Research - (2021) Volume 9, Issue 7
Effect of Different Restoration Designs on Fracture Strength of Endodontically Treated Teeth Weakened with MOD Cavities
Alaa H Abbas* and Zainab M Abdulameer
*Correspondence: Alaa H Abbas, Department of Conservative, College Of Dentistry, University of Baghdad, Iraq, Email:
Abstract
Purpose: The aim of this in vitro study was to evaluate the effect of different restoration designs on fracture strength and failure mode of endodontically treated upper first premolar with mesio-occluso-distal (MOD) cavity. Material and methods: Forty sound maxillary first premolars were divided into 5 groups (n=8): GA (intact group), GB-E (test groups). In tested groups, all the teeth were received MOD cavities and endodontically treated. GB: Endodontically treated teeth (ETT) restored with direct composite resins (Filtek™ Bulk Fill Posterior Restorative, 3M ESPE). While teeth in groups (C, D and E) were prepared to receive indirect ceramic restorations made from lithium disilicate material (IPS E-max CAD, Ivoclar-Vivadent). GC: ETT restored with overlays. GD: ETT restored with conventional crowns. GE: ETT restored with endocrowns. The indirect restorations were made by CAD/CAM system and adhesively cemented with dual-cure resin cement (RelyX™ Ultimate, 3M ESPE). Samples were mounted in a universal testing machine (LARYEE Universal testing machine, China). At a crosshead speed of 0.5 mm/min, each sample was loaded to failure. Failure modes were also observed. At P0.05, one-way analysis of variance (ANOVA) and Tukey's post hoc significance difference tests were used to analyze the data. Results: The results of this in vitro study revealed that the highest mean of fracture strength was recorded by GD (2013.750 N) followed by GC (1350 N), GE (1079.350 N), GA (1058.125 N) and GB (872.750 N) respectively. Tukey’s post-hoc test showed significant (p<0.05) differences among the different groups. Conclusions: Conventional crowns had the highest fracture strength, while direct composite had the lowest fracture strength. The most favourable combination of strength and failure mode could be observed in groups conventional crowns and overlays so that this restorations can be considered a clinically reliable restorative approach for ETT with MOD cavities.
Keywords
Endocrown, Lithium disilicate, Full crown, Overlay, CAD/CAM, ETT, Fracture resistance
Introduction
The best ways for restoring teeth after root canal treatment continue to remain a controversial matter to these days. When compared to vital teeth, endodontically treated teeth (ETT) have different biomechanical properties. The loss of hard tissues, fracture propagation, extension of the carious lesion, and final prepared cavity in addition to access cavity before endodontic therapy are all common causes of changes in the biomechanical properties and structural integrity of the tooth [1,2]. The ideal technique for restoring ETT is still a controversy, because those teeth are counted to have a higher risk of fracture than the vital teeth [3]. From a biomimetic viewpoint, the conservation and preservation of teeth structures are fundamental in maintaining the balances between mechanical, biological, adhesive, functional and esthetic parameters. preservation of coronal tissues and avoiding invasive endodontic procedure are beneficial, because these ways ensure the biomechanical balance and the long-term performance of restored tooth [4,5].
Endodontic access cavity in combination with MOD cavity preparation dramatically increasing cusps deflection and teeth fragility [6]. Clinical studies show that ETT with perfect coronal rehabilitations are necessary for long-term clinical success. The majority of ETT are missing because of failed coronal restorations in long term. Ideal dental restorations preserve the root canal system, support the residual tooth structure, and restore tooth function [7,8]. In the last few years, restorative approaches to ETT have developed. The availability of reliable and proven adhesive techniques have widened the restoration options for the clinicians. Restoration of ETT with adhesive technique may preserve more tooth structure and provide adequate fracture strength [6]. However, the direct restorations of tooth with resin composites reduces excessive loss of healthy tooth structure and overpreparation, but direct dental composite restorations of extensive cavity cannot build tooth strength and many studies give a median longevity of direct posterior composite restorations [9,10]. Despite clear results on the short-term for MOD restorations without cuspal coverage, overlays and full coverage crown restorations are still the recommended treatment options for restoration of posterior ETT since they present with higher success rate on the long term. These advantages in term of clinical performance still present with some drawbacks as the process still often requires removal of healthy dental tissues [11].
