Research - (2020) Advances in Dental Surgery
Effect of Cementation Protocol on the Marginal Adaptation of Indirect Overlay Restorations Fabricated from Two Different All-Ceramic CAD/CAM Materials
Zaidoon Hasan Mohammed* and Manhal A Majeed
*Correspondence: Zaidoon Hasan Mohammed, Department oDepartment of Conservative Dentistry, College of Dentistry, University of Baghdad, Iraq, Email:
Abstract
The objective of this in vitro study was to measure and compare the marginal adaptation of indirect overlay restorations fabricated from two different all-ceramic CAD/CAM materials (lithium disilicate and reinforced composite blocks) cemented with three different cementation protocols (adhesive resin cement, preheated composite, and sonically-activated composite). Fortyeight human maxillary first-premolar teeth were prepared for indirect overlay restorations with butt joint preparation design. The prepared teeth were divided into two main groups of twenty-four teeth each according to the type of CAD/CAM material used for the fabrication of the restorations: Group A: overlays fabricated from lithium disilicate blocks (IPS e.max CAD, Ivoclar Vivadent, Liechtenstein), Group B: overlays fabricated from reinforced resin blocks (BRILLIANT Crios, Coltene/ Whaledent AG, Switzerland). Each group was then further subdivided into three subgroups of eight teeth each according to the cementation protocol used: Subgroups (A1, B1): cemented with adhesive resin cement (RelyX Ultimate, 3M ESPE, USA), Subgroups (A2, B2): cemented with preheated composite (Filtek Z350 XT, 3M ESPE, USA) and Subgroups (A3, B3): cemented with sonically-activated composite (SonicFill 2, Kerr Corp., USA). The prepared teeth were then scanned using CEREC Omnicam digital intra-oral scanner, then overlay restorations were designed using Sirona InLab 15.1 software and milled with InLab MC XL milling unit. Overlay restorations of group A were then subjected to crystallization /glaze firing at 840 C0 while those of group B were finished and polished only. Each restoration was then seated on its respective tooth using a custom-made specimen holding device. The marginal gap was then measured using a digital microscope at four points on each surface of the tooth at a magnification of 230x and the mean value of these measurements was recorded. Each restoration cemented on its respective tooth according to the aforementioned sample grouping following the manufacturers’ instructions of each material. The results of this study were then analyzed statistically using independent t-test, one-way ANOVA test, LSD test, and Dunnett T3 test. The results of this study showed that the overlay restorations fabricated from reinforced resin blocks (Briallant Crios) recorded less marginal gap than those restorations fabricated from lithium disilicate blocks (IPS e.max CAD) with statistically significant difference (p<0.05), pre- and post-cementation regardless of cementation protocol used. The results of this study also showed that, for both block types, cementation with adhesive resin cement provided significantly better marginal adaptation than cementation with preheated composite and sonically-activated composite, with the statistically non-significant difference between the latter two cementation protocols.
Keywords
Lithium disilicate, Resin block, Resin cement, Marginal gap, Preheated composite, Sonicfill
Introduction
Full-coverage restorations require removal of a substantial amount of tooth structure, which in turn may cause weakening of the remaining substrate. Overlay restorations are considered an alternative option for traditional full-coverage restorations for restoring missing or weakened tooth structure [1,2].
The marginal as well as the internal adaptation of the ceramic restorations is considered a significant factor for the longevity and clinical success of ceramic restorations. The luting cement can be dissolved with the presence of these marginal gaps which act as an area for biofilm development and cause caries as well as periodontal diseases. Despite advancements in the CAD/CAM technologies, the marginal adaptation continues to be the target of investigations since it is considered a critical factor for the clinical success and longevity of restorations [3,4].
The lithium disilicate is considered a gold standard material for the fabrication of allceramic restorations. It is used according to its mechanical properties which make it close to the properties of enamel to be replaced. However, due to its hardness, micro-crack can be developed during milling within the materials which susceptible the restoration to failure under load, also it can cause wearing of the opposite dentition Therefore, the indirect resin restorations which produced differently based on their mechanical features have been developed. The CAD/CAM resin blocks used have some benefits over the glass-ceramic blocks. They produced less tear and wear on opposite tooth structures, have few micro-cracks during production, and less fragile which can improve the marginal adaptation of restorations [5,6].
