Research - (2022) Volume 10, Issue 1
Down Syndrome and its Association with Traumatic Dental Injuries: A Systematic Review and Meta-analysis
*Correspondence: Abdullah Ali H, Department of Dental Health, Faculty of Applied Medical Sciences, Al Baha University, Al Baha, Saudi Arabia, Email:
Abstract
Background: Very little is known about the association between traumatic dental injuries (TDI) and Down syndrome (DS) individuals. The aim of this review was to explore the prevalence of TDI among DS individuals and its severity compared to a normal population. Methods: The following databases were searched, without language or date restrictions, between 1900 and November 30, 2021: MEDLINE via PubMed, MEDLINE via OvidSP, Web of Science, CINAHL, Cochrane, and Scopus. A population, exposition, comparison and outcomes (PECO) strategy was performed, which investigated participants with and without DS and their relationship with TDI prevalence. The Joanna Briggs Institute (JBI) checklist was also conducted for quality assessment and bias control. Results: A total of 9,351 eligible articles were identified; 4,014 duplicated studies were eliminated, resulting in 5,337 titles and abstracts. These were then assessed with the inclusion and exclusion criteria, revealing 76 studies eligible for full-text assessment. Consequently, a further 69 were excluded for the reasons that they did not cover TDI or DS, resulting in a total of seven studies included in this review. TDI, class I and II malocclusion associations between both DS and control groups were statistically significant: p=0.005, p=0.05 and p=0.002 respectively. Conclusions: TDI, class I, and class II malocclusion occurrences were more prevalent among DS individuals than healthy controls. Future research may focus on exploring and developing preventive measures that aim at avoiding factors associated with increased TDI among DS individuals, or at least reduce their impact.
Keywords
Down syndrome, Dental trauma, Dental injury, Malocclusion, Dental public health
Introduction
As the age of a mother-to-be increases, the probability of her infant being affected by down syndrome (DS) increases. Overall, it is estimated that there are five cases of DS for every 10,000 births [1]. The facial features of DS individuals will be the same irrespective of their race and ethnicity, with a short neck and hypoplastic mid-face with slanting eyes due to the outer canthus of the eye being higher [2]. The underdeveloped or poorly developed paranasal air sinuses gives rise to a sloped forehead with a flat face. The underdeveloped mid face leads to class III malocclusion with a prognathic mandible, which is typically observed in DS individuals [3]. Moreover, other dental features associated with DS are temporomandibular joint (TMJ) dysfunction due to laxity of the supporting ligaments; an underdeveloped nervous system with lack of motor development; angel’s class III malocclusion and a weak lower limb caused by atlanto axial instability. These are all features that lead to a high risk of traumatic dental injuries (TDI) [4].
It is well known that the structure of the brain and its functions influence the mental and motor abilities of an individual. Any defects to these cause structural and functional issues. Children with DS have diminished psychomotor development, such as small a cerebrum, the brain not maturing completely, and they also have pathophysiological dysfunctions, including defects in neuronal apoptosis regulation and overexpression of the genes controlling the beta amyloid precursor protein (APP). People affected by DS also face problems with learning. These delayed and in harmonic cognitive and motor developmental skills result in hypotonia, reserved primary reflexes and slow performance of wilful reaction, which makes it difficult to maintain balance [5,6]. Moreover, DS children manifest characteristic orofacial features: delayed eruption of teeth, bruxism, malformed teeth, missing teeth, microdontia, open bite, angular cheilitis, crowding, poor oral hygiene, low level caries and a high prevalence of TDI [7-9].
Due to this high prevalence of TDI, it can be considered as a public health problem. Individuals with TDI not only suffer physical, physiological, social and economic consequences but also experience a negative impact on their quality of life, especially for children and adolescents. For DS patients, this adds to the complexity of their situation [10-12]. Exploring the literature revealed that patients with DS have a higher predisposition to experience malocclusion, difficulty in locomotion, macroglossia, and they are often mouth breathers. These characteristics are considered be to predisposed to the occurrence of TDI. Hence, TDIs are quite frequent and leads to severe consequences for vulnerable people with DS [11].
Dental injuries commonly occur in childhood but can occur throughout life. The aetiology of dental injuries varies, with the prominent cause being falls, sports injuries and accidents [3]. There is neither evidence nor consensus in the literature on whether DS individuals are more exposed to TDI than those without DS disorders. Yet, the associated features of DS individuals, with extra chromosomes which result in intellectual disability and delayed mental and physical development, might be the predisposing factors for the TDI [8-11]. It is therefore possible that these features associated with DS may increase the occurrence of the TDI when compared to healthy control individuals [12]. Consequently, the aim of this systematic review was to explore the prevalence of TDI among DS individuals and its severity compared to the normal population.
Materials and Methods
This systematic review and meta-analysis were registered in PROSPERO with CRD registration number: CRD42021244644. The recommendations of PRISMA statement for reporting systematic review and metaanalysis were used in the present review [13].
