Research - (2020) Volume 8, Issue 5
Effectiveness of Different Agents for Disinfection of Gutta Percha Cones an in vitro study
Madhuri Agrawal1*, Ganesh Kotalwar2, Akshay Gelda1, Safalya Kadtane3, Abhishek Badade1 and Vivek Hegde4
*Correspondence: Madhuri Agrawal, Department of Conservative Dentistry and Endodontics M.I.D.S.R. Dental College and Hospital, India, Email:
Abstract
Aim: The aim of the present study was to evaluate and compare the 1) sterilizing effect of different disinfecting solutions on gutta-percha cones: 5.25% sodium hypochlorite, 2% chlorhexidine gluconate, propolis and ozonated water.2) to find out the minimum time required to effectively disinfect gutta -percha cones.
Method: Fifty size 30 gutta-percha cones were used in this study. 40 cones were randomly divided into 4 groups of 10 samples each.5 cones served as positive control & 5 cones served as negative control. The cones were contaminated by immersion in saliva and then were disinfected by immersing in the above mentioned four disinfecting solutions: 5.25% sodium hypochlorite (G1), 2% chlorhexidine gluconate (G2), propolis (G3) and ozonated water (G4) for periods of 30 seconds and 60 seconds. After the disinfection procedure, the cones were incubated in brain heart infusion broth for 72hrs and the presence of bacterial growth was analysed by turbidity of the medium. Data was analysed by Fisher’s exact test.
Results: 2% chlorhexidine gluconate(G2) at both times evaluated did not show bacterial growth.5.25% sodium hypochlorite(G1) showed growth after immersion for 30 sec but after 60 sec did not show bacterial growth. Propolis (G3) and Ozonated water (G4) showed diverse results after the immersion for 30 sec and 60 sec.
Conclusion: Immersion of GP cones in 2% chlorhexidine gluconate for 30sec was an effective method for GP disinfection, while 5.25% sodium hypochlorite needed 60 sec of immersion to disinfect the GP. Ozonated water can be used for disinfection of gutta-percha cones. Propolis is less effective for disinfection of gutta percha cones.
Keywords
Gutta-percha, Disinfection, Chlorhexidine gluconate, Sodium hypochlorite, Propolis, Ozone
Introduction
The primary objective in root canal treatment is to maintain asepsis right from the access opening to the permanent coronal restoration of the tooth [1]. Obturation is one of the most important procedures of a root canal treatment which determines its success [2]. Since the introduction of Gutta-percha in endodontics, it has been widely used as a root canal filling material. Gutta-percha cones are made up of rubber and the use of standard high temperature moist or dry heat sterilization deforms guttapercha cones [3]. Hence, a rapid chairside decontamination which does not deform the structure of gutta-percha is needed [4]. Several studies have examined cold sterilizing agents for gutta-percha. One of the earlier reports regarding sterilization of gutta-percha cones recommended exposing the cones to paraformaldehyde vapor for 3 hours [5]. Such methods may be satisfactory for long-term storage of gutta-percha cones, but it is not suitable for rapid decontamination of gutta-percha during treatment [6]. The appropriate disinfectant should be the one that can be used routinely in dental clinics providing a fast disinfection without modifying the structure of the cone and biocompatible with the tissues surrounding it.
The purpose of the present study is to find out a rapid, convenient and effective method of disinfecting guttapercha using 5.25% NaOCl, 2% chlorhexidine gluconate (CHX), propolis and ozonated water contaminated by saliva after immersing for a period of 30 seconds and 60 seconds.
Materials and Methods
In the present study, fifty size 30 standardized GP cones from the same batch (Sure endo,korea) were used. The packages remained closed until the tests. 15 ml of human unstimulated whole saliva was collected just prior to performing the test. Then the samples were divided randomly into four groups of 10 samples each (n=10). Control groups (positive and negative) consisted of 5 samples each (n=5). Cones were contaminated with saliva. No attempt was made to remove excess saliva from the points. To confirm that all the samples were contaminated, GP cones were inserted individually into test tubes containing 5 ml of sterile BHI broth and were then incubated at 37°C for 72h. Bacterial growth was evaluated by the presence of turbidity in the broth. Then the samples were divided according to the disinfectant used:
Group 1–5.25% NaOCl.
Group 2–2% CHX.
Group 3–Propolis (7:3).
Group 4–Ozonated water.