The resin cement materials are considered contemporary cement materials. They have physical properties which considered to be superior to that of conventional cement materials, which lead to enhance retention of a restoration [7]. Furthermore, the preheated composite resin was suggested to be an alternative material for improving restoration performance as the resin composite could be performed better at the restoration margin due to its high inorganic filler content when used as a luting agent [8,9]. Additionally, sonically activated composite also has the advantage of reducing the viscosity of composite up to 87% which is found to be considered as a cementation material for indirect restoration [10].
The objective of this in vitro study was to measure and compare the marginal adaptation of indirect overlay restorations fabricated from two different all-ceramic CAD/CAM materials (lithium disilicate and reinforce composite blocks) before and after cementation with three different cementation protocols (adhesive resin cement, preheated composite, and sonicallyactivated composite).
Materials and Methods
Forty-eight sound human maxillary first premolar teeth with two roots extracted for orthodontic purposes with comparable size were collected for used in this study from a patient with an aged range from (18-22). Forty-eight human maxillary first-premolar teeth were prepared for indirect overlay restorations with butt joint preparation design. The prepared teeth were divided into two main groups of twenty-four teeth each according to the type of CAD/CAM material used for the fabrication of the restorations: Group A: overlays fabricated from lithium disilicate blocks (IPS e.max CAD, Ivoclar Vivadent, Liechtenstein), Group B: overlays fabricated from reinforced resin blocks (BRILLIANT Crios, Coltene/ Whaledent AG, Switzerland). Each group was then further subdivided into three subgroups of eight teeth each according to the cementation protocol used: Subgroups (A1, B1): cemented with adhesive resin cement (RelyX Ultimate, 3M ESPE, USA), Subgroups (A2, B2): cemented with preheated composite (Filtek Z350 XT, 3M ESPE, USA) and Subgroups (A3, B3): cemented with sonically-activated composite (SonicFill 2, Kerr Corp., USA). The teeth were then prepared for receiving indirect overlay restorations with butt joint occlusal preparation design according to adhesthetics clinical protocol for posterior indirect adhesive restoration (PIAR) proposed by Ferraris in 2017 [11]. The preparation was then done using a high-speed air-turbine handpiece with water cooling mounted in a modified dental surveyor. Preparation was done in two steps: occlusal reduction and proximal reduction. The teeth received an occlusal reduction of 1.5 mm by using the Barrel-shaped trapezoid bur, following the slopes of the cusps and the central groove. For the interproximal reduction, a slot preparation design of 1 mm depth was done by using a flat-end diamond fissure held parallel to the long axis of the tooth to produce a roundshoulder finishing line with a width of the gingival floor of the interproximal box of 1.5 mm with rounded inside angles (Figure 1).
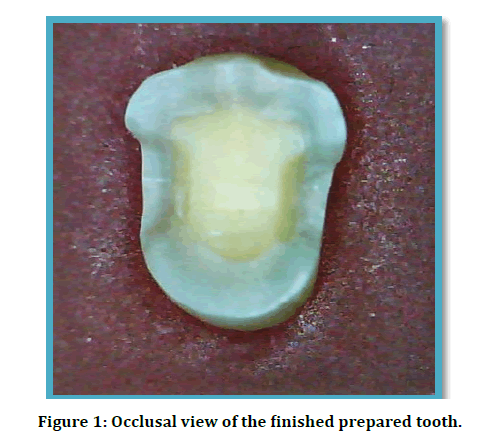
Figure 1: Occlusal view of the finished prepared tooth.