Eligibility Criteria and Study Selection
A Population, Exposition, Comparison and Outcomes (PECO) strategy was carried out to investigate participants with and without DS and its relationship with TDI prevalence [14]. The PECO format of the current systematic review focused on whether individuals with DS are more prone to TDI when compared to healthy individuals. The population included individuals from all age groups, the exposition considered was DS individuals of all age groups, the comparison (control) was healthy individuals with TDI, and the outcomes included were TDI, and its associated factors, as a primary outcome and malocclusion as a secondary outcome.
Two key inclusion criteria were applied: 1) Studies had to be published between 1900 and November 30, 2021, and 2) Studies had to be based on humans, including observational or cohort research, cross-sectional studies, systematic reviews, analytical studies, randomised and non-randomised clinical trials, case series and case reports. On the other hand, three key exclusion criteria were generated: 1) Studies that do not focus on TDI, 2) Studies in which the data was not compared with the control and 3) Research that was not written in English.
Literature Search Strategy
A systematic search of the literature without language or date restrictions, between 1900 and November 30, 2021, in these databases: MEDLINE via PubMed, MEDLINE via OvidSP, Web of Science, CINAHL, Cochrane, and Scopus; was conducted. Considering the fact that studies on the prevalence of TDI in DS are rare, an advanced search associated with the risk factors of DS leading to TDI was considered, such as motor skills, motor development and lack of function in the nervous system.
The MeSH terms used in the present systematic review were dental trauma, tooth injuries, dental injury, teeth injury, tooth movement, tooth avulsion, teeth avulsion, dental dislocation, teeth extrusion, lateral luxation, tooth fractures, teeth fractures, crown fractures, root fractures, oral health, accidental fall, malocclusion, TMJ dysfunction, TMJ disorder, lack of nervous system, motor skill, motor development, down syndrome, down’s syndrome, and trisomy 21.
The ‘OR’ and ‘AND’ Boolean operators were used to combine keywords. The MeSH synonyms and both associated and free terms were also included. Table 1 illustrates the literature search strategy across different databases.
| Database | Search Strategy |
|---|---|
| PubMed via Medline (n=1482) | #1 dental: "dental health services"[MeSH Terms] OR ("dental"[All Fields] AND "health"[All Fields] AND "services"[All Fields]) OR "dental health services"[All Fields] OR "dental"[All Fields] OR "dentally"[All Fields] OR "dentals"[All Fields] teeth: "teeth's"[All Fields] OR "teeth"[All Fields] OR "tooth"[MeSH Terms] OR "tooth"[All Fields] OR "teeth"[All Fields] OR "tooth's"[All Fields] OR "tooths"[All Fields] |
| #2 Tooth movement: "tooth movement techniques"[MeSH Terms] OR ("tooth"[All Fields] AND "movement"[All Fields] AND "techniques"[All Fields]) OR "tooth movement techniques"[All Fields] OR ("tooth"[All Fields] AND "movement"[All Fields]) OR "tooth movement"[All Fields] tooth avulsion: "tooth avulsion"[MeSH Terms] OR ("tooth"[All Fields] AND "avulsion"[All Fields]) OR "tooth avulsion"[All Fields] teeth: "teeth's"[All Fields] OR "teeth"[All Fields] OR "tooth"[MeSH Terms] OR "tooth"[All Fields] OR "teeth"[All Fields] OR "tooth's"[All Fields] OR "tooths"[All Fields] avulsion, "avulse"[All Fields] OR "avulsed"[All Fields] OR "avulsing"[All Fields] OR "avulsive"[All Fields] OR "fractures, avulsion"[MeSH Terms] OR ("fractures"[All Fields] AND "avulsion"[All Fields]) OR "avulsion fractures"[All Fields] OR "avulsion"[All Fields] OR "avulsions"[All Fields] | |