Each main group was further sub divided into 2 subgroups A, B according to the immersion time of guttapercha into solution. Subgroup A – Immersion time of Gutta-percha was 30 seconds. Subgroup B –Immersion time of Gutta-percha was 60 seconds. Five GP cones were immersed for 30 secs in one of the agents and other five were immersed for 60 secs. The same procedure was repeated for all the groups.
The following controls were used.
Positive control: A total of five gutta-percha cones were used as positive control from the same pack. The cones were contaminated with saliva and directly transferred to the broth without disinfection.
Negative control: A total of five gutta-percha cones were taken from freshly sealed pack and placed in the broth without contaminating with saliva.
After the points were dipped in the disinfectant, they were blotted on a sterile gauze piece to remove excess solution and then placed in a culture tube containing sterile BHI broth and incubated at 37°C for 72h.The whole experiment was conducted under aseptic conditions. All testing procedures were performed by a single operator using sterile gloves, mask, and instruments.
Bacterial growth was evaluated by the presence of turbidity in the broth. The presence or absence of turbidity resulted in quantitative data and the results were statistically analyzed by Fisher ’ s exact test. Statistical significance level was established at P <0.05 (Figure 1).
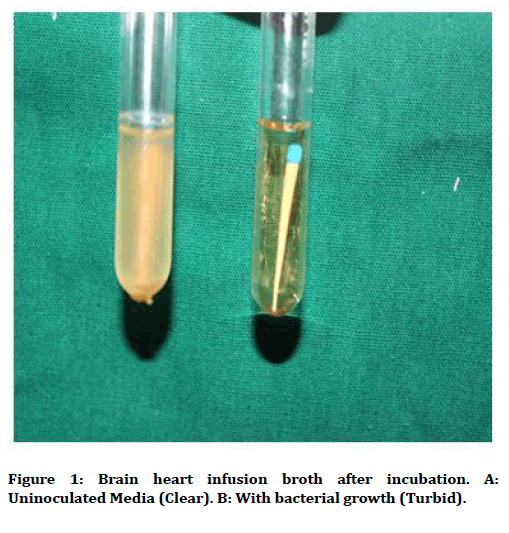
Figure 1. Brain heart infusion broth after incubation. A: Uninoculated Media (Clear). B: With bacterial growth (Turbid).
Results
The comparison between the bactericidal activities of the agents in disinfecting GP cones in this study is shown in Table 1.
| Time(sec) | Sodium hypochlorite -5.25% | Chlorhexidine gluconate (2%) | Propolis | Ozonated water |
|---|---|---|---|---|
| 30(A) | + + + - - | + - - - - | + + + + - | + + + + + |
| 60 (B) | - - - - - | - - - - - | - + + + - | + + - - - |
| Positive control | Negative control | |||
| + + + + + | - - - - - | |||
Table 1: Bacterial growth (turbidity) between samples.
It was observed that the positive control group did not demonstrate any bactericidal action. This resulted in intense turbidity in all samples. The negative control group did not show turbidity in any of the samples. 2% CHX demonstrated absence of the turbidity in the subgroup B; indicating no bacterial growth. 80% of the samples showed no turbidity in subgroup A. The immersion of the cones in 5.25% NaOCl (G1) showed absence of turbidity after 60 sec while 60% samples showed bacterial growth after 30 sec. In G3, 80% cones showed bacterial growth in subgroup A and 60% of the cones showed growth in subgroup B. In G4, all the samples showed bacterial growth in subgroup A and 40% of the samples showed bacterial growth in subgroup B. The Fisher’s exact test revealed significant difference between the groups (P = 0.01).
Gutta-percha (GP) have been the material of choice because of properties such as biocompatibility, dimensional stability, radiopacity and thermoplastic [7]. Despite GP cones being produced under aseptic conditions and sold in sealed packages their sterilization is questionable and they can be easily contaminated when they exposed in clinics as well as during handling [1,8].
In this study, the cones were intentionally contaminated with saliva. Saliva was chosen as a contaminant because of its high bacterial density (10 s bacterial cells/ml) and the fact that it contains several different bacterial species, including E. faecalis and Staphylococcus species [2]. Also, it may be one of the most common ways to contaminate the root canal during treatment.
Sodium hypochlorite 5.25% has been found to be effective in disinfecting GP cones [9]. The antibacterial activity of sodium hypochlorite is mainly due to hypochlorous acid (HClO) in the solution which has an oxidative action on sulfhydryl groups of bacterial enzymes [10]. The results in the present study showed that 5.25% NaOCl can be effective if a 60 secs immersion period is used.
