Research - (2021) Volume 9, Issue 7
Effect of Different Bonding Systems on Shear Bond Strength of Buccal Tubes Bonded to Various Restorative Materials: An In Vitro Study
Mohammed Razzaq Hussein*, Mehdi Abdulhadi Mehdi and Abeer Basim Mahmood
*Correspondence: Mohammed Razzaq Hussein, Department of orthodontics, College of Dentistry, Iraq, Email:
Abstract
Introduction: Orthodontic bonding to restorative surfaces poses a clinical dilemma as it does not follow a single universally accepted procedure. Aims: This study aimed at evaluating shear bond strength (SBS) and adhesive remnant index (ARI) of buccal tubes bonded to different restorative surfaces using three bonding systems. Materials and Methods: The sample included 54 restorative surfaces divided into three groups consisting of amalgam, composite and feldspathic porcelain (n=18), randomly divided into three bonding subgroups: A, B and C (n=6). In subgroup A, conventional bonding was conducted using Transbond XTTM. In subgroups B and C, Assure Plus® and ScotchbondTM were used, respectively. Six human molars were bonded with standard acid-etching technique and served as control. All specimens were thermo cycled 5000 times between 5°C and 55°C before SBS testing. Bond failure sites were classified using the ARI system. The results were statistically analyzed using one-way analysis of variance (ANOVA) and Kruskal-Wallis tests (P ≤ 0.05). Results: For all bonding systems used, SBS values were significantly lower on both amalgam and porcelain than enamel, while no significant difference was found between composite and enamel. ARI scores showed no significant difference among the bonding systems within each restorative group. Conclusion: The three bonding systems tested have produced SBS values above the clinically appropriate level in all restorative groups. Scotch bond created clinically acceptable SBS with no need for additional primer, and relatively low risk of surface fracture upon debonding. Therefore, it might be helpful in orthodontic bonding to the restorative surfaces tested in this study.
Keywords
Buccal tubes, Shear strength, Amalgam, Composite, Feld spathic Porcelain, Thermo cycling
Introduction
An increasing proportion of adults are undergoing orthodontic treatment, and many may present with restorations in some parts of their dentition [1]. Conventional bonding preceded by acid etching to condition the enamel is the approach of choice when the bonding surface of the tooth is intact; however, orthodontists frequently encounter restorative surfaces that, in turn, may consist of different materials, most notably alloys, ceramics and composite resins [2]. Since bonding to restorative and prosthetic surfaces does not follow a single universally accepted procedure, modifications in techniques and materials are essential to produce reliable bonds to non-enamel surfaces [3].
Traditionally, metal bands have been used for securing orthodontic attachments to molars. More recently, bonding of buccal tubes with the use of dental adhesives has become preferred to banding in fixed orthodontic appliances. Disadvantages of banding compared to bonding include higher risks of accumulation of dental plaque with increased incidence of gingival and periodontal diseases, the necessity of an additional appointment for separation of the adjacent teeth and fitting of the molar band, the need for an additional inventory, and higher risk of bacteraemia which necessitates the use of antibiotic prophylaxis for at-risk patients (e.g. patients with congenital heart disease) [4].
Adhesion to amalgam is facilitated by a variety of complex monomers including but not limited to 4- methacryloxyethyl trimellitate anhydride (4-META) and Methacryloyloxi-decyl-dihydrogen-phosphate (MDP) which function as connecter agents by chemically bonding to the oxidized surface of metals and alloys [5-7].
In operative dentistry, the majority of investigators considered the application of an intermediate agent to be essential for higher composite repair strength [8]. Unlike restorative dentistry, orthodontic treatment does not aim for a long-lasting bond. Instead, optimum orthodontic bonding to the composite surface would allow the treatment to proceed without bond failure [9].
A wide range of mechanical and chemical surface modifications are suggested in the literature to facilitate bonding to various types of porcelain. Application of hydrofluoric acid (HF) has been advocated as a chemical surface treatment to increase the bond strengths, as it reacts with and dissolves the glass phase of ceramics, creating retentive microchannels without reducing the flexural strength of the porcelain [10]. In a systematic review of orthodontic bonding to porcelain, the application of silane was found to significantly increase the bond strength of orthodontic attachments to feldspathic porcelain [11].
