facilitates identification of the uterine artery substantially. The uterine signal was obtained per abdomen by pointing the probe in the iliac fossa towards the lower para-cervical area. In the color mode, the uterine artery is seen to cross the external iliac artery, just after its origin frff the internal iliac artery and this point were taken as the sampling point. SID >2.6, RI > 0.58 and persistent early diastolic notch is considered abnormal.
Umbilical artery
Flow velocity waveforms from umbilical artery can be easily obtained, for this color flow is not usually needed. Doppler signals can be acquired from different points in cord, usually from midportion of cord. SID ratio of umbilical artery >3, Rl>0.7, presence of absent end diastolic velocity (AEDV) and reversed end diastolic velocity (REDV) were considered abnormal.
Middle cerebral artery (MCA)
MCA was visualized in transverse axial view of fetal head at a slightly more caudal plane than the one used for BPD. PI <1.3 and RI <0.7 were considered abnormal.
Follow up of cases
Maternal indications for termination of pregnancy included uncontrolled hypertension, abruption, deteriorating renal function and HELLP syndrome.
Fetal indications for termination - Evidence of fetal distress either by Biophysical profile or abnormal CTG.
The mode of delivery, Gestational age at delivery, whether delivery was Induced or spontaneous were noted. If induced, indication for Termination/mode of delivery-Labor Natural/elective/emergency LSCS were noted. The following were taken as adverse perinatal outcome.
• Preterm delivery.
• Birth weight < 10th percentile below the mean for gestational age.
• APGAR at 5 minutes< 7/10.
• Caesarean section done for fetal distress.
• Admission to NICU.
• Presence of Respiratory Distress, Hypoxic ischemic encephalopathy, intraventricular haemorrhage, Necrotising enterocolitis, seizures.
• Perinatal deaths.
Results
In the present study, out of 100 cases of Hypertension Complicating Pregnancy, 58cases showed positive Doppler indices in any of the three vessels studied. The remaining 42 cases showed normal Doppler indices in all the three vessels studied. The following were the results of the study. From our present study, age group 20-24 years was the common group. The mean maternal age was 25.46 years (Table 1). In the present study, 59 % were prum gravitas, 41% were multigravidas (Table 2).
| Age group (years) | No. of cases | Percentage (%) |
|---|---|---|
| <20 | 6 | 6 |
| 20-24 | 39 | 39 |
| 25-29 | 35 | 35 |
| 30 | 20 | 20 |
| Total | 100 | 100 |
Table 1: Age distribution of cases.
| Gravidity | No. of cases | Percentage (%) |
|---|---|---|
| Primi | 59 | 59 |
| GIi | 20 | 20 |
| G III | 11 | 11 |
| GIV&V | 10 | 10 |
| Total | 100 | 100 |
Table 2: Gravidity and gestational hypertension.
Out of the 100 cases studied 46% constituted gestational hypertension cases. Mild preeclampsia was seen in 28% of the cases, while severe preeclampsia is seen in 24% of the cases. Eclampsia occurred in 3% of cases. A widely quoted study by Friedman and Neff (1976) showed thatdiastolic hypertension of >95 mmHg was associated with 3 fold increase in fetal death (Table 3).
| Type | No. of Cases | Percentage (%) |
|---|---|---|
| Gestational hypertension | 46 | 46 |
| Mild preeclampsia | 28 | 28 |
| Severe preeclampsia | 24 | 24 |
| Eclampsia | 3 | 3 |
| Total | 100 | 100 |
Table 3: Type of hypertension complicating pregnancy.
After studying three arteries, patients were classified into normal and abnormal based on their color Doppler indices. Normal was those with no abnormality in any of the arteries (Table 4). Cases that had any of the following criteria were considered abnormal:
| Type of complication | No. of cases | Percentage |
|---|---|---|
| Anaemia | 18 | 18 |
| Oligohydramnios | 28 | 28 |
| Accidental Haemorrhage | 6 | 6 |
| Eclampsia | 3 | 3 |
| Rh-negative | 2 | 2 |
Table 4: Other complications coexisting.
• SID ratio >2.6 or RI >0.58 of Uterine Artery.
• Presence of persistent Early Diastolic Notch m Uterine Artery.
• SID ratio of>3 or RI 0.7 of Umbilical Artery.