CHX is a positively charged hydrophobic and lipophilic molecule that interacts with phospholipids and lipopolysaccharides on the cell membrane of bacteria and then enters the cell through some type of active or passive transport mechanism [11]. Its efficacy is because of the interaction of the positive charge of the molecule and the negatively charged phosphate groups on microbial cell walls thereby altering the cells’ osmotic equilibrium [12]. This increases the permeability of the cell wall.Chlorhexidine kills vegetative bacteria by disrupting the membrane integrity and inducing the precipitation of the cytoplasm [13].
When GP cones were immersed for 30 secs in CHX, 80% of the samples showed no turbidity after incubating while none of the samples showed bacterial turbidity when immersed for 60 secs. This showed that CHX is effective for disinfecting GP after immersing for a period of 30 secs.
Propolis is a sticky and resinous material gathered by bees from bud scales of plants and trees. The bees take the resin back to their hives and work on it, producing a glue-like substance with which they fill cracks and seal up their hives. It is composed of resin (55%), essential oils and wax (30%) mixed with bee glue “the salivary secretions of bees ” and pollen (5%) and other constituents (10%) which are amino acids, minerals, ethanol (alcohol), vitamins A, complex, E and the highly active bio-chemical substance known as bioflavonoid. In dentistry, propolis has been used for surgical wound repair, direct and indirect pulp capping, reduction of dentin hypersensitivity, and in treatment of infected root canals and periodontitis [14]. Antibacterial characteristic of propolis had been explained in several ways. Kujumgiev, et al. reported that it prevented bacterial cell division and broke down bacterial walls and cytoplasm similar to the action of some antibiotics [15].
Propolis in the present study showed diversified results. Most of the samples showed bacterial turbidity when immersed for 30 and 0 seconds. Hence, further studies are required to evaluate the efficacy of Propolis in disinfecting GP cones.
Ozonated water has been used for treatment of endodontic infections [16,17]. Studies have reported interesting results when ozone-treated water was used in the dental unit [18,19]. The antimicrobial effect of ozone results from oxidation of microbial cellular components. Ozone is a highly reactive form of oxygen that is generated by passing oxygen through high voltage [20]. Ozonated water had nearly the same antimicrobial activity as 5.25% sodium hypochlorite when immersed for 60 sec. Ozone works best when there is fewer organic debris remaining [21]. It is effective when it is used in sufficient concentration, for an adequate time. It will not be effective if too little dose of ozone is delivered or it is not delivered appropriately [22].
In the present study, GP cones when immersed for 30 sec in ozonated water, most of the samples showed bacterial turbidity. When the cones were introduced for 60 seconds,60% of the samples showed no turbidity. This might be due the shorter immersion period. Hence, further research including longer immersion time can is required to evaluate the efficacy of ozonated water.
The limitations of this study include the shorter incubation times used. A longer incubation time may be needed for some species of bacteria, and this cannot be overlooked. Hence, more sensitive tests such as polymerase chain reaction testing are to be carried out before confirming the sterility of gutta percha cones. However, even with the shorter incubation times, the fact that one group turned positive for bacteria strengthen the point for disinfection.
Although there are studies related to the use of ozonated water on oral microorganisms in vitro, no literature exists till date on the comparison of the anti-microbial activity of propolis and ozonated water with sodium hypochlorite and chlorhexidine in endodontic treatment. So, this study could very well be the first research.
Conclusion
Based on statistical analysis, it can be concluded that the immersion of GP cones in a solution of 2% CHX for 30 sec is an efficient method to promote their disinfection. The use of 5.25% NaOCl required 60 sec to provide an effective action. Ozonated water can be used for disinfection of gutta-percha cones. Propolis is less effective for disinfection of gutta percha cones. Also, there was no contamination present in new sealed boxes of gutta-percha cones and gutta-percha cones are usually sterile during storage.
References
- Özalp N, Ökte Z, Özcelika B. The rapid sterilization of gutta-percha cones with sodium hypochlorite and glutaraldehyde. J Endod 2006; 32:1202– 1204.
- Siqueira JR, da Siliva CH, Cerqueira M das D, et al. Effectiveness of four chemical solutions in eliminating Bacillus subtilius spores on gutta-percha cones. Endod Dent Traumatol 1998; 14:124–126.
- Montgomery S. Chemical decontamination of gutta-percha cones with polyvinyl pyrolidone-Iodine. Oral Surg Oral Med Oral Pathol 1971; 31:258–266.