Preferably, bond strengths on restorative materials should be comparable to those achieved on enamel to minimize the incidence of bond failure. On the other hand, excessively high strengths are not desirable and must be avoided to allow for smooth debonding procedures without damaging, breaking or dislodging the restorations [2].
Theoretically, an ideal primer would not provide clinically acceptable bond strengths to enamel and nonenamel surfaces without being technique-sensitive nor requiring a material-specific pre-treatment, and thus reducing the cost and effort involved in bonding of fixed orthodontic appliances [3].
Universal bonding agents have been introduced to clinical practice since 2011 and are intended to provide sufficient bond strengths to dentin, enamel, metal, ceramic, zirconia and composite without the need for a separate primer [12]. Examples include Assure® Plus All Surface Bonding Resin and ScotchbondTM Universal Adhesive, both of which contain the monomer MDP, which bonds to other materials besides enamel, such as metal and ceramic [13]. Additionally, Scotchbond also contains silane, which facilitates bonding to porcelain [11].
The aims of this in vitro study were to determine which bonding system provides the most effective SBS value for orthodontic treatment on each restorative surface while exerting minimum risk of damaging the surface during debonding procedure; and to evaluate whether or not a universal bonding agent containing silane (Scotchbond) is able to produce acceptable results on all tested restorative surfaces.
Materials and Methods
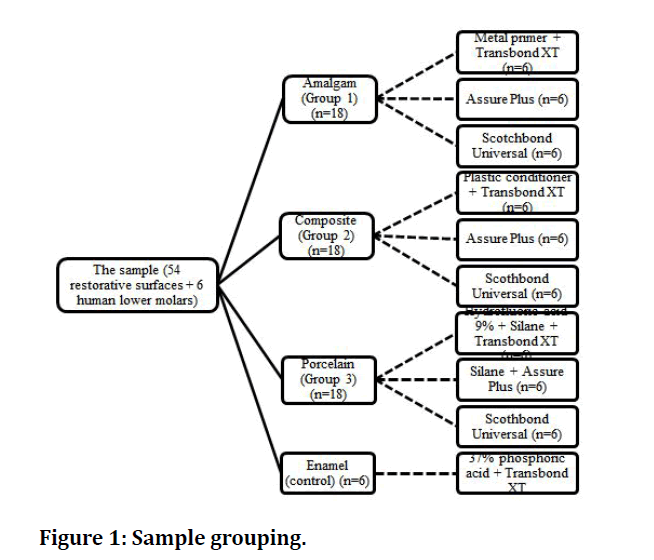
The sample included 54 restorative surfaces divided into three groups consisting of amalgam, composite and feldspathic porcelain (n=18). In each group, all surfaces were randomly divided into three bonding subgroups: A, B and C (n=6). Additionally, 6 human molars were bonded with the conventional acid-etching technique and served as control (Figure 1).
Figure 1: Sample grouping.
The teeth used were extracted for general dental reasons and were collected from private dental clinics. Instantly after extraction, teeth were debrided by water to remove soft tissue remnants, debris, or blood, and examined under a stereomicroscope (LeicaTM, Leitz, Wetzlar, Germany) at a tenfold magnification to verify that they were generally intact with no caries, restoration, enamel cracks, or surface irregularities; and had no history of previous endodontic, orthodontic or bleaching treatments.
Sample preparation
For the amalgam and composite samples, thirty-six dent form teeth of lower first molars (Columbia Dentoform, Long Island City, NY, USA) with identical size and shape were used. Each dentoform tooth had a cylindrical hole in its root that increased the retention inside the acrylic blocks. Class V cavities were prepared in buccal surfaces of dentoform teeth using round and fissure diamond burs in a high speed hand piece. The dimension of each cavity was determined carefully with the help of a digital caliper. The cavities were extended beyond the dimensions of the buccal tubes (> 3.3 mm in length, > 2.72 mm in width) and had a depth of 3 mm.