| #3 Dental: "dental health services"[MeSH Terms] OR ("dental"[All Fields] AND "health"[All Fields] AND "services"[All Fields]) OR "dental health services"[All Fields] OR "dental"[All Fields] OR "dentally"[All Fields] OR "dentals"[All Fields] dislocation: "dislocate"[All Fields] OR "dislocates"[All Fields] OR "dislocating"[All Fields] OR "dislocator"[All Fields] OR "dislocators"[All Fields] OR "joint dislocations"[MeSH Terms] OR ("joint"[All Fields] AND "dislocations"[All Fields]) OR "joint dislocations"[All Fields] OR "dislocated"[All Fields] OR "dislocation"[All Fields] OR "dislocations"[All Fields]teeth: "teeth's"[All Fields] OR "teeth"[All Fields] OR "tooth"[MeSH Terms] OR "tooth"[All Fields] OR "teeth"[All Fields] OR "tooth's"[All Fields] OR "tooths"[All Fields] extrusion: "extrusion"[All Fields] OR "extrusions"[All Fields] lateral: "functional laterality"[MeSH Terms] OR ("functional"[All Fields] AND "laterality"[All Fields]) OR "functional laterality"[All Fields] OR "laterality"[All Fields] OR "lateral"[All Fields] OR "lateralization"[All Fields] OR "lateralization"[All Fields] OR "lateralize"[All Fields] OR "lateralized"[All Fields] OR "literalizes"[All Fields] OR "lateralizing"[All Fields] OR "literalities"[All Fields] OR "lateralization"[All Fields] OR "lateralization"[All Fields] OR "lateralize"[All Fields] OR "lateralized"[All Fields] OR "lateralizes"[All Fields] OR "lateralizing"[All Fields] OR "laterally"[All Fields] OR "laterals"[All Fields] luxation, Tooth: "tooth avulsion"[MeSH Terms] OR ("tooth"[All Fields] AND "avulsion"[All Fields]) OR "tooth avulsion"[All Fields] OR ("luxation"[All Fields] AND "tooth"[All Fields]) OR "luxation, tooth"[All Fields] teeth: "teeth's"[All Fields] OR "teeth"[All Fields] OR "tooth"[MeSH Terms] OR "tooth"[All Fields] OR "teeth"[All Fields] OR "tooth's"[All Fields] OR "tooths"[All Fields] crown: "crown's"[All Fields] OR "crowned"[All Fields] OR "crowns"[MeSH Terms] OR "crowns"[All Fields] OR "crown"[All Fields] root: "plant roots"[MeSH Terms] OR ("plant"[All Fields] AND "roots"[All Fields]) OR "plant roots"[All Fields] OR "root"[All Fields] | |
| #4 Oral health, "oral health"[MeSH Terms] OR ("oral"[All Fields] AND "health"[All Fields]) OR "oral health"[All Fields] Accidental fall, "accidental falls"[MeSH Terms] OR ("accidental"[All Fields] AND "falls"[All Fields]) OR "accidental falls"[All Fields] OR ("accidental"[All Fields] AND "fall"[All Fields]) OR "accidental fall"[All Fields] | |
| #5Malocclusion, "malocclusal"[All Fields] OR "malocclusion"[MeSH Terms] OR "malocclusion"[All Fields] OR "malocclusions"[All Fields] OR "malocclusive"[All Fields] | |
| #6 TMJ dysfunction: "temporomandibular joint dysfunction syndrome"[MeSH Terms] OR ("temporomandibular"[All Fields] AND "joint"[All Fields] AND "dysfunction"[All Fields] AND "syndrome"[All Fields]) OR "temporomandibular joint dysfunction syndrome"[All Fields] OR ("tmj"[All Fields] AND "dysfunction"[All Fields]) OR "tmj dysfunction"[All Fields] TMJ disorder,: "temporomandibular joint disorders"[MeSH Terms] OR ("temporomandibular"[All Fields] AND "joint"[All Fields] AND "disorders"[All Fields]) OR "temporomandibular joint disorders"[All Fields] OR ("tmj"[All Fields] AND "disorder"[All Fields]) OR "tmj disorder"[All Fields] nervous system,: "nervous system"[MeSH Terms] OR ("nervous"[All Fields] AND "system"[All Fields]) OR "nervous system"[All Fields] Motor skill,: "motor skills"[MeSH Terms] OR ("motor"[All Fields] AND "skills"[All Fields]) OR "motor skills"[All Fields] OR ("motor"[All Fields] AND "skill"[All Fields]) OR "motor skill"[All Fields] Motor: "motor"[All Fields] OR "motor's"[All Fields] OR "motoric"[All Fields] OR "motorically"[All Fields] OR "motoric"[All Fields] OR "motoring"[All Fields] OR "motorization"[All Fields] OR "motorized"[All Fields] OR "motorization"[All Fields] OR "motorized"[All Fields] OR "motors"[All Fields] development: "develop"[All Fields] OR "developed"[All Fields] OR "developed"[All Fields] OR "developer"[All Fields] OR "developer's"[All Fields] OR "developers"[All Fields] OR "developing"[All Fields] OR "developments"[All Fields] OR "develops"[All Fields] OR "growth and development"[Subheading] OR ("growth"[All Fields] AND "development"[All Fields]) OR "growth and development"[All Fields] OR "development"[All Fields] down syndrome: "down syndrome"[MeSH Terms] OR ("down"[All Fields] AND "syndrome"[All Fields]) OR "down syndrome"[All Fields down's syndrome: "down syndrome"[MeSH Terms] OR ("down"[All Fields] AND "syndrome"[All Fields]) OR "down syndrome"[All Fields] OR "down s syndrome"[All Fields] | |