• Presence of Absent End Diastolic Velocity (AEDV) of Reversed End Diastolic Velocity (REDV).
• PI <1.3 and RI <0.7 of Middle Cerebral Artery.
In present study, 58 cases (58%) had abnormal Doppler indices (Table 5).
| Doppler | Number | Percentage (%) |
|---|---|---|
| Normal | 42 | 42 |
| Abnormal | 58 | 58 |
| Total | 100 | 100 |
Table 5: Normal and abnormal doppler wise distribution of cases.
The table shows more than 50% of cases with elevated SID ratio (Table 6 and Figure 1). The table shows 74% of cases with abnormal RI in this study (Table 7 and Figure 2). About 72% of the cases had normal umbilical artery SID ratio (Table 8 and Figure 3).
| SID ratio | No. of cases | Percentage |
|---|---|---|
| Abnormal | 33 | 56.9 |
| Normal | 25 | 43.1 |
| Total | 58 | 100 |
Table 6: Uterine artery SID ratio.
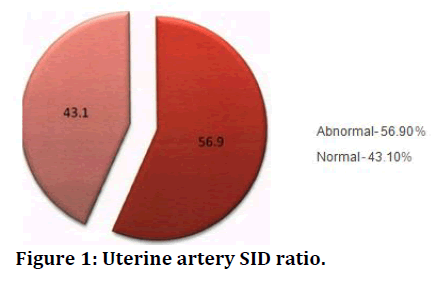
Figure 1. Uterine artery SID ratio.
| Resistance Index | No. of cases | Percentage |
|---|---|---|
| Abnormal | 43 | 74.14 |
| Normal | 15 | 25.86 |
| Total | 58 | 100 |
Table 7: Uterine artery resistance index.
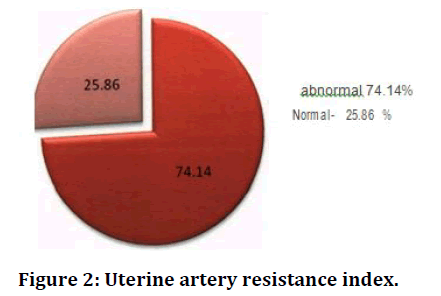
Figure 2. Uterine artery resistance index.
| Umbilical artery SID ratio | No. of cases | Percentage |
|---|---|---|
| Abnormal | 42 | 72.41 |
| Normal | 16 | 27.59 |
| Total | 58 | 100 |
Table 8: Umbilical artery SID ratio.
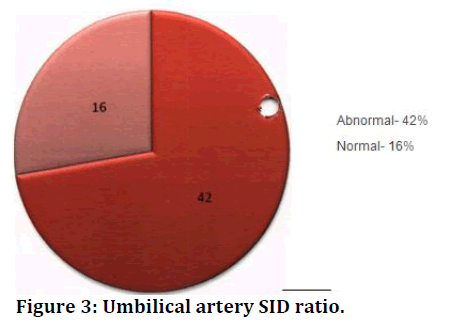
Figure 3. Umbilical artery SID ratio.
Nearly two-third of cases with abnormal doppler show abnormal umbilical artery RI value (Table 9 and Figure 4). In the present study, 8 cases (about 13%) showed absent end diastolic velocity in umbilical artery (Table 10). Uterine artery SID X2 -1.1., umbilical artery X2-nl l. 66., uterine notch X2-1.72 (p<0.01) (Table 11).
| Umbilical artery RI | No. of cases | Percentage |
|---|---|---|
| Abnormal | 36 | 62.06 |
| Normal | 22 | 37.94 |
| Total | 58 | 100 |
Table 9: Umbilical artery resistive index.
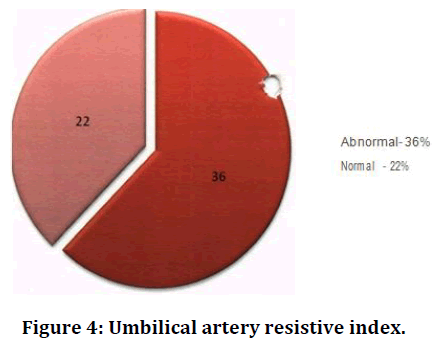
Figure 4. Umbilical artery resistive index.
| Umbilical artery AEDV | No. of cases | Percentage |
|---|---|---|
| Present | 8 | 13 .79 |
| Absent | 50 | 86.21 |
| Total | 58 | 100 |
Table 10: Umbilical artery AEDV.