Furthermore, restoration techniques with post free-andcore build-ups are growing in popularity due to their minimal invasiveness and simplification of clinical procedures [12]. However, several clinical and in vitro studies have shown that applying post helps to keep the restorations in place, but it may weaken the root [2]. Endo crowns have been introduced as alternative post less approaches for the restoration of ETT, depending on the availability of remaining tooth structure. The advantages of end crown are conserving of intracanal tissues that are often removed during post placement [11]. As a result, the aim of this study was to assess and compare the effects of various restoration designs on fracture resistance and failure mode in endodontically treated premolars with MOD cavity.
Methods
Samples selection
Forty sound human upper first premolars with two roots and two canals were utilized. Teeth with caries, cracks and abnormal occlusal anatomy were excluded from the study. Digital calipers were used to calculate the buccolingual, mesiodistal, and occlusogingival tooth dimensions, and teeth of comparable size were chosen. The collected teeth were cleaned from debris with hand scalers and then polished with a rubber cup and pumice [13]. The teeth were immersed in a % thymol solution at room temperature for 24 hours [14]. After that, the teeth were held at room temperature in deionized distilled water until the experiment.
Samples grouping
The teeth were divided into five groups, each with 8 teeth:
- Group A: Intact teeth (control).
- Group B: ETT restored with direct composite resin.
- Group C: ETT restored with lithium disilicate overlays.
- Group D: ETT restored with lithium disilicate conventional crowns.
- Group E: EET restored with lithium disilicate end crowns.
Mold construction
To simplify handling of the sample during MOD cavity preparation and root canal treatment, each tooth was embedded in silicone rubber base impression material (putty consistency) that placed inside a mold. A mold was made from transparent acrylic that consisted of a cylindrical shape hole of 10 mm radius and 15 mm depth. The root was wrapped in a saline-socked surgical gauze to keep the tooth hydrated during root canal treatment as shown in Figure 1A.
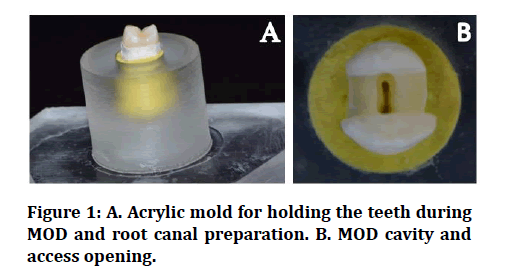
Figure 1: A. Acrylic mold for holding the teeth during MOD and root canal preparation. B. MOD cavity and access opening.
MOD cavity preparation
The teeth in the test groups (B-E) obtained standardized class II MOD cavities with a gingival cavosurface margin 2.0 mm above the cementoenamel junction (CEJ). Each cavity's buccolingual width was one-half of the buccolingual distance, as measured with a digital caliper. The cavities were 4.0 mm deep, without proximal step and a flat floor. all internal line angle were rounded, the cavity's facial and palatal walls were prepared parallel to one another. as shown in Figure 1B.
Root canal treatment
A diamond round bur (Komet, Germany) was employed with a high-speed handpiece under copious airwater cooling to eliminate the roof of the pulp chamber. Size 10 K files (Dentsply, Germany) were placed into a canal after the pulp was removed till their tip could be seen at the apical foramen. By subtracting 1 mm from this length, the working length was calculated. NiTi rotary instruments were used for the endodontic procedure (ProTaper next; Dentsply Maillefer). The canals were enlarged using a crown-down technique with EDTA (MD-CHelCream, META®BIOMED, Korea) as a lubricant until master apical file X2. During endodontic procedures, 5.25 % NaOCl was used to irrigate the canal. All canals were obturated with ProTaper next X2 gutta percha with sealer (Gutta Flow® 2, Coltene) and dried with paper points. Extra guttapercha was eliminated with a heated tool, and the coronal portion was compacted vertically with a plunger.