The prepared teeth were then scanned using CEREC Omnicam digital intra-oral scanner, then overlay restorations were designed using Sirona InLab 15.1 software and milled with InLab MC XL milling unit. Overlay restorations of group A were then subjected to crystallization/glaze firing at 840 C0 while those of group B were finished and polished only. Each restoration was then seated on its respective tooth under a standard static load of 5 Kg using a custommade specimen holding device. The digital microscope was then used at a magnification of 230X for vertical marginal gap measurement at four points on each surface of the tooth with the measurements that were done using Image J software. For each specimen, sixteen measurements were taken, and the mean of that measurement was used to be the value of the precementation gap. Before cementation, the surface treatment was done first for both restoration and tooth according to the manufacturers’ instructions then the restorations seated on its respective prepared teeth. For Group A, the surface treatment of restorations were done by application of Hydrofluoric acid (Etching gel < 5%) (Ivoclar Vivadent, Liechtenstein) onto the internal surface of restoration for 20 seconds, then a suction tip was used to remove the etchant from the internal surface of overlay followed by rinsing the internal surface for 15 seconds and the internal surface was then air-dried. The single bond universal was then applied to the internal surface of overlay for 20 seconds using a micro brush then a gentle stream of air was applied for 5 seconds followed by application of light-curing for 10 seconds using the light-curing unit (VALO Cordless curing light, USA). While, for Group B, Surface treatment was carried out with sandblasting using 50 μm aluminum oxide for 10 seconds, 10 mm distance [12]. After that, the overlays were put for 5 minutes in an ultrasonic cleaner followed by application of ONE COAT 7 UNIVERSAL adhesive onto the internal surface of restorations using a disposable dental brush with rubbing the surface for 20 seconds and then gently air-dried for 5 seconds followed by light cure application for 10 seconds. On the other hand, the surface treatment of tooth for all groups was done with the application of 37% Phosphoric acid (N-ETCH) (Ivoclar Vivadent, Liechtenstein) for 15 seconds then thoroughly rinsed for 15 seconds and the excess of water was then removed by suctioning without drying to leave the preparation visibly moist according to the manufacturer's instructions. For cementation: subgroups (A1, B1), the spatula was used for mixing base and catalyst paste of resin cement (RelyX™ Ultimate) (3M ESPE, USA) into homogeneous paste within 20 seconds followed by application of the resin cement onto the entire prepared surface of the tooth then the initial seating of overlay restoration on its respective prepared tooth was done with finger pressure first, then final seating was done by application constant load of 5 kg on restoration using specimen holding device. After removing the excess of cement, light-curing from the buccal and lingual surfaces was done for 20 seconds, then light-curing for 20 seconds from the occlusal direction was done. The sample was then removed from the holding device and kept undisturbed for one hour for a bench set, and then stored in the distilled water for 24 hours [13]. For subgroups (A2, B2), the Filtek Z350 XT composite capsule (3M ESPE, USA) was preheated using a heating device (Ena Heat Micerium, Italy) which was set at 54 C0. The capsule was placed in the heating device for 15 minutes [9], then the capsule was removed from the device and the preheated capsule was injected onto the prepared surface of the tooth by using the campule dispenser. The subsequent steps were then done as illustrated previously for subgroup A1. For subgroups (A3, B3), the SonicFill 2 unidose capsule (Kerr Corp., USA) was attached to the SONICfill handpiece and the extrusion speed of the handpiece was set on level 5, then the handpiece was used to inject the composite onto the prepared surface of the tooth. The subsequent steps were then done as mentioned earlier. The measurement of the marginal gap was then done at the same predetermined points used for the measurement of the marginal gap pre-cementation measurement. The results were then analyzed statistically using independent t-test, one-way ANOVA test, LSD test, and Dunnett T3 test at a level of significance of 0.05.
Results
The descriptive statistics including the mean, standard deviation, minimum and maximum values of the vertical marginal gap in (μm) of two groups and their subgroups pre- and post-cementation are shown in Table 1 and Figure 2.