| #7 trisomy 21.: "down syndrome"[MeSH Terms] OR ("down"[All Fields] AND "syndrome"[All Fields]) OR "down syndrome"[All Fields] OR "trisomy 21"[All Fields] | |
| #8 Dental: "dental health services"[MeSH Terms] OR ("dental"[All Fields] AND "health"[All Fields] AND "services"[All Fields]) OR "dental health services"[All Fields] OR "dental"[All Fields] OR "dentally"[All Fields] OR "dentals"[All Fields] trauma,: "injuries"[Subheading] OR "injuries"[All Fields] OR "trauma"[All Fields] OR "wounds and injuries"[MeSH Terms] OR ("wounds"[All Fields] AND "injuries"[All Fields]) OR "wounds and injuries"[All Fields] OR "trauma's"[All Fields] OR "traumas"[All Fields] tooth injuries: "tooth injuries"[MeSH Terms] OR ("tooth"[All Fields] AND "injuries"[All Fields]) OR "tooth injuries"[All Fields] | |
| # 7 & #8 | |
| OvidSP via Medline (n=1363) | #9 (tw:(Disabled Persons)) OR (tw:(Dental Injury)) OR (tw:(Dental Trauma)) OR (tw:(special needs)) OR (tw:(special needs)) OR (tw:(Down syndrome)) OR (tw:(Trisomy 21)) OR (tw:(Mongolism)) OR (OR (tw:(Dental Injury Spectrum Disorder)) |
| #10 (tw:(Tooth Injuries)) OR (tw:(Tooth Movement)) OR (tw:(Tooth avulsion)) OR (tw:(Teeth injury*)) OR (tw:(root fracture*)) OR (tw:(dental injury*)) OR (tw:(dental trauma)) OR (tw:(traumatic injur*)) OR (tw:( Oral Health)) OR (tw:( Malocclusion)) | |
| #9 & #10 | |
| Web of Science (n=2046) | #11 “disabled persons” OR disabl* OR “Dental Trauma” OR special needs OR “special needs” OR vision disord* OR visually impair* |
| #12 “down syndrome” OR “trisomy 21” OR “special care” OR “autistic disorder” OR Dental Injury OR “Dental Injury spectrum disorder” OR “Dental Trauma” | |
| #13 “dental injury” OR “dental injuries” OR “dental trauma” OR “traumatic injury” OR “traumatic injuries” OR “teeth avulsion” OR exarticulation OR “dental dislocation” OR “teeth extrusion” OR “lateral luxation” OR “crown fracture” OR “crown fractures” OR “root fracture” OR “root fractures” | |
| #14 OR “tooth fractures” OR “teeth injury” OR “teeth injuries” OR “dental injury” OR “dental injuries” OR “dental trauma” OR “traumatic injury” OR “traumatic injuries” OR “teeth avulsion” | |
| #11, #12, #13 #14 | |
| Scopus (n=1926) | #15 KEY ( dental AND trauma, AND tooth AND injuries OR dental AND injur* OR teeth AND injur*, AND tooth AND movement OR tooth AND avulsion OR teeth AND avulsion, AND dental AND dislocation OR teeth AND extrusion OR lateral AND luxation, AND tooth AND fractur* OR teeth AND fractur* OR crown AND fractur* OR root AND fractur*, AND oral AND health, AND accidental AND fall, AND malocclusion, AND tmj AND dysfunction OR tmj AND disorder, AND lack AND of AND nervous AND system, AND motor AND skill, AND motor AND development; AND down AND syndrome OR down’s AND syndrome OR trisomy AND 21. ) |
| CHINAHL (n=2055) | #16 Disabled Persons OR Dental Trauma OR Down syndrome OR Trisomy 21 OR Mongolism OR Dental Injury OR Dental Injury Spectrum Disorder OR Oral health |
| #17 Dental Injury* OR “Tooth fractur* OR *oral heath* OR Teeth injury* OR dental injury* OR “dental trauma” OR traumatic injuyr* OR OR “Malocclusion” OR crown fractur* OR root fracture | |
| #15, #16 & #17 | |
| Cochrane (n=479) | #18 Dental trauma, tooth injuries OR dental injur* OR teeth injur*, Tooth movement OR tooth avulsion OR teeth avulsion, Dental dislocation OR teeth extrusion OR lateral luxation, Tooth fractur* OR teeth fractur* OR crown fractur* OR root fractur*, Oral health, Accidental fall, Malocclusion, TMJ dysfunction OR TMJ disorder, Lack of nervous system, Motor skill, Motor development; AND down syndrome OR down’s syndrome OR trisomy 21. in Title Abstract Keyword |
| AND | |
| #19 Down syndrome in Title Abstract Keyword - in Cochrane Reviews, Cochrane Protocols, Trials, Clinical Answers, Editorials, Special Collections (Word variations have been searched | |
| #18 & #19 |
Table 1: Search Strategy Across Different Databases.
The two reviewers searched all sources independently to reduce selection bias. They screened the titles and abstracts of articles obtained through the search to assess their eligibility.