Alloy amalgam capsules of lathe-cut particle shape (SDI Limited, Bayswater, Victoria, Australia) were mixed and condensed into eighteen cavities. The amalgam was left to set for 24 hours. The other eighteen cavities were filled with the nano-filled Filtek Z350 XT Universal Restorative composite (3M ESPE Dental Products, St. Paul, Minnesota, USA) in three increments, each increment cured for 20 s.
For porcelain samples, a digital scan of a dentoform was made and used to construct eighteen zirconia crowns. Using the CAD-CAM technology and during the designing phase, a class V buccal cavity was placed on the buccal surface of each zirconia crown to receive the feldspathic porcelain (VitaVM. 9, Vita, Postfach, Germany). The cavity was extended beyond the dimensions of the buccal tubes and had a depth of 3 mm. To improve the retention inside the acrylic blocks, a groove was made on the radicular area of the crowns. Following milling and sintering of zirconia crowns, the feldspathic porcelain was stacked into the buccal cavities, using the traditional condensation technique, followed by sintering for 1.5 hour to a final temperature of 910o C. Finally, glaze layer was applied and firing was performed to a maximum temperature of 900o C.
All of the materials were prepared and used according to the manufacturers’ instructions.
Every three samples were fixed about 1cm apart from each other on a metal slide secured to a dental surveyor to ensure that the middle third of the buccal surface of each samples was parallel to the analyzing rod of the surveyor so that the force is applied at a right angle to the tooth/tube interface. An acrylic mold was then made for each three samples.
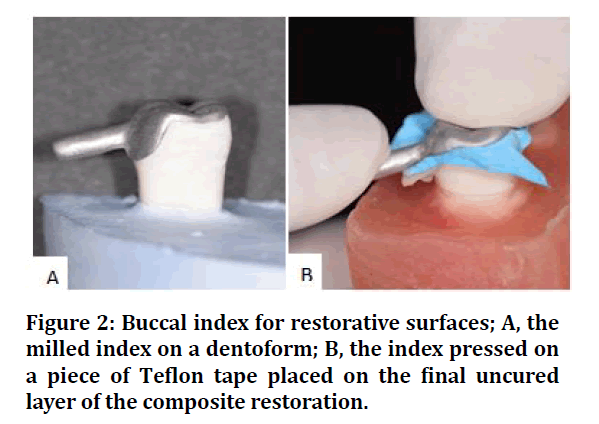
To replicate the anatomy of the bonding surface of all restorative samples for better standardization, a metal index was initially prepared from a digital scan of the of an intact dentofrom tooth using the CAD-CAM technology. The index was extended to cover the occlusal surface in addition to the buccal surface, to ensure its correct placement during application, and was pressed over the restorative surfaces immediately after their placement. For composite samples, a piece of teflon was used to cover the final uncured increment before pressing the index (Figure 2).
Figure 2: Buccal index for restorative surfaces; A, the milled index on a dentoform; B, the index pressed on a piece of Teflon tape placed on the final uncured layer of the composite restoration.
Each bonding surface was polished for 10 s using polishing brushes with non-fluoridated pumice (PD, Vevey, Switzerland) for enamel, green and brown polishing rubber points for amalgam (Shofu Inc., Kyoto, Japan), and silicone polishers for composite and ceramic samples (BrioShine Feather Lite, Brasseler, Savannah, USA). Afterwards, washing of samples was performed for 10 seconds, followed by drying with oil-free air for another 10 seconds.
Sandblasting was carried out on the restorative samples before bonding with 50-micron aluminum oxide from a distance of 10 mm at a pressure of 2.5 bars for 4 s using an air-abrasion device (EMS, Chemin de la Vuarpillieère, Nyon, Swiss), and then rinsed and dried.