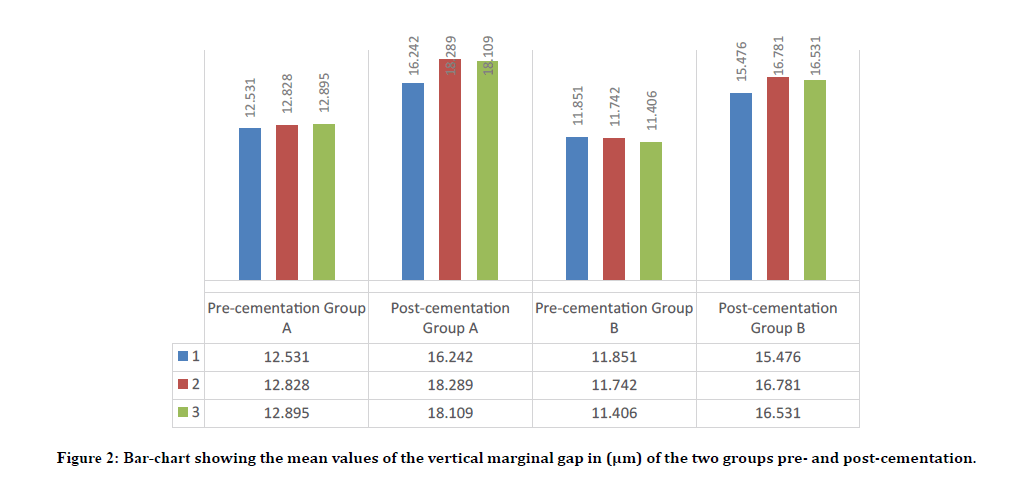
Figure 2: Bar-chart showing the mean values of the vertical marginal gap in (μm) of the two groups pre- and post-cementation.
| Cement | Block type | Pre-cementation | Post-cementation | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Min | Max | Mean | ± SD | Min | Max | Mean | ± SD | ||
| 1 | A | 11.75 | 13.312 | 12.531 | 0.47 | 15.687 | 17.125 | 16.242 | 0.47 |
| B | 10.75 | 12.375 | 11.851 | 0.521 | 14.75 | 15.812 | 15.476 | 0.352 | |
| 2 | A | 11.625 | 13.625 | 12.828 | 0.654 | 16.375 | 19.187 | 18.289 | 0.889 |
| B | 10.5 | 13.5 | 11.742 | 1.188 | 15.562 | 18.125 | 16.781 | 0.959 | |
| 3 | A | 11.875 | 13.937 | 12.859 | 0.819 | 17.312 | 18.625 | 18.109 | 0.496 |
| B | 9.875 | 13.562 | 11.406 | 1.204 | 15.812 | 17.812 | 16.531 | 0.705 | |
Table 1: Descriptive statistics of the vertical marginal gap in (μm) of both groups pre- and post-cementation.
From the above table and Bar-chart, it can be seen that pre-cementation, subgroup B3, in which the overlays were fabricated from Brilliant Crios recorded the lowest mean value of marginal gap (11.406), while the highest mean value of marginal gap was recorded by subgroup A3 in which overlays were fabricated from IPS e.max CAD (12.895).
Meanwhile, there is a general increase in the mean values of the marginal gap among all groups post-cementation. Subgroup B1 recorded the lowest mean value of marginal gap in which the overlays were fabricated from Brilliant Crios and cemented with resin cement (15.476), while the highest mean value of marginal gap was recorded by subgroup A2, in which the overlays were fabricated from IPS e.max CAD and cemented with preheated composite material (18.289).
Pre-cementation
Independent t-test was used for comparison of the marginal gap of the corresponding subgroups of both block types at the level of the significance of 0.05 as seen in Table 2. From the below table, a statistically significant difference was seen between both groups’ pre-cementation (p < 0.05).
| Subgroups | Mean difference | T | Df | P | |
|---|---|---|---|---|---|
| A1 | B1 | 0.68 | 2.741 | 14 | 0.016S |
| A2 | B2 | 1.086 | 2.264 | 14 | 0.040S |
| A3 | B3 | 1.453 | 2.822 | 14 | 0.014S |
Table 2: Independent t-test for comparison of the marginal gap of both subgroups’ Pre-cementation.
Post-cementation
Independent t-test was also used for comparison of the marginal gap between the corresponding subgroups of both block types at the level of the significance of 0.05 as shown in Table 3. From the below table, a highly significant difference was seen between both block materials (p ˂ 0.01)./p>
| Subgroups | Mean difference | T | Df | P | |
|---|---|---|---|---|---|
| A1 | B1 | 0.766 | 3.691 | 14 | 0.002HS |
| A2 | B2 | 1.508 | 3.261 | 14 | 0.006HS |
| A3 | B3 | 1.578 | 5.174 | 14 | 0.000HS |
Table 3: Independent t-test for comparison of the marginal gap of both groups' post-cementation.