- Senia ES, Macarro RV, Mitchell JL, et al. Rapid sterilization of gutta-percha cones with 5.25% sodium hypochlorite. J Endod 1975; 1:136–140.
- Haapasalo M, Udnæs T, Endal U. Persistent, recurrent and acquired infection of the root canal system posttreatment. Endod Top 2003; 6:29–56.
- Da Motta PG, de Figueiredo CBO, Maltos SMM, et al. Efficacy of chemical sterilization And storage conditions of gutta-percha cones. Int Endod J 2001; 34:435–439.
- Cardoso CL, Kotaka CR, Redmerski R, et al. Rapid decontamination of gutta-percha cones with sodium hypochlorite. J Endod 1999; 25:498 –501.
- Suchde RV, Talim ST, Billimoria KF. Efficiency of cold sterilizing agent for endodontic procedure. J Dent Res 1979; 58:670.
- Gomes BPFA, Ferraz CCR, Vianna ME, et al. In vitro antimicrobial activity of several concentrations of sodium hypochlorite and chlorhexidine gluconate in the elimination of Enterococcus faecalis. Int Endod J 2001; 34:424–428.
- Gomes BPFA, Vianna ME, Matsumoto CU, et al. Disinfection of gutta-percha cone with Chlorhexidine and sodium hypochlorite. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 100:512–517.
- Short RD, Dorn SO, Kuttler S. The crystallization of sodium hypochlorite on gutta-percha cones after the rapid-sterilization technique: An SEM study. J Endod 2003; 29:670–674.
- Athanassiadis B, Abbott PV, Walsh LJ. The use of calcium hydroxide, antibiotics and biocides as antimicrobial medicaments in endodontics. Australian Dent J 2007; 52;S64–S82.
- Jenkins S, Addy M, Wade W. The mechanism of action of chlorhexidine. A study of plaque growth on enamel inserts in vivo. J Clin Periodontol 1988; 15:415-424.
- AL-Qathami, AL-Madi. Comparison of sodium hypochlorite, propolis and saline as root canal irrigants: A pilot study. Saudi Dent J 2003; 15.
- Kujumgiev A, Tsvetkova I, Serkedjieva Y, et al. Antibacterial, antifungal andantiviral activity of propolis of different geographic origin. J Ethnopharmacol 1999; 64:235-240.
- Nagayoshi M, Fukuizumi T, Kitamura C, et al. Efficacy of ozone on survival and permeability of oral microorganisms. Oral M`icrobiol Immunol 2004; 19:240-246.
- Hems RS, Gulabivala K, Ng YL, et al. An in vitro evaluation of the ability of ozone to kill a strain of Enterococcus faecalis. Int Endod J 2005; 38:22-29.
- Lezcano I, Rey RP, Gutierrez MS, et al. Ozone inactivation of Pseudomonas aeruginosa, Escherichia coli, Shigella sonnei and Salmonella typhimurium in water. Ozone Sci Engineering 1999; 21:293–300.
- Filippi A. Water disinfection of dental units using ozone– microbiological results after 11 years and technical problems. Ozone Sci Engineering 2001,24, 479–83.
- Murakami H, Mizuguchi M, Hattori M, et al. Effect of denture cleaner using ozone against methicillin-resistant Staphylococcus aureus and E. coli T1 phage. Dent Materials 2002; 21:53–60.
- Baysan A, The use of ozone in dentistry and medicine. Primary Dent Care 2005; 12:47–52.
- Haapasalo M, Endal U, Zandi H, et al. Eradication of endodontic infection by instrumentation and irrigation solutions. Endod Top 2005; 10:77–102.
Author Info
Madhuri Agrawal1*, Ganesh Kotalwar2, Akshay Gelda1, Safalya Kadtane3, Abhishek Badade1 and Vivek Hegde4
1Department of Conservative Dentistry and Endodontics M.I.D.S.R. Dental College and Hospital, Latur, India2Department of Orthodontics and Dentofacial Orthopaedics, Nanded Rural Dental College and Research Centre, Nanded, India
3Department of Public Health Dentistry, M.I.D.S.R. Dental College and Hospital, Latur, India
4Department of Conservative Dentistry and Endodontics, M.A. Rangoonwala College of Dental Sciences and Research Centre, Pune, India
Received: 27-Jul-2020 Accepted: 24-Aug-2020 Published: 31-Aug-2020