At this stage, a total of 9,351 eligible articles were identified; 4,014 duplicated studies were eliminated, resulting in 5,337 titles and abstracts. Following this, the reviewers conferred and decided which articles were to be included. It ought to be emphasised that there was no disagreement between the two researchers about articles to be included.
However, it was proposed that if any disagreements were presented between the reviewers about the eligibility of the included studies, it would be resolved by a third specialised reviewer.
After evaluating the titles and abstracts, a further 5,261 studies were excluded because they did not meet the inclusion criteria of this review: revealing 76 studies for full-text assessment. Consequently, a further 69 were excluded because they did not cover TDI or DS, resulting in a total of seven studies included, four of which were included in the quantitative synthesis and meta-analysis. Figure 1 describes the process utilised for searching the literature and identifying the relevant studies using the PRISMA flow diagram [12].
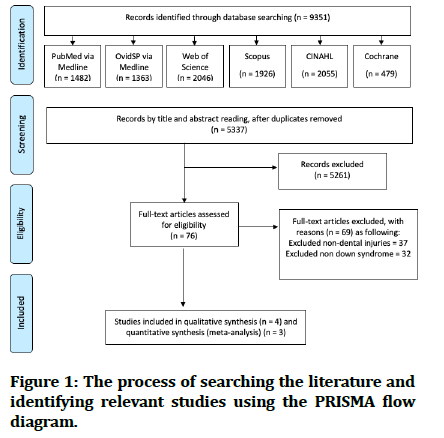
Figure 1: The process of searching the literature and identifying relevant studies using the PRISMA flow diagram.
Quality Assessment and Meta-Analysis
Quality assessment and bias control were conducted according to the guidelines illustrated by the Joanna Briggs Institute (JBI) of the University of Adelaide [13].
This quality assessment was done for the inclusion criteria: the subjects included, study setting, method of exposure and outcome measurement, any confounding factors, statistical analysis and overall appraisal (Table 2).
| JBI Checklist | Al Sarheed MA (2015) | Al‐Batayneh et al. (2017) | Gaith et al. (2019) |
|---|---|---|---|
| Were the criteria for inclusion in the sample clearly defined? | Yes | Yes | Yes |
| Were the study subjects and the setting described in detail? | Yes | Yes | Yes |
| Was the exposure measured in a valid and reliable way? | Yes | Yes | Yes |
| Were objective, standard criteria used for measurement of the condition? | Yes | Yes | Yes |
| Were confounding factors identified? | Not applicable | Not applicable | Not applicable |
| Were strategies to deal with confounding factors stated? | Not applicable | Not applicable | Not applicable |
| Were the outcomes measured in a valid and reliable way? | Yes | Yes | Yes |
| Was appropriate statistical analysis used? | Yes | Yes | Yes |
| overall appraisal | Included | Included | Included |
Table 2: Quality Assessment According to the JBI Checklist.
The Meta-analysis and forest plot were generated through RevMan software (version 5.4). The results used a fixed-effects meta-analysis, with the number of events reported and assessed in two groups. The risk of bias of each study was assessed, in the first instance, based on the information reported in the studies included in this review. The 95% confidence intervals and two-sided pvalues for each outcome were also calculated. Heterogeneity was assessed using both the Chi-square (χ²) test and the I² index. The forest plot revealed no evidence of heterogeneity as depicted by the value of I2 as 0%, which is not significant. Subsequently, we used a fixed-effect model in the present systematic review.
Results
A total of 5,337 articles were identified using the search strategy. After detailed evaluation of full text articles, only seven articles were included (Figure 1). The characteristics of the included studies are provided in Table 3.
| Author and Year | Age Range Average | Sample | Place of Data Collection | |||||
|---|---|---|---|---|---|---|---|---|
| DS Group | Control Group | |||||||
| Events | Total | Events | Total | DS Group | Control Group | |||
| TDI | ||||||||
| Al Sarheed M (2015) | DS (10.61 ± 2.47) | 23 | 93 | 5 | 99 | The Saut Society Riyadh | Schools | |
| Control (10.89 ± 2.29) | ||||||||
| Al‐Batayneh et al. (2017) | DS (11.10 ± 3.8) | 60 | 166 | 31 | 1010 | Schools | Schools | |
| Control (11.70 ± 4.22) | ||||||||
| Gaith et al. (2019) | DS (9.3 ± 2.8) | 74 | 82 | 4 | 82 | Special Needs Centers | Dental Centers | |
| Control (11.7 ± 4.4) | ||||||||
| Malocclusion | ||||||||
| Al Sarheed M (2015) | Class I | DS (10.61 ± 2.47) | 23 | 93 | 78 | 99 | The Saut Society Riyadh | Schools |
| Class II | Control (10.89 ± 2.29) | 20 | 13 | |||||
| Class III | 50 | 8 | ||||||
| Marques LS et al (2015) | Class I | DS (14.73) | 13 | 60 | 31 | 60 | Not reported | Dentistry Collage |
| Class II | 16 | 25 | ||||||
| Class III | Control (12.18) | 31 | 4 | |||||
| Gaith et al. (2019) | Class I | DS (9.3 ± 2.8) | 4 | 81 | 68 | 110 | Special Needs Centers | Dental Centers |
| Class II | Control (11.7 ± 4.4) | 7 | 28 | |||||
| Class III | 70 | 14 | ||||||
Table 3: Data Extraction.