Bonding procedure
(i) Conventional bonding system (subgroup A): In amalgam group, a thin coat of Reliance Metal Primer (Reliance Orthodontic Products, Itasca, Illinois, USA) was applied and allowed to rest for 30 s. In composite group, Plastic Conditioner (Reliance Orthodontic Products, Itasca, Illinois, USA) was applied and allowed to dry for 60 s. In porcelain group, the surface was covered by a thin layer of 4% HF (Reliance Orthodontic Products, Itasca, Illinois, USA) allowed to rest for 4 minutes, then wiped off with a cotton pellet. The surface was then rinsed thoroughly for 30 s, air- dried and coated with a thin layer of porcelain conditioner (silane) (Reliance Orthodontic Products, Itasca, Illinois, USA). The latter was allowed to rest for 60 s Transbond XT Primer (3M Unitek, Monrovia, Calif, USA) was applied afterwards to all surfaces in this group.
(ii) Assure Plus (subgroup B): One coat of Assure Plus (Reliance Orthodontic Products, Itasca, Illinois, USA) was applied to each amalgam and composite surface and dried with oil-free air for 5 s then light cured for 10 s. In the porcelain group, an additional primer was required; the surface was painted with a thin layer of Reliance Porcelain Conditioner and left to rest for 60 s and then one layer of Assure Plus was placed, air-dried for 5 s and light cured for 10 s.
(iii) Scotchbond Universal Adhesive (subgroup C): each restorative surface was coated with one layer of Scotchbond Universal Adhesive (3M Deutschland, Gmbh, Neuss, Germany) and rubbed for 20 s, air-dried for 5 s and light cured for 10 s. No additional primer was added.
Six human lower molars were bonded using the conventional acid etching technique and served as control. The enamel surface was etched with 37% phosphoric acid for 30 s, washed with water spray for 20 s, dried with oil-free air for 20 s. The Transbond XT Primer was used afterwards, then thinly dispersed with air.
Following the priming procedures, bonding was conducted similarly for all groups, using Transbond XT Adhesive Paste (3M Unitek, Monrovia, Calif, USA) which was applied to the base of the buccal tubes. The tubes were then positioned in the middle third of the buccal surface of the samples. A constant load of 200 gm was placed on each buccal tube for 20 s to ensure equal pressure. A LED curing unit (Eighteeth, Changzhou City, Jiangsu Province, China) was then used for polymerizing the adhesive paste for 40 seconds (10 seconds from each side of the buccal tube) from a distance of 5 mm with an intensity of 1600 mw/cm2. To allow better comparability, only Ortho-Cast M-Series buccal tubes (Dentaurum, Ispringen, Germany) with a bonding surface area of 13.15 mm2 were used.
Sample hydration and thermo cycling
Following bonding of buccal tubes, the bonded teeth were stored in distilled water at 37°C for 24 h, then subjected to a thermocycling regimen of 5000 cycles between cold and hot water baths of 5°C and 55°C with a dwell time of 30 s in each bath and transfer time of 5s.
Shear bond strength test
Shear test was accomplished using Tinius Olsen universal testing machine (H50KT, England), with a loading cell of 50 kilogram and a crosshead speed of 0.5 mm/min and a customized chisel rod. The shear bond strength in MPa was measured by dividing the maximum load-at-failure in Newton by the bonding surface area in mm2.
Estimation of the adhesive remnant index
Following shearing-off, the base of the buccal tubes and the bonding surfaces were examined using a stereomicroscope (LeicaTM, Leitz, Wetzlar, Germany) at tenfold magnification and the mode of bond failure was assessed using the adhesive remnant index as follows:
Score 0 = no adhesive left on the tooth; score 1 = less than 50% adhesive left on the tooth; score 2 = more than 50% adhesive left on the tooth; score 3 = all the adhesive is left on the tooth, score 4 = surface fracture.
Statistical analysis
Statistical analysis of data was performed using SPSS StatisticsTM software version 26.0 (IBM Company, New York, USA). Normality of data distribution was tested using the Shapiro-Wilk test, which showed that SBS values were normally distributed while ARI scores were not normally distributed. Analysis of statistical differences was carried out using ANOVA for SBS test and Kruskal-Wallis test for ARI scores. The significance level was set at p <=0.05.