For comparison of the effect of type of cementation protocols used on the marginal gap, One-way ANOVA test was used at the level of significance of 0.05 as seen in Table 4. From the table below, there was a statistically highly significant difference among the different subgroups of each block type (p ˂ 0.01).
| Block type | Subgroups | ± SD | F | P |
|---|---|---|---|---|
| A | A1 | 0.47 | 24.54 | 0.000HS |
| A2 | 0.889 | |||
| A3 | 0.496 | |||
| B | B1 | 0.352 | 7.47 | 0.004HS |
| B2 | 0.959 | |||
| B3 | 0.705 |
Table 4: One-way ANOVA test for comparison of the effect of type of cementation protocols on the marginal gap of both block types.
The post hoc test was used for comparing the effect of different cementation protocols on the marginal gap within the same group at the level of significant 0.5 as seen in Table 5. From this table, it can be seen that for both block types, there was a statistically highly significant (p< 0.01) and significant difference (p < 0.05) between the subgroups cemented with resin cement (A1, B1) and those subgroups cemented with preheated and sonically-activated composite (A2, B2 and A3, B3) respectively, with a statistically nonsignificant difference with latter two subgroups (p>0.05).
| Block type | Post hoc test | Subgroups | Subgroups | Mean Difference | P |
|---|---|---|---|---|---|
| A | LSD | A1 | A2 | -2.047 | 0.000HS |
| A3 | -1.868 | 0.000HS | |||
| A2 | A3 | 0.18 | 0.585NS | ||
| B | Dunnett T3 | B1 | B2 | -1.305 | 0.016H |
| B3 | -1.055 | 0.010H | |||
| B2 | B3 | 0.25 | 0.909NS |
Table 5: Post hoc tests for comparison of the effect of the different cementation protocols on the marginal gap within the same group.
Discussion
The measurement of the vertical marginal gap is considered the most frequent method used to measure the accuracy of the fit of the restoration [14]. Marginal gaps of less than 120 μm are considered clinically acceptable [15-18].
The results of this study showed that the marginal gap of all subgroups was below the clinically acceptable limit.
In previous studies, for measurement of the marginal gap, the restoration was fitted on the abutment and hold in place with a screw holding device. This procedure is subjective to inaccuracies. Therefore, a new specimen holding device was specially designed and fabricated for this study. This device is an electro-hydraulically controlled preset at 5 Kg load. Therefore, load application is more precise and there is no need for continuous calculation of the load with each application as in previous devices, thus reducing the operator fatigue and saves time.
Before cementation, for both block types, there were statistically significant differences between them. The overlays fabricated from lithium disilicate showed greater marginal gaps than overlays fabricated from the reinforced composite block. This might be attributed to the following:
1. The difference in the post-milling treatment of both CAD/CAM materials: the lithium disilicate required an additional step (post-milling crystallization) to reach maximum esthetic and mechanical properties. The post-milling crystallization firing was found to cause 0.2% -0.3% shrinkage which caused an increase in the marginal gap of the lithium disilicate group [19]. This could be not accurately accounted for by the CAD/CAM software used in this in-vitro study. Gold et al. studied the effect of the crystallization firing process on the marginal gap of lithium disilicate crowns using leucite-reinforced glassceramic blocks (IPS Empress CAD) and lithiumdisilicate blocks (IPS e.max CAD) before and after crystallization firing. Gold et al. concluded that the crystallization firing method resulted in a significant increase in the marginal gap size, which was related to the shrinkage that occurred in lithium disilicate crown due to the firing process. Also, Kim et al. studied the marginal and internal fitness of lithium disilicate crowns before and after the crystallization method. Kim et al. found statistically significant differences in marginal and internal fitness measurements in all areas before and after the crystallization firing method but with the gap still within the clinically acceptable limit [20].