Traumatic Dental Injuries (TDI)
Our findings revealed that three studies explored TDI among DS individuals and healthy control. The first study showed that DS children had a significantly higher proportion of incisal fractures, compared to the healthy control group (24.73%, and 4.95% respectively) [3]. While the second study indicated that 88.7% of the DS group had TDI, compared to 3.2% in the control group without DS [15]. Finally, the third study concluded that the prevalence of TDI among DS and control group were n=83, 8.7%, and n= 42, 4.1% respectively [16,17].
The present systematic review revealed that there was evidence of heterogeneity in the TDI association among the three trials eligible for meta-analysis (I2 = 81%, p= 0.005). The previous three studies which focused on TDI association among DS and control groups had point estimates with an odds ratio ranging from 6.18 to 69.95. The forest plot of the TDI association between the DS group and control group is described in Figure 2. It is clearly shown in Figure 2 that the diamond shape does not touch the line of no effect, and this means that the difference in TDI association between both the DS and control groups was statistically significant. Figure 3 illustrates the TDI funnel plot of publication bias.
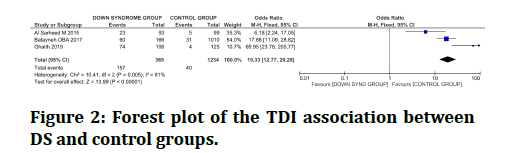
Figure 2: Forest plot of the TDI association between DS and control groups.
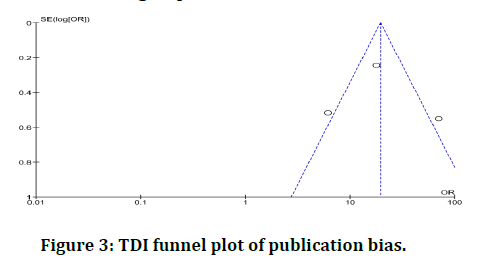
Figure 3:TDI funnel plot of publication bias.
Malocclusion
The results of this systematic review showed that three studies explored the malocclusion among DS individuals and healthy control. The first study reported that the children with DS had more occurrences of class III incisor relationship than the control group (45% and 8% respectively). Likewise, the DS group also showed more incidents of class III molar relationship compared to the control (50% and 8%, respectively0 [3]. The second study indicated a significantly higher prevalence of malocclusion among the individuals with DS than the control group (P= 0.028) [12]. Finally, the third study concluded significantly higher-class III molar angle malocclusion in DS in comparison to controls (66% and 11.2%) [16].
The meta-analysis revealed a heterogeneity in class I and class II malocclusion associations among both the DS and control groups: I2 = 67%, p= 0.05 and I2 = 84%, p= 0.002. Figure 4 shows a forest plot of the malocclusion association between DS and control groups. While Figure 5 describes the malocclusion funnel plot of publication bias. However, there is no evidence of heterogeneity in class III malocclusion between DS and the healthy control groups (I2 = 0%, p= 0.41) (Figures 4 and 5).
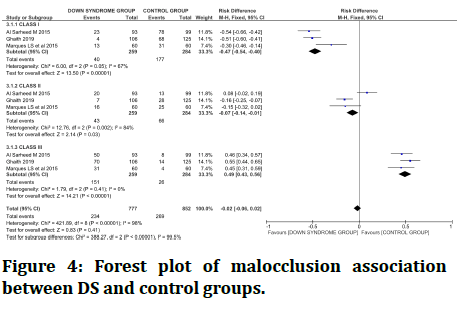
Figure 4:Forest plot of malocclusion association between DS and control groups.
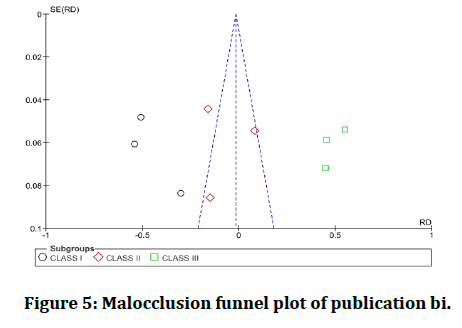
Figure 5:Malocclusion funnel plot of publication bi.