| SID Ut.A | SID Um.A | Notch | AEDV | |||||
|---|---|---|---|---|---|---|---|---|
| Parameters | No. | % | No. | % | No. | % | No. | % |
| Abnormality present | 33 | 56.9 | 42 | 72.41 | 24 | 41.38 | 8 | 13.79 |
| Abnormality absent | 25 | 43.1 | 16 | 27.59 | 34 | 58.62 | 50 | 86.21 |
| Total | 58 | 100 | 58 | 100 | 58 | 100 | 58 | 100 |
Table 11: Cases with doppler abnormality.
Of the 58 women with abnormal Doppler indices, 55 babies born to them had adverse perinatal outcome in terms of neonatal complications which included birth asphyxia, Meconium aspiration syndrome, hyperbilirubinemia, Respiratory distress syndrome, etc. of the mentioned neonatal complications, majority of them had hyperbilirubinemia-18/55, while it was only 8 babies abnormal Doppler indices had hyperbilirubinemia (Figure 5 to Figure 13).
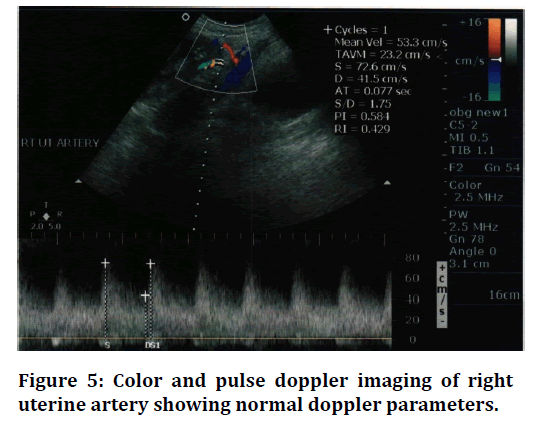
Figure 5. Color and pulse doppler imaging of right uterine artery showing normal doppler parameters.
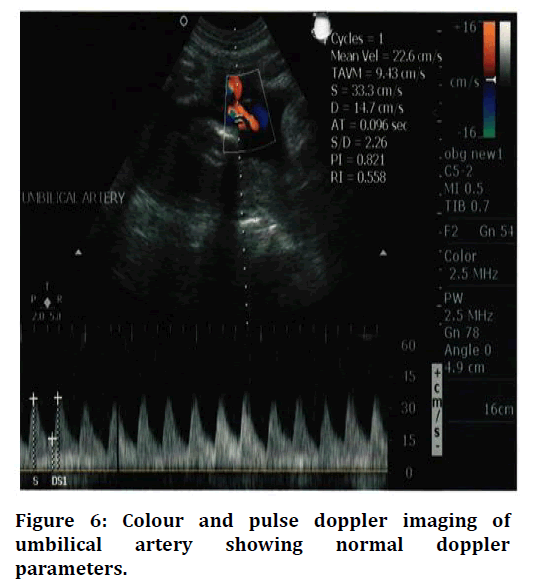
Figure 6. Colour and pulse doppler imaging of umbilical artery showing normal doppler parameters.
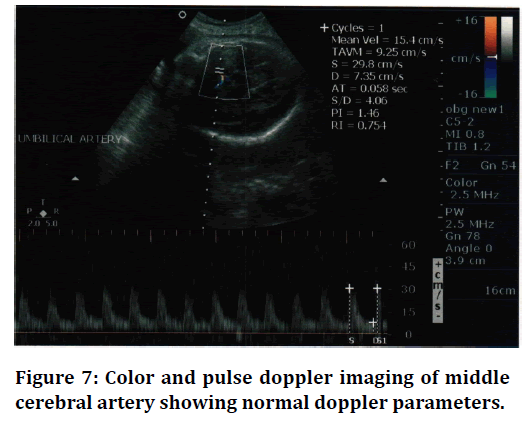
Figure 7. Color and pulse doppler imaging of middle cerebral artery showing normal doppler parameters.