Direct restoration) core build-up)
Before the MOD cavity preparation of groups B, C, and D, flowable composite was used for taking the impressions for the occlusal surfaces (stamp technique). This technique was used to restore the tooth with composite restoration to the original anatomy. The prepared MOD cavities were etched with 37% phosphoric acid (N- etch, ivoclar ) for 20 sec., then rinsed with water and dried with moisture free air. Two thin coats of a universal bond (Single bond universal, 3M ESPE) were applied on tooth structure then gently air jet for 5 sec. and curing for 20 sec. Super Mat® Adapt® Super Cap® Matrix system (Kerr Hawe SA, Switzerland) was adapted on tooth structure then continued with the administration of composite resin (filtekTM one bulk fill restorative) in two layers at room temperature. Afterward, the Teflon was wrapped on composite layer then the stamp of the tooth was pressed gently on the Teflon to make the restoration take the same shape of the original tooth anatomy. The stamp was displaced to remove the excess material by dental probe, and then the teeth were cured occlusally, mesially and distally for 20 sec. for each surface with a light curing unit (curing pen, Eighteeth, China) (Light intensity: >1000 mW/cm2).
Teeth preparation for indirect restoration
Before starting the preparation step for indirect restorations, using a cubic rubber mold, the roots of teeth were inserted parallel to the long axis of the teeth in selfcuring acrylic resin up to 2 mm below the CEJ.
Uniform teeth preparations were performed for all teeth in group C (overlays) which included: planar occlusal reduction of about 2 mm with butt joint type. The proximal preparation was represented by slot design which had a rounded shoulder of about 1.2 mm depth, with buccolingual width was 1/2 of the buccal-lingual distance, and gingival floor was located 1 mm above the CEJ as shown in Figure 2A. For group D (conventional crowns), uniform teeth preparations were performed which included: axial reduction of about 1.5mm, deep chamfer finish line of 1.0 mm depth, planar occlusal reduction with 5 mm occlusogingival height, and a total convergence angle of 6º as shown in Figure 2B. While the preparation for group E (endocrowns) was included: decapitation of teeth crowns 2 mm above CEJ, The pulp chambers were prepared to eradicate undercut with a 8o occlusal divergence and oval shape with a 4 mm depth from the cavosurface margin with smooth and rounded internal line angle as shown in Figure 2C. A thin layer of flowable composite resins (Filtek Z350, 3M ESPE) was applied to seal the canals entrance and to uniform depth of pulp chamber at 4 mm.

Figure 2: Teeth after preparation for indirect restorations: A. Overlay, B. Conventional crown. C. Endo crown.
Indirect restorations fabrication by CAD/CAM
Scanning and designing
The prepared teeth for indirect restorations were scanned using digital intraoral scanner (Medit I500), the resulting 3D virtual image for the scanned teeth was saved as STL file format. The restorations were designed with the inLab CAD Software (Dentsply Sirona, Germany). To standardize restoration design for all teeth, the The design mode “Biogeneric Reference” was chosen, with intact upper first premolar dentoform tooth serving as a reference tooth for measuring the restoration suggestions. The manufacturer-specified restoration parameters were chosen except the spacer which was reduced to 100 μm instead of the preset 120 μm according to a pilot study.
Milling process
Data were sent to the inLab MC XL milling unit, a 4-axis milling unit (Dentsply Sirona, Germany). In this step, the type and the size of the CAD/CAM block (IPS e.max CAD blocks shade LT A2/C14) was selected and the position of the restorations inside the block was determined. Crystallization and glaze firing: This process was carried out for all restorations by using (EP programat 3010, Ivoclar Vivadent). The crystallization process increases the strength and attained final color of the restorations then glaze firing is conducted by using IPS Ivocolor® glaze Paste fluo (Ivoclar vivadent, Liechtenstein) as shown in Figure 3.
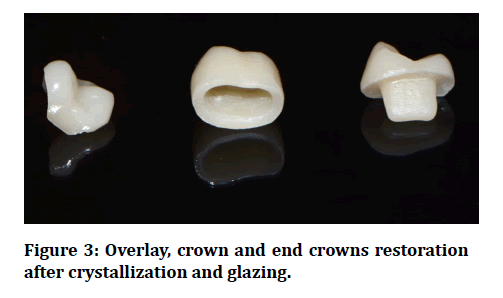
Figure 3: Overlay, crown and end crowns restoration after crystallization and glazing.
Cementation
Surface treatment of indirect restorations: the internal surface of each restoration was processed according to the IPS e.max CAD block manufacturer's instructions. Etching with a 5 % hydrofluoric acid gel (IPS® Ceramic Etching Gel, ivoclar vivadent) was applied for 20 seconds as directed by the manufacturer, then rinsed with copious amounts of water and air dried using a three-way syringe. On the restoration surface, two coats of universal bond (3M ESPE, USA) were applied separately eliminating the need for a separate silane agent when used RelyXTM Ultimate system then rubbing for 20 sec. then the restoration surface is gently air dried for 5 sec. until the solvent has completely evaporated.