Discussion
People with DS disabilities have physical and intellectual deficiencies. These commonly interfere with the performance of normal functions of these individuals, and therefore require greater care and supervision for their activities throughout their lives. This is also applicable to the activities that relate to their oral health. The lack of cooperation, understanding, comprehension of individuals with DS or unapproachable specialised health centres contribute towards worsening their situation [6,7]. In the dental literature, there have been several reviews concerning oral health and TDI among individuals with intellectual disabilities, and those in special care. However, there were no systematic reviews which focused particularly on examining the association between TDI and DS individuals [4]. It was for this reason that this review was carried out to report the best available evidence to determine the prevalence and relation between TDI and DS individuals, compared to healthy individuals.
In the present meta-analysis, patients with DS had a statistically significant higher chance of having TDI in comparison to healthy patients. These findings are in accordance with those reported by Silveira et al (2020), where they reported that in general people with special needs, such as cerebral palsy (CP), DS and hyperactivity disorders, had a higher chance of suffering from TDI; however, this study had a very low certainty of evidence [17]. Likewise, other research found that people with intellectual disabilities, including DS and hyperactivity disorders, had a higher chance of TDI [11, 12]. This can not only be attributed to cognitive and functional impairments seen in DS patients, but DS may also affect motor coordination issues and peer relationships, increasing the risk of physical abuse [16]. A further possible reason for the increase in occurrences of TDI among DS patients might be that those patients commonly have more difficulties protecting themselves from falls, as well as problems in reacting to stimuli or noise.
Our results also showed a significant difference in class I and class II malocclusion association between DS compared to healthy control subjects. This is quite consistent with another study conducted by Dieguez-Perez M et al (2016), where they concluded that children with intellectual disabilities, including both CP and DS patients, were more likely to be affected by malocclusion [4]. The differences between children with intellectual disabilities and those without were significant and malocclusion was more prevalent in the former group, with cases of classes II and open bite more common in children with CP and occurrences of classes III higher among children with DS [4]. Similarly, Marques LS et al (2015) also reported statistically significant differences between DS and healthy individuals for missing teeth, diastema, overjet, mandibular protrusion, anterior open bite, posterior crossbite, facial type, lip incompetence and angle classification [12]. The underdevelopment of the midface and mandibular prognathism, a history of premature birth, and long face pattern were found to correlate with the severity of malocclusion [4,12]. These factors may contribute greatly towards the prevalence of malocclusion among DS, compared to healthy individuals.
Gaith et al. (2019) reported significantly higher prevalence of class III molar relationship, open bite and other occlusal problems among children with down syndrome [14]. It is well known that DS children have anomalies, be it occlusal or dentofacial. They have inherited mental retardation with a varying range of cognitive dysfunction and characteristic facial features, cardiovascular defects, skeletal abnormalities, ocular defects, protuberant abdomen, hypogonadism and delayed puberty [15-17]. Craniofacial abnormalities include brachycephaly, flat occiput, cranial base flattening, small sella turcica and a prominent forehead, a broad and short neck, hypoplasia of the maxilla, up slanting palpebral fissures, short ears and small chin. The nasal bone is shorter, angled acutely and the frontal process of the maxilla is underdeveloped. The growth of both jaws is reduced, and the mandibular ramus and body are shorter than on non-DS individuals. The vertical dimensions of the maxillary and mandibular alveolar height are reduced. Therefore, all these characteristics associated with DS may essentially lead to an overall improper functioning, which manifests in the form of delayed eruption, TDI, malocclusion, thickening of lips, macroglossia and a fissured and protruding tongue [18-22].
Once a tooth becomes traumatised, local sequelae might occur immediately, or over the months or years thereafter, leading to the requirement of years of followup after the initial TDI treatment, which results in further direct and indirect costs. Moreover, inadequate oral-care habits along with potential negligence on the parents’ behalf, lack of awareness of prevention and regular dental visits, as well as long waiting hours for dental treatment can all worsen DS individuals’ situations. Therefore, prevention, through the development of measures aimed at avoiding these aforementioned factors, or at least reducing their impact, must constitute the primary goal. Similar principles of treatment apply to DS patients as those of the general population but with extra effort focused on behavioural challenges and intelligence quotient medications. In cases where the patient is not cooperative, treatment in the dental office or medical facility can be carried out under sedation or general anaesthesia [22].
A key limitation to the present systematic review was that the studies included were low in number. They were also analytical cross-sectional studies, which may overestimate the findings. However, this review was a first of its kind in the dental literature, which offered insights into the prevalence and relation between TDI and DS individuals, compared to healthy matched controls. It provides a comprehensive coverage of the research that has been carried out on TDI and DS individuals with suggestions on the potential direction of future research, which we will touch upon in the conclusion.
Conclusion
DS individuals reported greater incidence of TDI and malocclusion (class I and II), as compared to healthy control groups. No significant association of class III malocclusion was detected among both DS and control groups. The DS group may require early and regular dental care in order to prevent and limit the severity of their anomalies. Future research may evaluate the first management of TDI and possible long-term sequelae of TDI among DS individuals. A further direction in research can also focus on exploring preventive measures that aim at avoiding factors which cause higher rates of TDI among DS individuals, or at least reducing their impact.