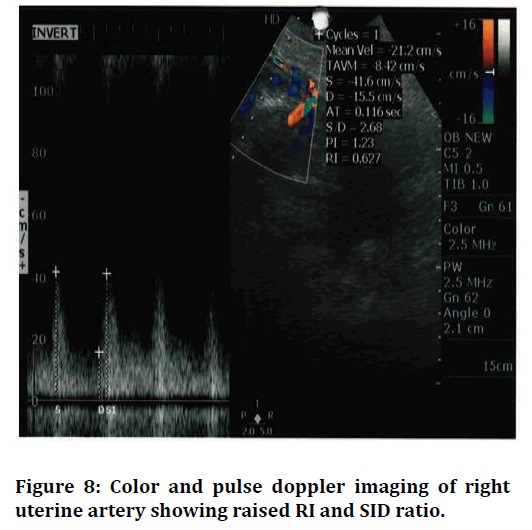
Figure 8. Color and pulse doppler imaging of right uterine artery showing raised RI and SID ratio.
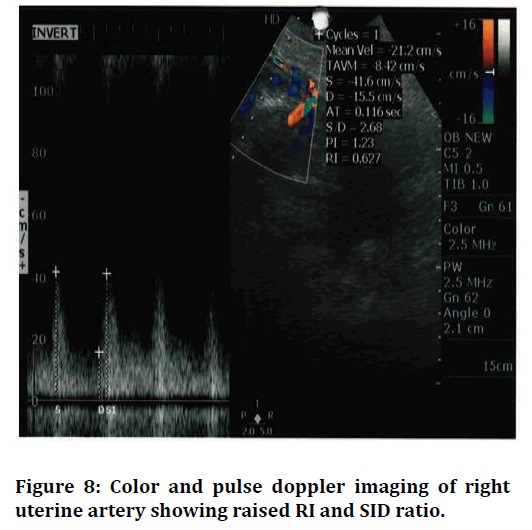
Figure 9. Color and pulse doppler imaging of right uterine artery showing persistent early diastolic notch.
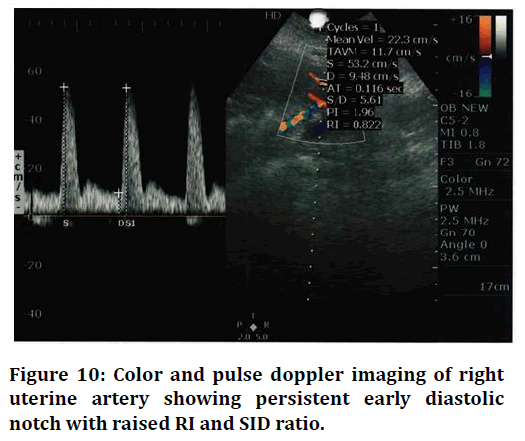
Figure 10. Color and pulse doppler imaging of right uterine artery showing persistent early diastolic notch with raised RI and SID ratio.
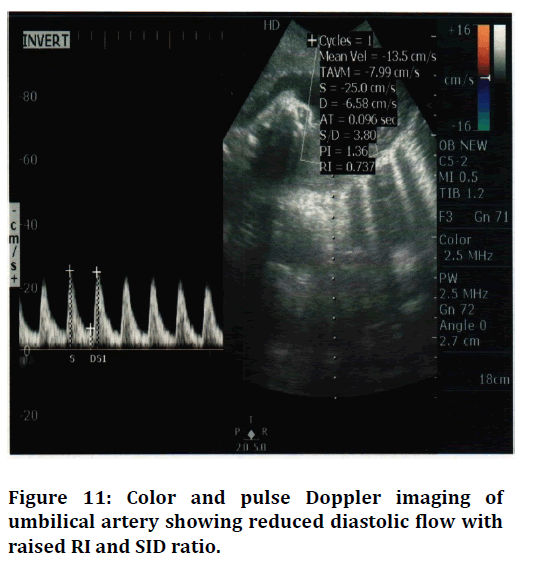
Figure 11. Color and pulse Doppler imaging of umbilical artery showing reduced diastolic flow withraised RI and SID ratio.
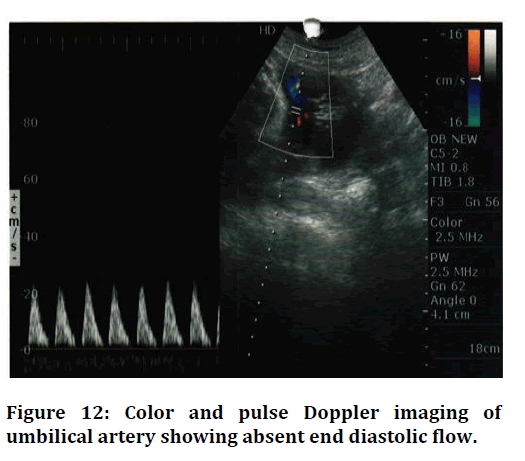
Figure 12. Color and pulse Doppler imaging of umbilical artery showing absent end diastolic flow.