2. The difference in the machinability of both block materials: the lithium disilicate is harder with the high elastic modulus (95 GPa) as compared with reinforced composite with a low elastic modulus (10.3 GPa). This increased hardness caused difficulty in milling of lithium disilicate with more time required for milling which in turn could lead to an increase in the marginal discrepancy [21, 22]. Furthermore, the hardness of lithium disilicate could cause the wearing of the milling bur of CAD/CAM machine, since the continuous milling may have a role in their cutting ability of milling bur which in turn led to discrepancies in the marginal area of the restorations. Azarbal et al. studied the marginal fit of two CAD/CAM material: lithium disilicate and hybrid ceramic. They found that after continuous milling of fifteen coping of lithium disilicates group, the marginal gap was a significant increase from coping #9 to #15 with a mean value of marginal gap 132 μm for the coping #15. Azarbal et al. (2018) attributed these findings to the wear of milling burs which in turn affected cutting accuracy, therefore they suggested that the bur should be changed after milling of 8 lithium disilicate coping in contrary to manufacturer recommendations [23].
After cementation, both block types cemented with three different types of cement showed an increase in the marginal gap. This finding agrees with the previous study which stated that the cementation process caused an increase in the discrepancy of the vertical marginal gap [24-27].
However, in this study, the increase in the marginal gap was less as compared with the previous study and this could be attributed to the design of preparation chosen which created a non-retentive preparation design that produced overlay restorations with better marginal adaptation [28]. Kim et al. study the effect of preparation design on marginal and internal fitness of partial ceramic restoration using two different designs including a nonretentive preparation design with horizontal reduction of cusps and a retentive preparation design with traditional cusp capping. Kim et al. used the CEREC 3 system for the fabrication of the partial ceramic crown from IPS Empress CAD. Kim et al. found that the non-retentive design produced better marginal adaptation than the retentive design. Another reason might be related to the using of a more precise holding device used in this study because this device applied automatically an accurate preset load of 50 N during the cementation process as compared with the previous study which used a manual holding device to applied that load.
Post-cementation, regarding the type of CAD/ CAM material, the overlay restorations fabricated from the reinforced composite and cemented three types of cement recorded lower marginal gap as compared with overlay restorations fabricated from lithium disilicate as in precementation with statistical differences (either significant or highly significant difference). The explanation for this might be due to the composite resin block having a lower precementation marginal gap relative to lithium disilicate, meaning that the rise in the marginal gap between all block forms was similar after cementation.
Concerning the type of luting cement, for both block types, the overlays cemented with resin cement showed less marginal gap with statistical differences (either significant or highly significant difference) than those cemented with preheated and sonically activated composite material. This might be related to the following reasons:
1. The difference in film thickness of cement materials: since the resin cement produced a lower marginal gap post-cementation as compared with pre-heated composite and sonically-activated composite which could be related to a low film thickness of resin cement which produced a better marginal adaptation through reducing discrepancy in the final restoration seating. Because the seating of restorations affected by the film thickness of the cement so that as film thickness decrease, the internal fitness of restoration increase [29,30]. Sampaio and colleagues studied film thickness of the various luting cement. They found that the flowable composite resins and the veneer cement showed a lower film thickness than the restorative composite resins film thickness, whether preheated or not [31]. Goulart et al. studied the effect of pre-heating on the film thickness of three different luting material include: nanofilled% (Z350% XT/3MESPE), micro-hybrid (Opallis/FGM), with two different temperature include: room temperature and pre-heating and resin cement (AllCem/FGM). The two composite materials were heated at (64 C0) using a heating device (CalSet/AdDent). After heating the film thickness for nano-fill composite and micro-hybrid was (59.7 μm, 45.3 μm) respectively while the resin cement record the lowest film thickness was 28.2 μm [32]. Furthermore, Blalock and colleagues stated that an average film thickness of preheated resin composites at 54 C0 (140 microns) while (35 microns) for flowable resin composites [33]. However, there is a lack of data in the literature about the film thickness of sonically-activated composite (SonicFill 2) which could be attributed to the rapid drop of the viscosity of the material into normal viscosity once sonic activation has been stopped.