Results
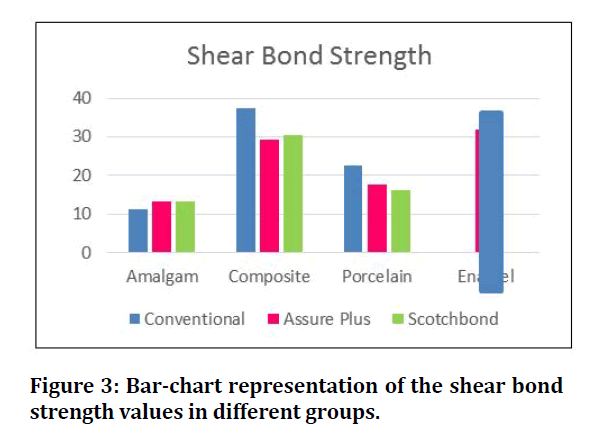
The means and standard deviations of SBS for each group are given in (Table 1) and (Figure 3).
Table 1: Descriptive statistics of the shear bond strength test of different groups.
| Group | Primer | Mean |
|---|---|---|
| Amalgam | Conventional | 11.30 ± 2.81 |
| Assure Plus | 13.40 ± 2.28 | |
| Scotchbond | 13.16 ± 2.18 | |
| Total | 12.62 ± 2.49 | |
| Composite | Conventional | 37.28 ± 1.73 |
| Assure Plus | 29.17 ± 3.87 | |
| Scotchbond | 30.46 ± 5.73 | |
| Total | 32.30 ± 5.33 | |
| Porcelain | Conventional | 22.45 ± 2.25 |
| Assure Plus | 17.65 ± 2.95 | |
| Scotchbond | 16.09 ± 2.77 | |
| Total | 18.73 ± 0.88 | |
| Enamel (control) | Conventional | 31.85 ± 4.26 |
Figure 3: Bar-chart representation of the shear bond strength values in different groups.
Among all tested groups, the highest mean SBS value was produced by conventional priming of composite (37.28 ± 1.73 MPa), while conventional priming of amalgam produced the lowest mean value (11.30 ± 2.81 MPa).
Comparison of mean difference of SBS between the control group with each restorative group was performed using ANOVA test and showed both significant and nonsignificant differences. The Post-hoc Tukey’s test was carried out for multiple comparisons to reveal the differences among the tested groups. Inferential Statistics of SBS are presented in (Table 2).
Table 2: Comparison of the mean shear bond strength between enamel and amalgam groups by ANOVA and Post-hoc Tukey’s test.
| Group | ANOVA test | Tukey’s test | ||
|---|---|---|---|---|
| F-test | P-value | Between subgroups | P-value | |
| Control-Amalgam | 62.018 | 0.000 | Control-A1 | 0 |
| Control-A2 | 0 | |||
| Control-A3 | 0 | |||
| A1-A2 | 0.629 | |||
| A1-A3 | 0.711 | |||
| Control-Composite | 4.458 | 0.016 | A2-A3 | 0.999 |
| Control-B1 | 0.107 | |||
| Control-B2 | 0.858 | |||
| Control-B3 | 0.992 | |||
| B1-B2 | 0.016 | |||
| B1-B3 | 0.048 | |||
| Control-Porcelain | 30.43 | 0.000 | B2-B3 | 0.949 |
| Control-C1 | 0 | |||
| Control-C2 | 0 | |||
| Control-C3 | 0 | |||
| C1-C2 | 0.069 | |||
| C1-C3 | 0.011 | |||
| C2-C3 | 0.827 | |||
In the amalgam group, SBS values were highly significantly lower compared to enamel for all bonding subgroups. However, there was no significant difference between the three bonding systems.
In the composite group, regardless of the bonding system used, there was no significant difference compared to enamel. However, the conventional bonding system produced significantly higher SBS than Assure Plus and Scotchbond, while there was no significant difference between Assure Plus and Scotchbond.