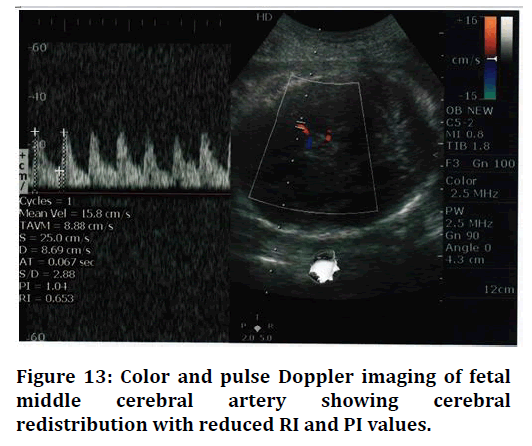
Figure 13. Color and pulse Doppler imaging of fetal middle cerebral artery showing cerebral redistribution with reduced RI and PI values.
Discussion
This is a prospective study done in the department of Obstetrics and Gynaecology, Sree Balaji Medical College and Hospital, Chromepet, Chennai. Study duration is for two years, from August 2010 to September 2012. This study is done in a population of 100 pregnant women with gestational hypertension.
In the present study of 100 hypertensive pregnant women, the m an maternal age is 25.46 yrs, which was comparable to other studies. Duen Holter reported that pregnancy induced hypertension was common in very young teenage women. Guzick and associates in 1987 reported that it was common in older women 30-35 Years of age.
In the present study, 59% were primigravidae and 41% were multigravida. This correlated with the study of Chesley et al. where they found higher incidence of PIH in primigravidae. Whereas in the study conducted by Chin- Ming Liu, the percentage of multigravida is more than primigravidae.
While in Ching Ming Liu's study, 37.67% (249/661) of patients had gestational hypertension, 28% had mild preeclampsia and 55.07% had severe preeclampsia.
In our study group, it was found that anaemia was seen in 18%, Oligohydramnios was observed in 28%. None of the women developed HELLP syndrome, while in Ching-Ming Liu's study, 5.14% (34/661) developed HELLP syndrome [47-55].
Conclusion
Abnormal uterine and umbilical artery doppler flow is associated with severe form of hypertension and higher incidence of IUGR. Abnormal PI of MCA/umbilical artery ratio is also associated with IUGR. RI in MCA is less sensitive than RI in umbilical artery. Maternal complications encountered were abruption placentae, eclampsia and most of the cases needed induction of labour and majority of cases went in for operative delivery. Neonatal complications included birth asphyxia, low birth weight, IUGR, respiratory distress, stained liquor and sepsis which require NICU admissions. Because the changes in the uterine and umbilical circulation strongly correlate with the perinatal outcome, doppler velocimetry is a primary tool for feto-matemal surveillance in hypertensive pregnancy. It is safe, non-invasive technique, easy to perform, easy to interpret, and hence most valuable tool in the management of high risk pregnancy.
Funding
No funding sources.Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflicts of Interest
The authors declare no conflict of interest.
Acknowledegements
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Chesley LC. A short history of eclampsia. Obstet Gynecol 1974; 43:500-602.
- Hypertension in pregnancy. ACOG Technical Bulletin. 1996; 219:1-8.
- Myers JE, Baker PN. Hypertensive diseases and eclampsia. Current Opinion Obstetr Gynecol 2002; 14:119-25.
- Walsh SW. Pre-eclampsia: An imbalance m placental prostacycline and thromboxane production. Am J Obstet Gynecol 1985; 152:335-340.
- Newnham JP, O'Dea MRA, Reid KP 'e t al. Doppler flow velocity waveforms analysis in high risk pregnancies: A randomized controlled trial. Br J Obstet Gynaecol 1991; 98:956-963.
- Baker DW. Pulsed ultrasonic doppler blood flow sensing IEEE Trans sonic ultrasonics SU-17 1970; :170-185.