2. Cement spacer can play an important role concerning the consistency of luting materials, therefore resin cement has a low film thickness produced a better marginal adaptation, and allowed proper seating of restorations, in contrast to thick and more viscous pre-heated and sonically-activated composite which could be prevented the proper seating of restorations [34]. Since the cement spacer was preset on (100 μm) for all overlay restorations for both block types in this study, therefore with high film thickness cement, it is supposed to increase the amount of spacer to provide more space and to allow proper seating of restoration when using a high film thickness cement as a luting agent.
Conclusion
Within the limitations of this in vitro study, the following conclusions could be drawn:
The indirect overlay restorations fabricated from Brilliant Crios blocks showed better marginal adaptation than those fabricated from lithium disilicate blocks, regardless of the type of cementation protocols used.
The marginal gap of indirect overlay restorations increased post-cementation with either type of cement, regardless of the type of CAD/CAM block.
The marginal adaptation of overlay restorations of all groups was below the clinically acceptable limit.
Cementation with adhesive resin cement provided significantly better marginal adaptation than cementation with preheated composite or sonically activated composite, with non-significance difference between the latter two techniques.
References
- Torbjörner A, Fransson B. A literature review on the prosthetic treatment of structurally compromised teeth. 2004; 17.
- Jotkowitz A, Samet N. Rethinking ferrule–a new approach to an old dilemma. 2010; 209:25-33.
- Colpani JT, Borba M, Della Bona Á. Evaluation of marginal and internal fit of ceramic crown copings. 2013; 29:174-180.
- Lima FF, Neto CF, Rubo JH, et al. Marginal adaptation of CAD-CAM onlays: Influence of preparation design and impression technique. J Prosthetic Dent 2018; 120:396-402.
- Gopal SV. CAD-CAM and all ceramic restorations, current trends and emerging technologies: A review. Int J Orofac Res 2017; 2:40.
- Kavut İ, Uğur M, Tanrıkut ÖO. Evaluation of the adhesion of different CAD/CAM materials with self etch/adhesive resin cements. J Dent Med Sci 2019; 18:51-54.
- Burke FT. Resin luting materials. 2019; 46:371-378.
- Goulart M, Borges Veleda B, Damin D, et al. Preheated composite resin used as a luting agent for indirect restorations: Effects on bond strength and resin-dentin interfaces. Int J Esthet Dent 2018; 13:86-97.
- Rickman LJ, Padipatvuthikul P, Chee B. Clinical applications of preheated hybrid resin composite. Br Dent J 2011; 211:63.
- Elzoheiry A, Hafez A, Amr H. Microhardness testing of resin cement versus sonic bulk fill resin composite material for cementation of CAD/CAM composite block with different thickness. Egyptian Dent J 2019; 65:78.
- Ferraris F. Posterior indirect adhesive restorations (PIAR): Preparation designs and adhesthetics clinical protocol. Int J Esthet Dent 2017; 12:482-502.
- Reymus M, Roos M, Eichberger M, et al. Bonding to new CAD/CAM resin composites: Influence of air abrasion and conditioning agents as pretreatment strategy. Clin Oral Investigations 2019; 23:529-538.
- Shahrbaf S, Van Noort R, Mirzakouchaki B, et al. Fracture strength of machined ceramic crowns as a function of tooth preparation design and the elastic modulus of the cement. Dent Materials 2014; 30:234-241.
- Wolfart S, Wegner SM, Al-Halabi A, et al. Clinical evaluation of marginal fit of a new experimental all-ceramic system before and after cementation. Int J Prosthodont 2003; 16.
- Akbar JH, Petrie CS, Walker MP, et al. Marginal adaptation of cerec 3 CAD/CAM composite crowns using two different finish line preparation designs. J Prosthodont 2006; 15:155-163.
- Baig MR, Tan KB, Nicholls JI. Evaluation of the marginal fit of a zirconia ceramic computer-aided machined (CAM) crown system. J Prosthetic Dent 2010; 104:216-227.
- Abduo J, Lyons K, Swain M. Fit of zirconia fixed partial denture: A systematic review. Journal Oral Rehab 2010; 37:866-876.