In the feldspathic porcelain group, all tested bonding systems had highly significantly lower SBS than standard bonding of enamel. Furthermore, conventional porcelain bonding achieved significantly higher SBS than Scotchbond, while there was no significant difference between the conventional system and Assure Plus and between Assure Plus and Scotchbond.
As the ARI scores were not normally distributed, the Kruskal–Wallis test was used for comparison of mean differences and showed no statistically significant difference between adhesive subgroups within each restorative group, as demonstrated in (Table 3).
Table 3: Comparison the ARI among different primers within each restorative group using Kruskal-Wallis test.
| Group | Df | P-value |
|---|---|---|
| Amalgam | 2 | 1.000 (NS) |
| Composite | 2 | 0.823 (NS) |
| Porcelain | 2 | 0.356 (NS) |
All amalgam samples had ARI of score 0 (100%).
In the composite group, score 0 had no occurrence; and samples showed a mixed distribution of scores 1,2,3 and 4. More importantly, surface fracture occurred in 33.3% in each of the Assure Plus and the Scotchbond groups, and in 16.7% in the conventional group.
The majority of porcelain samples had score 0, while score 3 was not found in this group. Porcelain surface was fractured in 33.3% in each of the conventional and the Assure Plus groups, and in 16.7% in the Scotchbond group.
Discussion
Although there is no universally accepted value for clinically successful shear bond strength, the 6-8 MPa range suggested in Reynold’s 1975 article has been cited by the vast majority of in vitro studies as a reference [14]. In all of the amalgam, composite and porcelain groups, the three bonding systems tested in this study produced SBS values that were higher than the required range, and therefore they seem to be clinically adequate. In the literature, SBS of brackets bonded to enamel using the traditional etch-and-rinse method ranged from 9 to 35 MPa, however, considering that bonding forces should not be too strong in order to avoid enamel loss after debonding (40-50 MPa), the ideal orthodontic biomaterial should have bonding forces included in the interval of 5 to 50 MPa, even if these limits are more or less theoretical [15].
Caution must be taken, however, when comparing laboratory bond strength studies with each other because of potential variations in test parameters. In fact, SBS tests are very technique-sensitive, and the measurements depend not only on the different material properties, but on the design of the testing arrangement [16]. Factors such as the moment arm length (the horizontals distance between the tip of the debonding chisel and the bonding interface), the angulation of the chisel, the sample shape and the speed of the crosshead might have a direct effect on the SBS test results [17-20].
Irrespective of the type of primer, bonding to amalgam provided significantly lower SBS than standard bonding to enamel. The mean SBS of buccal tubes bonded to amalgam ranged from 11.30 MPa to 13.40 MPa. Additionally, there was no significant difference among the three bonding systems on amalgam in terms of SBS. These results are consistent with findings of previous studies which demonstrated that even with a combined use of both sandblasting and adhesion promoters, bond strength values on amalgam were approximately half or less than half of that achieved by standard bonding to enamel [2,4,5,6,7].
The weaker bond strength on amalgam in comparison to enamel can partly be explained by the rather unusual interaction between mechanical and chemical surface modifications of amalgam to enhance SBS. On one hand, both of MDP and 4-META-containing adhesion promoters form hydrogen bonds with the oxygen and hydroxyl groups in the “oxidized surface” of metals and thus provide chemical bond to amalgam [21]. On the other hand, although sandblasting is one of the most effective means of mechanical surface treatment on amalgam, it minimizes or potentially eliminates the superficial oxide layer [14]. Thus, sandblasting may have a negative impact on the effectiveness of these promoters [21].
All three bonding systems produced SBS values on composite that were statistically similar to that of enamel. This is consistent with the findings of previous studies, where the use of a universal bonding agent provided similar SBS values on both enamel and composite [2,3].
Additionally, within the composite subgroups in the current study, conventional bonding system (Transbond XT + Reliance Plastic Conditioner) produced significantly higher SBS (37.28 ± 1.73 MPa) than Scotchbond (30.46 ± 5.73 MPa) and Assure Plus (29.17 ± 3.87 MPa). This finding might be explained by the lesser viscosity of Plastic Conditioner and consequently better surface infiltration as compared to Assure Plus and Scotchbond.