- Angelsen BAJ, Kristofferson K. On ultrasonic MTI measurement of velocity profiled in blood flow. IEEE Trans Biomed Eng 1979; 26:665-771.
- Namekawa K, Kasai C, Tsukamoto M, et al. Imaging of blood flow using autocor-relation. Ultrasound Med Biol 1982; 8:138.
- Callaghan DA, Rowland TC, Goldman DE. Ultrasonic doppler observation of the fetal heart. Obstet Gynecol 1964; 23:637
- FitzGerald DE, Drumm JE. Noninvasive measurement of the fetal circulation using ultrasound : A new method. BMJ 1977; 2:1450-1451.
- MaCallum WD, Olson RF, Daigle RE, et al. Real time analysis of doppler signals obtained from the fetoplacental circulation. Ultrasound Med 1977; 3:1361-1364.
- Gill RW. Pulsed Doppler with B-mode 1magmg for quantitative blood flow measurements. Ultrasound Med Biol 1979; 5;223-227.
- Eik-Nes SH, Brubakk AO, Ulstein I. Measurement of human fetal blood flow BMJ 1980; 28:283.
- Campbell S, Diaz Recasens J, Griffin DR, et al. New doppler technique for assessing uteroplacental blood flow. Lancet 1983; 1:675.
- Chiba Y, Utsu M, Kanzaki T, et al. Changes in venous flow and intra-tracheal flow in fetal breathing movements. Ultrasound Med Biol 1983; 11:43.
- Maulik D, Nanda NC, Saini VD. Fetal Doppler echocardiography: methods and characterization of normal and abnormal hemodynamics. Am J Cardiol 1984; 53:572.
- Arbeille P, Tranquart F, Body G, et al. Evolution de la circulation arterielle ombilicale et cerebrale du la foetus au cours de la grossesse. Prog Neonatol 1986; 6:30.
- Wladimiroff JW, Tonge HN, Stewart PA. Doppler ultrasound assessment of cerebral blood flow in the human fetus Br J Obstet Gynaecol 1986; 93:471.
- Vyas S, Nicolaides KH,Campbell S. Renal artery flow velocity waveforms in normal and hypoxemic fetuses. Am J Obstet Gynecol 1989; 161:168-172.
- Veille JC, Kanaan C. Duplex Doppler ultrasonographic evaluation of the fetal renal artery in normal and abnormal fetuses. Am J Obstet Gynecol 1989; 161:102-1507.
- Devore GR, Hornstein J, Siassi B, et al. Doppler color flow mapping in use the prenatal diagnosis in the human fetus Echocardiography 1985; 2:551-557.
- Maulik D, Nanda NC, Hsiung MC, et al. Doppler color flow mapping of the fetal heart. Angiology 1986; 37:628-632.
- Taylor KJW, Bums PN, Wells PNT, et al. Ultrasound Doppler flow studies of the ovarian and uterine arteries. Br J Obstet Gynaecol 1985; 92:240-246.
- Atkinson P,Woodcock JP. Doppler ultrasound. Academic Press, London 1982.
- Gill RW. Doppler ultrasound: Physical aspects. Semin Perinatol 1987; 11:292.
- Reid JM, Spencer P. Ultrasonic doppler technique for imaging blood vessels.Science 1972; 176:1235.
- Carroll BA, von Ramm OT. Fundamentals of current doppler technology. Ultrasound 1988; 6:275.
- Maulik D, Yarlagadda P. In vitro Validation of doppler waveform indices. D Maulik, D McNellis (eds). Perinatology Press, Ithaca, Ny, 1987; 257.
- North RA, Ferrier CL, Long D, et al. Utreine artery doppler flow velocity waveforms in the second trimester for the prediction of pre-eclampsia and fetal growth retardation. Obstet Gynecol 1994; 83;378-86.
- Low JA. The current status of maternal and fetal blood flow velocimetry. Am J Obstet Gynecol 1991; 164.
- https://onlinelibrary.wiley.com/doi/abs/10.1016/S1526-9523%2803%2900291-5
- Porcelot L. Applications cliniques de I examen doppler transcutane In: Perommeau P. Velocimetric ultrasonoic doppler. Paris: INSERM, 1974; 213.
- Maulik D, Yarlagadda AP, Youngblood JP, et al. Components of variability of umbilical arterial doppler velocimetry-a prospective analysis. Am J Obstetr Gynecol 1989; 160:1406-12.