Surface treatment of the prepared teeth: Prepared tooth surface was etched with 37% phosphoric acid–etching gel (N-etch, ivoclar vivadent) for 15 sec., rinsed for 15 sec. and dried with air for another 5 sec. A micro-brush was used to apply two coats of universal bond (3M ESPE) to the prepared tooth. Excess solvent was air dried for 5 sec., then light activated for 10 sec.
The dual cure resin cement RelyXTM Ultimate ClickerTM (RelyX™ Ultimate, 3M ESPE, Germany) was used for cementation of restoration to tooth. With finger pressure, each restoration was put on its corresponding tooth, and excess cements were removed with a micro brush. 5 kg constant load was applied with the long axis of each restoration for 5 min. by a customized loading device to keep the restorations from reverting during the cementation. After that, each surface was illuminated by light for 20 sec. then the specimens were stored at 37˚ in distilled water for 24 hrs.
Fracture resistance test
Using a universal testing machine (LARYEE Universal testing machine, China) with a load cell of 5 KN, a single static compressive load was applied with the long axis of the sample, and data was collected using computer software. A compressive load was applied occlusally with a metallic rod with a round tip 4 mm diameter moving at a crosshead speed of 0.5 mm/min during the fracture test. Laboratory made rubber sheet 1 mm thickness to act as a stress breaker and avoid damage from the direct contact of the load applicator with the tested restorations. The loads required to fracture were recorded in Newton. Following the fracture strength test, fracture modes of all samples were examined visually by using dental loupes. The samples were examined for determining different fracture modes whether favourable (restorable) or unfavorable (non-restorable), If the teeth fractured below the CEJ, including vertical root fracture, the failures were called unfavorable. Favorable fracture, on the other hand, was described as restorable failure above the CEJ (Figure 4).
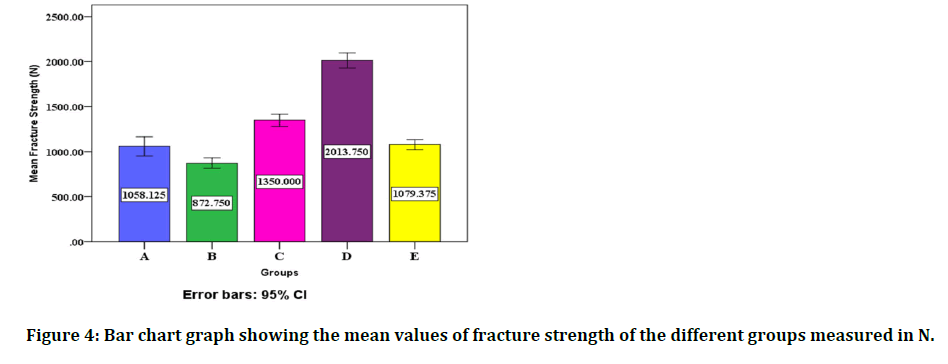
Figure 4: Bar chart graph showing the mean values of fracture strength of the different groups measured in N.
Results
According to the Shapiro-Wilk tests, the data had normal distributions. One-way ANOVA showed statistically significant differences (p>0.05) among all groups. HSD post hoc TuKey test showed that there were statistically significant differences in fracture strength between each two groups when compared together (p<0.05), except when compared group A with group E that there was a statistically non- significant difference (p<0.05) as shown in Figure (4).
The highest mean value of Fracture resistance was found in group D (2013.750 ± 100.915) followed by group C (1350 ± 82.202), the lowest value of Fracture resistance was found in group B (872.750 ± 68.174) as illustrated in Table 1.
Table 1: Descriptive statistics of fracture resistance of the different groups measured in N.
| Groups | N | Mean | ±SD | Minimum | Maximum |
|---|---|---|---|---|---|
| A | 8 | 1058.125 | 128.117 | 930 | 1280 |
| B | 8 | 872.75 | 68.174 | 785 | 1007 |
| C | 8 | 1350 | 82.202 | 1290 | 1545 |
| D | 8 | 2013.75 | 100.915 | 1880 | 2135 |
| E | 8 | 1079.375 | 66.248 | 1005 | 1215 |
Fracture mode
The sound teeth were mostly fractured with restorable patterns (75% restorable); on the other hand, the teeth in the endo crowns group were mostly fractured with non-restorable pattern (12.5% restorable). Teeth in conventional crowns group were recorded 37.5% restorable fracture, while groups overlays, and direct composite were recorded 25% restorable fracture as illustrated in Table 2.