- Ender A, Zimmermann M, Attin T, et al. In vivo precision of conventional and digital methods for obtaining quadrant dental impressions. Clin Oral Investigations 2016; 20:1495-1504.
- Gold SA, Ferracane JL, da Costa J. Effect of crystallization firing on marginal gap of CAD/CAM fabricated lithium disilicate crowns. J Prosthodont 2018; 27:63-66.
- Kim JH, Oh S, Uhm SH. Effect of the crystallization process on the marginal and internal gaps of lithium disilicate CAD/CAM crowns. BioMed Res Int 2016; 2016.
- Alamoush RA, Silikas N, Salim NA, et al. Effect of the composition of CAD/CAM composite blocks on mechanical properties. BioMed Res Int 2018; 2018.
- Yara A, Goto SI, Ogura H. Correlation between accuracy of crowns fabricated using CAD/CAM and elastic deformation of CAD/CAM materials. Dent Material J 2004; 23:572-576.
- Azarbal A, Azarbal M, Engelmeier RL, et al. Marginal fit comparison of CAD/CAM crowns milled from two different materials. J Prosthodont 2018; 27:421-428.
- Borges GA, Faria JS, Agarwal P, et al. In vitro marginal fit of three all-ceramic crown systems before and after cementation. Operative Dent 2012; 37:641-649.
- Abdullah LS, Ibraheem AF. The effect of finishing line designs and occlusal surface reduction schemes on vertical marginal fit of full contour CAD/CAM zirconia crown restorations (A comparative in vitro study). Int J Dent Oral Health 2017; 4:1-6.
- Al-Hawwaz ZM, Ibraheem AF. Microbiology, Marginal and internal fitness of full contour CAD/CAM Fabricated zirconia crowns using different digital intra-oral scanners (An In vitro study). J PurE PPliEd Microbiol 2018; 12:839-844.
- Abdulla HA, Majeed MA. Assessment of bioactive resin-modified glass ionomer restorative as a new CAD/CAM material part II: Fracture strength study. J Res Med Dent Sci 2019; 7:74-79.
- Goujat A, Abouelleil H, Colon P, et al. Marginal and internal fit of CAD-CAM inlay/onlay restorations: A systematic review of in vitro studies. J Prosthet Dent 2019; 121:590-597.
- Alghazzawi TF, Liu PR, Essig ME. The effect of different fabrication steps on the marginal adaptation of two types of glass‐infiltrated ceramic crown copings fabricated by CAD/CAM technology. J Prosthodont 2012; 21:167-172.
- Anadioti E, Aquilino SA, Gratton DG, et al. Internal fit of pressed and computer-aided design/computer-aided manufacturing ceramic crowns made from digital and conventional impressions. J Prosthet Dent 2015; 113:304-309.
- Sampaio CS, Barbosa JM, Cáceres E, et al. Volumetric shrinkage and film thickness of cementation materials for veneers: An in vitro 3D microcomputed tomography analysis. J Prosthet Dent 2017; 117:784-791.
- Goulart M, Damin DF, Melara R, et al. Effect of pre-heating composites on film thickness. J Res Dent 2013; 1:274-280.
- Blalock JS, Holmes RG, Rueggeberg FA. Effect of temperature on unpolymerized composite resin film thickness. J Prosthet Dent 2006; 96:424-432.
- Azar B, Eckert S, Kunkela J, et al. The marginal fit of lithium disilicate crowns: Press vs. CAD/CAM. Brazilian Oral Res 2018; 32.
Author Info
Zaidoon Hasan Mohammed* and Manhal A Majeed
Department oDepartment of Conservative Dentistry, College of Dentistry, University of Baghdad, IraqCitation: Zaidoon Hasan Mohammed, Manhal A Majeed, Effect of Cementation Protocol on the Marginal Adaptation of Indirect Overlay Restorations Fabricated from Two Different All-Ceramic CAD/CAM Materials, J Res Med Dent Sci, 2020, 8 (7): 518-525.
Received: 03-Nov-2020 Accepted: 10-Nov-2020 Published: 17-Nov-2020