Funding
This systematic review and meta-analysis did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgement
The author would like to acknowledge Dr Abdullah Madhawi, Assistant Professor and Consultant of Oral and Maxillofacial, Dental Healh Department, Faculty of Applied Medical Sciences, Al Baha University, for his help and support in the data extraction process and bias control of this systematic review.
References
- Desai SS. Down syndrome: A review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 84:279-85.
- Noordin S, Wright JG, Howard AW. Global relevance of literature on trauma. Clin Orthop Related Res 2008; 466:2422-7.
- AlSarheed M. A comparative study of oral health amongst trisomy 21 children living in Riyadh, Saudi Arabia: Part 1 caries, malocclusion, trauma. Saudi Dent J 2015; 27:220-3.
- Diéguez-Pérez M, de Nova-García MJ, Mourelle-Martínez MR, et al. Oral health in children with physical (Cerebral Palsy) and intellectual (Down Syndrome) disabilities: Systematic review I. J Clin Exp Dent 2016; 8:e337-43.
- Malak R, Kostiukow A, Krawczyk-Wasielewska A, et al. Delays in motor development in children with down syndrome. Med Sci Monit 2015; 21:1904-10.
- Van Allen MI, Fung J, Jurenka SB. Health care concerns and guidelines for adults with down syndrome. Am J Med Genet 1999; 89:100-10.
- American Academy of Pediatric Dentistry. Guidelines on management of dental patients with special health care needs. Pediatr Dent 2016; 38:171–176.
- Macho V, Palha M, Macedo AP, et al. Comparative study between dental caries prevalence of down syndrome children and their siblings. Special Care Dent 2013; 33:2-7.
- Andreasen P, Davis E. Oral health of patients with intellectual disabilities: A systematic review. Spec Care Dentist 2010; 30:110–117.
- Marques LS, Alcântara CE, Pereira LJ, et al. Down syndrome: A risk factor for malocclusion severity? Brazilian Oral Res 2015; 29:1-7.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J Clin Epidemiol 2009; 62:e1-34.
- Maia LC, Antonio AG. Systematic reviews in dental research. A guideline. J Clin Pediatr Dent 2012; 37:117-24.
- https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal Checklist_for_Analytical_Cross_Sectional_Studies2017_0.pdf.
- Ghaith B, Al Halabi M, Khamis AH, et al. Oral health status among children with Down syndrome in Dubai, United Arab Emirates. J Int Soc Prevent Communit Dent 2019; 9:232-9.
- Oliveira AC, Paiva SM, Campos MR, et al. Factors associated with malocclusions in children and adolescents with Down syndrome. Am J Orthod Dentofac Orthop 2008; 133:489-e1.
- Al‐Batayneh OB, Owais AI, Al‐Saydali MO, et al. Traumatic dental injuries in children with special health care needs. Dent Traumatol 2017; 33:269-75.
- Oredugba F. Oral health condition and treatment needs of a group of Nigerian individuals with Down syndrome. Down Syndrome Res Practice 2007; 12:72-6.
- Silveira AL, Magno MB, Soares TR. The relationship between special needs and dental trauma. A systematic review and meta‐analysis. Dent Trauma 2020; 36: 218-36.
- Sarkar PA, Shigli A. Management of traumatic intrusive luxation of incisors in a patient with Down’s syndrome. Case Reports 2011; 2011:bcr1020114887.
- Hennequin M, Faulks D, Vyrune JL, et al. Significance of oral health in persons with Down syndrome: a literature review. Dev Med Child Neurol 1999; 41:275–83.
- NS S, Jayakaran GT. Exploratory Study on the developmental pattern of oral-motor function in children with down's syndrome. J India Institute Speech Hearing 2015; 34.
- Shyama M, Al‐Mutawa SA, Honkala S. Malocclusions and traumatic injuries in disabled schoolchildren and adolescents in Kuwait. Special Care Dent 2001; 21:104-8.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Schoar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Sholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Department of Dental Health, Faculty of Applied Medical Sciences, Al Baha University, Al Baha, Saudi ArabiaCitation: Alzahrani, AAH, Down Syndrome and its Association with Traumatic Dental Injuries: A Systematic Review and Metaanalysis, J Res Med Dent Sci, 2022, 10(1): 561-569
Received: 21-Dec-2021, Manuscript No. Jrmds-21-50374; , Pre QC No. Jrmds-21-50374 (PQ); Editor assigned: 23-Dec-2021, Pre QC No. Jrmds-21-50374 (PQ); Reviewed: 06-Jan-2022, QC No. Jrmds-21-50374; Revised: 10-Jan-2022, Manuscript No. Jrmds-21-50374 (R); Published: 17-Jan-2022