Table 2: Fracture mode of different groups.
| Groups | Restorable fracture | Non- restorable fracture | ||
|---|---|---|---|---|
| No. | % | No. | % | |
| A | 6 | 75 | 2 | 25 |
| B | 2 | 25 | 6 | 75 |
| C | 2 | 25 | 6 | 75 |
| D | 3 | 37.5 | 5 | 62.5 |
| E | 1 | 12.5 | 7 | 87.5 |
Discussion
Depending on age and facial morphology, the physiological maximum occlusal force will range from 100 to 500 N. [15]. According to the findings of several studies, the usual biting force in the premolar region ranged from 222 to 445 N (average 322.5 N) [14,15]. The mean fracture loads for the various tested groups are higher than the mean of maximum biting forces in this study. As a result, all the measured samples should be able to withstand the masticatory forces.
According to the statistical analysis of the result, the null hypothesis was rejected because there were significant differences among the five groups in terms of fracture resistance of the different types of restorations. The statistically significant differences in fracture strength between the groups could be due, in general, to the amount of coronal tooth structure retained and preparation designs, as well as differences in mechanical properties and chemical composition of restoration materials.
The results of this study revealed that Group D conventional crown had the highest mean value of fracture resistance, followed by Group C overlay, Group E endo crown, Group A intact teeth, and Group B direct composite had the lowest mean value of fracture resistance. The higher fracture resistance of conventional crowns (Group D) than other Groups may be related to bracing mechanism of the crown around the cervical tooth structure. The greater the height of remaining tooth structure above the margin of the preparation) ferrule) the better fracture resistance provided [16]. Also, Crown coverage has also been shown to result in an even greater distribution of forces, which is more similar to the clinical conditions [17].
On the other hand, some articles suggest that because of their mechanical properties, all ceramic crowns can also strengthen the tooth structure [18]. In comparison with direct composite restorations (Group B), lithium disilicate conventional crowns have higher fracture toughness and Flexural strength than resin composite and this may be explained the high difference in fracture strength of two groups. Furthermore, teeth with crown rehabilitation had a six-fold higher success rate than teeth that were directly restored, according to research [19].
In comparison with endo crowns, conventional crowns registered higher fracture strength, this is probably due to the smaller surface area of premolar for bonding and the higher crown height, which compromises the endo crown's mechanical properties. On other hands, according to preparation designs of this study, conventional crown preserved more tooth structure than endo crown. The existence of a ferrule effect [20], which distributes the stresses of an endodontically treated tooth. This result agrees with who found that the conventional crown with ferrule recorded statistically significant highest mean value than endo crown group.
The result of this study shows disagreement with [20] who found that the group of endo crown recorded higher fracture strength than group of fibre post and conventional crown in upper premolars. This disagreement may be related to the effect of fibre post insertion and it’s weakening effect on root canal dentin [20].
For overlays (group C), the result showed higher fracture strength following conventional crowns, this positive outcome may be related to several factors, including differences in design of restoration techniques and elastic moduli of restorative materials. The overlay design preserves sounder tooth structure that the increase in the surface area of adhesive bonding of ceramic restorations which improve stress distribution of occlusal forces and enhance fracture resistance [21,22]. This explained high fracture resistance of overlays over endo crowns group. Adhesive cusp coverage restorations improved the fracture resistance of endodontically treated premolars with MOD cavities to a degree comparable to that of intact teeth, according to Kalay, Yildirim [6,23]. The present study confirmed these results, finding that cusp reduction increased fracture resistance. The fracture resistances and fracture patterns were influenced by the cusp reduction designs and thicknesses. The teeth that were preserved with anatomic cusp reduction designs had a higher fracture resistance.