This minimal viscosity is probably the result of Plastic Conditioner’s simpler chemical structure, which consists primarily of methyl methacrylate resin, as opposed to the complex and sophisticated compositions of Assure Plus and Scotchbond [12].
All tested bonding systems had significantly lower SBS values on porcelain surface than enamel. This finding is supported by the results of previous studies [2,10]. Furthermore, within the porcelain subgroups in the present study, the highest SBS was achieved by conventional bonding (22.45±2.25 MPa), followed by Assure Plus (17.65± 2.95 MPa) and Scotchbond (16.09±2.77 MPa). This result is verified by the conclusion of a systematic review of orthodontic bonding to porcelain, in which the use of HF followed by silane was described as the best bonding protocol in terms of bond strength [11].
The characteristic ability of the HF to etch the surface of porcelain might be the main factor for achieving significantly higher SBS in the conventional bonding group, as HF preferentially dissolves the glass phase of porcelain and thus creates retentive microchannels that particularly improve the SBS [10,22].
Statistical analysis of the distribution of the ARI scores showed no significant difference between adhesive subgroups within each restorative group.
All amalgam samples in the current study, irrespective of the bonding system used, had score 0, indicating that bond failure occurred purely at the amalgam/adhesive interface, with no adhesive left on the amalgam. This result is in agreement with the findings of several other studies, in which score 0 had a percentage of 100% on the surface of amalgam, regardless of the bonding protocol [5,7,19,21].
In the composite group, surface fracture occurred in 33.3% of both Assure Plus and Scotchbond groups, and in 16.7% of the conventional bonding group. These frequencies of restorative composite fracture are lower than those of comparable studies [2,3]. The lower fracture rates might be the result the aging effect of thermocycling [23]. Furthermore, a previous study concluded that the type of the bonded composite affects the ARI, with the nano-filled composite having the highest resistance to fracture upon debonding [24].
No significant difference was found in the ARI distribution on porcelain surface among the different bonding systems in the present study. The majority of the samples had score 0 in the Assure Plus and Scotchbond groups, while the conventional bonding group had mixed scores.
Regarding the porcelain fracture upon deboning (score 4), cohesive fracture occurred in 33.3% of both conventional bonding and Assure Plus samples, and in 16.7% of the Scotchbond samples. The higher frequency of porcelain fracture in both conventional bonding and Assure Plus groups than the Scotchbond group can be linked to the separate silane application which was performed in the first two groups [25].
Conclusion
The three bonding systems tested have shown SBS values above the clinically appropriate level in all restorative groups. Scotchbond created clinically acceptable SBS with no need for additional primer, and relatively low risk of surface fracture upon debonding. Therefore, it might be helpful in orthodontic bonding to the restorative surfaces tested in this study.
References
- Kokich VG, Spear FM. Guidelines for managing the orthodontic-restorative patient. Semin Orthod 1997; 3:3–20.
- Hellak A, Ebeling J, Schauseil M, et al. Shear bond strength of three orthodontic bonding systems on enamel and restorative materials. BioMed Res Int 2016; 6307107.
- Ebert T, Elsner L, Hirschfelder U, et al. Shear bond strength of brackets on restorative materials. J Orofac Orthop 2016; 77:73-84.`
- Wongsamut W, Satrawaha S, Wayakanon K. Surface modification for bonding between amalgam and orthodontic brackets. J Orthodo Sci 2017; 6:129.
- Zachrisson BU, Büyükyilmaz T, Zachrisson Y. Improving orthodontic bonding to silver amalgam. Angle Orthodont 1995; 65:35-42.
- Büyükyilmaz T, Zachrisson BU. Improved orthodontic bonding to silver amalgam. Part 2. Lathe-cut, admixed, and spherical amalgams with different intermediate resins. Angle Orthod 1998; 68:337-344.