- Merritt CRB, Kremakau FW, Hobbins JC. Diagnostic ultrasound: Bio effects andd and safety. Ultrasound Obstet Gynecol 1992; 2:366.
- Miller MW, Ziskin MC. Biological consequences of hyperthermia. Ultrasound Med Biol 1990; 15:707.
- Jauniaux E, Jurkovic D, Campbell S, et al. Investigation of placental circulations by color doppler ultrasonography. Am J Obstetr Gynecol 1991; 164:486-8.
- Thaler I, Manor D, Itskovitz J. C.aanges in uterine blood flow during human pregnancy. Am J Obstet Gynecol 1990; 162:121-125.
- Brosens I, Pijnenborg R, Bland JM, et al. Uteroplacental arterial changes related to interstitial trophoblastic migration in early pregnancy. Placenta 1983; 4:397-414.
- Campbell S, Kevin H, Kurt H. A color atlas of doppler ultrasonography in obstetrics-An induction to its use in maternal fetal medicine. Edited by Kevin H, Campbell S, London, 1995: 60.
- Schulman H, Fleischer A, Stem W. Umbilical velocity wave ratios in human pregnancy. Am J Obstet Gynecol 1984; 148:985-990.
- Rubin PC, Bronghton, Pipkin F. Pre-eclampsia the disease of theories. Br Med Bull 1994; 50:381-96.
- Redman CWG. Current topic: Pre-eclampsia and the placenta. Placenta 1991; 12:310-8.
- Trudinger BJ, Warwich B, Giles MB, et al. Flow velocity waveforms in the maternal uteroplacental and fetal umbilical placental circulation. Am J Obstet Gynecol 1985; 152:155-163.
- Zeeh PM, Arsali NS. Vascular changes in the decidua associated with eclamptogenic toxemia of pregnancy. Am J Clin Patho 1950; 20:1099-1109.
- Peeters LL, Sheldon RE, Jone MK, et al. Blood flow to fetal organs as a function of arterial ox en content. Am J Obstet Gynecol 1979; 135:637-646.
- Arbeille P, Montenegro N, Tranquart F, et al. Assessment of the fetal cerebrovascular areas by color coded doppler. Enchocardiography J 1990; 7:629-634.
- Fleischer A, Schulman H, Formahides G, et al. Uterine artery doppler primary in pregnant women with hypertension. Am J Obstet Gynecol 1986; 154:806-813.
- Trudinger BJ, Cook CM. Doppler umbilical and uterine flow waveforms in severe pregnancy hypertension. Br. J Obstet Gynecol 1990; 97:142-148.
- https://www.elsevier.com/books/chesleys-hypertensive-disorders-in-pregnancy/roberts/978-0-12-374213-1
- Thaler I, Weiner Z, Itskovitz J. Systolic or diastolic notch in the uterine artery blood flow velocity waveforms in hypertensive pregnant patients: Relationship to outcome. Obstet Gynecol 1992; 80:277-282.
- Joern H & Rath W. Comparison of doppler sonographic examination of the umbilical and uterine arteries in high risk pregnancies -Fetal Diagn Ther 1998; 13:150-153.
- Campbell S, Cooper D, Bewley S. Uteroplacental doppler flow velocity waveforms. Br. J Obstet G ecol 1989; 96:1040-1046.
- Farmakides G, Schulman H, Schneider E. Surveillance of the pregnant hypertensive patient with doppler flow velocimetry. Clin Obstetr Gynecol 1992; 35:387-94.
- Karsdrop VH, Van Vingt JM. Clinical significance of absent or reversed end diastolic velocity waveforms in umbilical artery. Lancet 1994; 344:1664-1668.
- Mohd Khalid, Shagufta Wahab, Vijay Kumar, et al. Doppler indices in prediction of fetal outcome in hypertensive pregnant women. Nepal J Obstet Gynaecol 2011; 6:28-34.
Author Info
A Padmaja Rani, K Saraswathi and K Vani*
Department of Obstetrics & Gynecology, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: A Padmaja Rani, K Saraswathi, K Vani, Doppler Study in Gestational Hypertension and Perinatal Outcome-A Prospective Study, J Res Med Dent Sci, 2021, 9(6): 429-438
Received: 08-May-2021 Accepted: 23-Jun-2021