The results of this study revealed that there is no significant difference between endo crowns (Group E) and intact teeth (Group A), These findings are clinically relevant because it show that endocrowns may restore severely destructive endodontically treated premolars to point similar to intact teeth, at least in terms of posterior tooth fracture resistance. The positive results of butt joint endocrown may be related to an even, wide, stable surface of the tooth structure that resists the compressive stresses, because it is prepared parallel to the occlusal plane to ensure stress resistance along the main axis of the tooth, also even thickness of ceramic used in the restoration [24]. In addition, endo crowns comprising both the crown and core as a single unit, was suggested to provide a monoblock effect [25]. This finding is consistent with previous studies who confirmed that endocrowns have been shown to be a successful approach to restoring severely damaged molars and premolars, even in the presence of significant coronal tissue loss or an occlusal risk factor, such as bruxism. This research was a 10-year retrospective study of recorded endocrown cases.
The worst effects of direct inlay restorations (group B) are due to a geometric method of preparation that exerts a wedging force on the tooth, causing it to break under occlual stress. Overlay and complete coverage, on the other hand, direct force along the long axis by overlaying the cusp tips and a portion of the buccal and lingual surface, thus opposing the wedging action caused by the restoration's internal design [26,27]. Also, least fracture strength of direct composite restoration may be related to low flexure strength and fracture toughness of resin composite, and the effect of polymerization shrinkage on cuspal deflection and formation of microcracks in the tooth structure [28-30].
Regarding fracture mode, this study has been found that sound teeth group had the most favourable mode of fracture followed by conventional crowns after that overlays and direct composite groups had the same fracture mode while endocrowns had the most unfavourable one. This may be explained by the fact that the modulus of elasticity of core build up material in groups B, C & D that is in a proximity to that of dentin so more stress distribution at core dentin interface, also full and partial coverage restorations have been associated with better distribution of loads along the root [10,12]. While the mismatching in modulus of elasticity between ceramic material and dentin lead to stress concentration at pulpal floor and this explained the high catastrophic failure in endocrowns group. Another explanation the thickness of endocrown is more than that of other restorations result in fracture of tooth structure rather than restorations in endocrowns group.
Conclusion
The following conclusions may be drawn within the limitations of this research:
- Conventional crowns and overlays restorations increased the fracture resistances of endodontically treated premolars with MOD cavity to a level higher than that of intact teeth.
- The most favorable combination of strength and failure mode could be observed in groups conventional crowns and overlays so that these restorations can be considered a conservative and clinically reliable restorative approach for endodontically treated maxillary premolars with MOD cavities
- No difference in fracture resistance between endocrowns and intact teeth, so that endocrowns can consider a clinically feasible restorative approach for restoring severely damaged endodontically treated premolars.
- The findings of this study suggest that endodontically treated premolars with MOD cavities should not be restored with direct composite.
References
- Dietschi D, Duc O, Krejci I, et al. Biomechanical considerations for the restoration of endodontically treated teeth: A systematic review of the literature, Part II (Evaluation of fatigue behavior, interfaces, and in vivo studies). Quintessence Int 2008; 39.
- Carvalho MAD, Lazari PC, Gresnigt M, et al. Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Brazilian Oral Res 2018; 32.
- Magne P, Carvalho A, Bruzi G, et al. Influence of no-ferrule and no-post buildup design on the fatigue resistance of endodontically treated molars restored with resin nanoceramic CAD/CAM crowns. Operative Dent 2014; 39:595-602.
- Magne P, Lazari P, Carvalho M, et al. Ferrule-effect dominates over use of a fiber post when restoring endodontically treated incisors: an in vitro study. Operative Dent 2017; 42:396-406.
- Lazari PC, de Carvalho MA, Cury AADB, et al. Survival of extensively damaged endodontically treated incisors restored with different types of posts-and-core foundation restoration material. J Prosthetic Dent 2018; 119:769-76.
- Kalay TS, Yildirim T, Ulker M. Effects of different cusp coverage restorations on the fracture resistance of endodontically treated maxillary premolars. J Prosthet Dent 2016; 116:404-10.
- Ree M, Schwartz RS. The endo-restorative interface: current concepts. Dent Clin 2010; 54:345-74.
- Gillen BM, Looney SW, Gu L-S, et al. Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: A systematic review and meta-analysis. J Endodont 2011; 37:895-902.
- Rho Y, Namgung C, Jin B, et al. Longevity of direct restorations in stress-bearing posterior cavities: A retrospective study. Operative Dent 2013; 38:572-82.
- Shu X, Mai QQ, Blatz M, et al. Direct and indirect restorations for endodontically treated teeth: A systematic review and meta-analysis, IAAD 2017 consensus conference paper. J Adhes Dent 2018; 20:183-94.