- Isman E, Ozsevık S, Yavan MA, et al. Effects of two metal primers on the shear bond strength of orthodontic molar tubes bonded to silver amalgam restorations of different dimensions. J Adhes Sci Technol 2016; 30:1109-1118.
- Tezvergil A, Lassila LV, Vallittu PK. Composite–composite repair bond strength: effect of different adhesion primers. J Dent 2003; 31:521-525.
- Newman S, Dressler KB, Gsrenadier MR. Direct bonding of orthodontic brackets to esthetic restorative materials using a silane. Am J Orthod 1984; 86:503–506.
- Zachrisson YØ, Zachrisson BU, Büyükyilmaz T. Surface preparation for orthodontic bonding to porcelain. Am J Orthod Dentofacial Orthop 1996; 109:420-430.
- Grewal Bach GK, Torrealba Y, Lagravère MO. Orthodontic bonding to porcelain: a systematic review. Angle Orthod 2014; 84:555-560.
- Gange, P. The evolution of bonding in orthodontics. Am J Orthod Dentofacial Orthop 2015; 147:S56–S63.
- Ju GY, Oh S, Lim BS, et al. Effect of simplified bonding on shear bond strength between ceramic brackets and dental zirconia. Mater 2019; 12:1640.
- Alzainal AH, Majud AS, Al-Ani AM, et al. Orthodontic Bonding: Review of the Literature. Int J Dent 2020; 2020.
- Ibrahim AI, Al-Hasani NR, Thompson VP, et al. Resistance of bonded premolars to four artificial ageing models post enamel conditioning with a novel calcium-phosphate paste. J Clin Exp Dent 2020; 12:e317.
- Della Bona A, Van Noort R. Shear vs. tensile bond strength of resin composite bonded to ceramic. J Dent Res 1995; 74:1591-1596.`
- Rasmussen ST. Analysis of dental shear bond strength tests, shear or tensile? Int J Adhes Adhes 1996; 16:147–154.
- Klocke A, Kahl-Nieke B. Effect of debonding force direction on orthodontic shear bond strength. Am J Orthod Dentofacial Orthop 2006; 129:261-265.
- Skilton JW, Tyas MJ, Woods MG. Effects of surface treatment on orthodontic bonding to amalgam. Aust Orthod J 2006; 22:59-66.
- Bishara SE, Soliman M, Laffoon J, Warren JJ. Effect of changing a test parameter on the shear bond strength of orthodontic brackets. Angle Orthod 2005; 75:832-835.`
- Germec D, Cakan U, Ozdemir FI, et al. Shear bond strength of brackets bonded to amalgam with different intermediate resins and adhesives. Eur J Orthod 2009; 31:207-212.
- Major PW, Koehler JR, Manning KE. 24-hour shear bond strength of metal orthodontic brackets bonded to porcelain using various adhesion promoters. Am J Orthod Dentofacial Orthop 1995; 108:322-329.
- Elekdag-Turk S, Turk T, Isci D, et al. Thermocycling effects on shear bond strength of a self-etching primer. Angle Orthod 2008; 78:351-356.`
- Viwattanatipa N, Prasertsangwal J, Juntavee N. Weibull analysis of shear/peel bond strength of orthodontic buccal tubes bonded to five resin composites. Orthod Waves 2008; 67:120-127.
- Bourke BM, Rock WP. Factors affecting the shear bond strength of orthodontic brackets to porcelain. Br J Orthod 1999; 26:285-290.
Author Info
Mohammed Razzaq Hussein*, Mehdi Abdulhadi Mehdi and Abeer Basim Mahmood
Department of orthodontics, College of Dentistry, IraqCitation: Mohammed Razzaq Hussein, Mehdi Abdulhadi Mehdi, Abeer Basim Mahmood,Effect of Different Bonding Systems on Shear Bond Strength of Buccal Tubes Bonded to Various Restorative Materials: An In Vitro Study, J Res Med Dent Sci, 2021, 9(7): 133-139
Received: 05-Jun-2021 Accepted: 08-Jul-2021