- Daher R. Optimizing the restoration of posterior endodontically treated teeth: Universiteit van Amsterdam 2019.
- Magne P, Goldberg J, Edelhoff D, et al. Composite resin core buildups with and without post for the restoration of endodontically treated molars without ferrule. Operative Dent 2016; 41:64-75.
- Forster A, Braunitzer G, Tóth M, et al. In vitro fracture resistance of adhesively restored molar teeth with different MOD cavity dimensions. J Prosthodont 2019; 28:e325-e31.
- Lin CL, Chang YH, Pai CA. Evaluation of failure risks in ceramic restorations for endodontically treated premolar with MOD preparation. Dent Materials 2011; 27:431-8.
- Röhrle O, Saini H, Ackland DC. Occlusal loading during biting from an experimental and simulation point of view. Dent Materials 2018; 34:58-68.
- Jotkowitz A, Samet N. Rethinking ferrule–a new approach to an old dilemma. Br Dent J 2010; 209:25-33.
- Beck N, Graef F, Wichmann M, et al. In vitro fracture resistance of copy-milled zirconia ceramic posts. J Prosthet Dent 2010; 103:40-4.
- Habibzadeh S, Rajati HR, Hajmiragha H, et al. Fracture resistances of zirconia, cast Ni-Cr, and fiber-glass composite posts under all-ceramic crowns in endodontically treated premolars. J Adv Prosthodont 2017; 9:170.
- Aquilino SA, Caplan DJ. Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent 2002; 87:256-63.
- Zogheib LV, Saavedra GdSFA, Cardoso PE, et al. Resistance to compression of weakened roots subjected to different root reconstruction protocols. J Applied Oral Sci 2011; 19:648-54.
- Dere M, Özcan M, Göhring TN. Marginal quality and fracture strength of root-canal treated mandibular molars with overlay restorations after thermocycling and mechanical loading. J Adhesive Dent 2010; 12:287.
- Rocca GT, Krejci I. Crown and post-free adhesive restorations for endodontically treated posterior teeth: From direct composite to endocrowns. Eur J Esthet Dent 2013; 8:156-79.
- Mondelli RFL, Ishikiriama SK, Oliveira Filho Od, et al. Fracture resistance of weakened teeth restored with condensable resin with and without cusp coverage. J Applied Oral Sci 2009; 17:161-5.
- Rocca GT, Daher R, Saratti CM, et al. Restoration of severely damaged endodontically treated premolars: The influence of the endo-core length on marginal integrity and fatigue resistance of lithium disilicate CAD-CAM ceramic endocrowns. J Dent 2018; 68:41-50.
- Zogheib LV, Pereira JR, Valle ALD, et al. Fracture resistance of weakened roots restored with composite resin and glass fiber post. Br Dent J 2008; 19:329-33.
- Magne P, Belser UC. Porcelain versus composite inlays/onlays: effects of mechanical loads on stress distribution, adhesion, and crown flexure. Int J Periodont Restorative Dent 2003; 23.
- https://scientonline.org/open-access/effect-of-full-coverage-endocrowns-onlays-inlays-restorations-on-fracture-resistance-of-endodontically-treated-molars.pdf
- Eapen AM, Amirtharaj LV, Sanjeev K, et al. Fracture resistance of endodontically treated teeth restored with 2 different fiber-reinforced composite and 2 conventional composite resin core buildup materials: An in vitro study. J Endodont 2017; 43:1499-504.
- Cobankara FK, Unlu N, Cetin AR, et al. The effect of different restoration techniques on the fracture resistance of endodontically-treated molars. Operative Dent 2008; 33:526-33.
- De Kuijper M, Gresnigt M, Van Den Houten M, et al. Fracture strength of various types of large direct composite and indirect glass ceramic restorations. Operative Dent 2019; 44:433-42.
Author Info
Alaa H Abbas* and Zainab M Abdulameer
Department of Conservative, College Of Dentistry, University of Baghdad, Baghdad, IraqCitation: Alaa H Abbas, Zainab M Abdulameer,Effect of Different Restoration Designs on Fracture Strength of Endodontically Treated Teeth Weakened with MOD Cavities, J Res Med Dent Sci, 2021, 9(7): 190-196
Received: 16-May-2021 Accepted: 12-Jul-2021
