Research - (2022) Volume 10, Issue 9
Estimating the Levels of GlycA: A Novel Pro Inflammatory Biomarker in Periodontitis Subjects with and without Diabetes Mellitus
Paladugu Devi Navya1*, Kaarthikeyan G1 and Selvi Raj J2
*Correspondence: Paladugu Devi Navya, Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical sciences (SIMATS), Saveetha University, Chennai, India, Email:
Abstract
Background: The NMR biomarker Glycoprotein acetylation [GlycA] is a novel glycoprotein acetylation biomarker. It's an NMR signal that comes from the glycan groups of some acute-phase glycoproteins [most notably -1-acid glycoprotein, haptoglobin, 1-antichymotrypsin, and transferrin]. GlycA has been examined extensively in the context of cardiovascular disease [CVD], where it was discovered to be highly linked to atherosclerosis and the risk of future CVD. Methods: The study enlisted the participation of 30 people. Based on gingival index, probing depth, and clinical attachment level, participants were separated into three groups: the healthy group (group 1; n=10), periodontitis without diabetes group (group 2; n=10), and periodontitis with diabetes mellitus group (group 3; n=10). Gingival crevicular fluid (GCF) samples collected from each subject were quantified for GlycA levels using an enzyme-linked immunosorbent assay. Results: The mean GlycA concentrations in GCF increased as the disease progressed from healthy to gingivitis to periodontitis. GlycA concentration was found to be highest in group 3 and lowest in group 1. GlycA levels also had a beneficial relationship with periodontal markers. Conclusions: In all groups, GCF GlycA concentrations were positively associated. Hence, GCF GlycA values were considered a marker of inflammatory activity in periodontal disease. However, GlycA deserves further consideration as a diagnostic target. To confirm positive associations, more large-scale investigations should be conducted.
Keywords
Chronic periodontitis, Gingival crevicular fluid, Diabetes mellitus
Introduction
Periodontitis is an inflammatory illness of the teeth's supporting tissues caused by individual germs or groups of microorganisms that leads to the progressive deterioration of the periodontal ligament and alveolar bone, culminating in periodontal pocket formation, gingival recession, or both [1]. An increasing risk for periodontitis has been shown with the variations in genes related to the inflammatory response [2].
Diabetes mellitus- it is a progressive metabolic disease and is a great threat to human health. According to the International Diabetes Federation, it has been estimated that 463 million people were suffering from diabetes worldwide in 2019. By 2030 it was predicted that 578 million people will have diabetes and this number will be increased by 51% around 2045 [3]. The major complications of diabetes are diabetic nephropathy, diabetic neuropathy, cardiomyopathy, delayed wound healing, and retinopathy. The sixth complication of diabetes mellitus is periodontitis [4]. The link between periodontitis and diabetes mellitus is a “double edged sword” with uncontrolled diabetes leading to periodontal destruction and loss of teeth. On the other hand, poor periodontal health leads to insulin resistance and diabetes mellitus [5-10].
The pathogenic mechanism between periodontitis and diabetes is the chronic elevation of the proinflammatory mediators like interleukin1 beta, tumour necrosis factoralpha (TNF-α) in serum leading to insulin resistance. On the other hand the chronic elevation of the blood glucose in diabetic subjects leads to the accumulation of advanced glycation end products in periodontal tissues. This can cause periodontal destruction and worsening of the periodontal condition.
Glycans are complex oligosaccharides that are crucial for health and play a role in the development of many inflammatory illnesses. The acetylation of glycoproteins [GlycA] is a brand-new NMR biomarker. The glycosyl groups of a few acute-phase glycoproteins [primarily -1-acid glycoprotein, haptoglobin, -1-antichymotrypsin, and transferrin] produce an NMR signal. GlycA has been examined extensively in the context of cardiovascular disease [CVD], where it was discovered to be highly linked to atherosclerosis and the risk of future CVD. A link between cardiovascular and short-term all-cause mortality has also been discovered in large population research. Based on substantial associations with both CVD and diabetes in large cohorts, GlycA underlines the cumulative risk stemming from various inflammatory pathways in several inflammatory illnesses, including rheumatoid arthritis and psoriasis. Furthermore, GlycA levels were reduced with successful anti-TNF therapy treatment of psoriatic skin inflammation, suggesting that it could be a therapeutically meaningful biomarker for disease severity monitoring. GlycA is currently being investigated as a novel marker of systemic inflammation for the reasons stated above. Periodontitis is a chronic inflammatory disease. As far as our knowledge is concerned, there are no studies yet in the literature evaluating the GlycA expression levels between periodontitis patients with or without diabetes mellitus. Thus the aim of this study was to estimate the levels of GlycA in periodontitis subjects with and without diabetes mellitus and systemically healthy subjects.
Materials and Methods
The study was approved by the institutional ethical committee. This study was conducted in the department of periodontics, Saveetha institute of medical and technical sciences, Saveetha dental college and hospitals. Total of 30 subjects (male=17,female=13) were stratified into three groups, group 1(n=10) patients with stage 2-4 periodontitis (according to the world workshop of periodontics classification, 2017), interdental clinical attachment loss of 3 to > 5mm, radiographic bone loss of coronal third and extending to mid third of root and beyond it, tooth loss due to periodontitis of 5 or more than 5 teeth, probing depth of > 6mm. Group 2 (n=10) - patients with type 2 diabetes mellitus (HbA1c value ranging from 6.8 to 7.5 were included), group 3(n=10) systematically and periodontally healthy subjects. The exclusion criteria were: smokers, type 1 diabetes mellitus, other systemic diseases apart from DM like Cardiovascular diseases, pregnant or lactating women, patients underwent periodontal treatment within the past 6 months, patients under anti-inflammatory drug therapy.
Informed consent obtained from all the subjects. After recording the complete periodontal chart, gentle supragingival scaling was done in the first appointment. Next appointment early in the morning, After proper isolation GCF was collected from deep pocket regions in periodontitis subjects and at the sulcular entrance of the tooth for healthy subjects by inserting the micro capillary tube. The collected GCF from multiple sites of the same patients were pooled together and transferred to sterile Eppendorf tubes by convenient air blast by using a chip blower and immediately stored at -70 degree centigrade until further investigation. Enzyme linked immunosorbent assay (ELISA) was performed after the completion of sample collection.
Assay procedure
Before beginning the test method, get all of the reagents ready. It is suggested that all Standards and Samples be added to the microplate in duplicate. Standardise: Set up standard wells and conduct sample well tests. To the standard well, add 50L of diluted standard. Add Sample: Fill the testing sample well with 40L of sample diluent. Then pour 10L into the testing sample well, leaving the blank well empty. Incubate for 45 minutes at 37 °C, covered with a plate cover. Aspirate and wash each well four times for a total of five washes, about 1-3 minutes each time. Using a squirt bottle, manifold dispenser, or autowasher, fill each well with a Wash buffer (250L). Achieving good performance requires complete liquid elimination at each phase. After Incubate for 30 minutes at 37 degrees Celsius. As in step 5, repeat the aspiration/ wash operation five times. To each well, pour 50 mL of Chromogens solution A and 50 mL of chromogenes solution B. Incubate for 15 minutes at 37°C after gently mixing. Protect yourself from the sun. To each well, pour 50 liters of Stop Solution. The wells' hue should shift from blue to yellow. Gently tap the plate to ensure full mixing if the colour in the wells is green or the colour shift does not appear uniform. Within 15 minutes, use a microtiter plate reader to read the Optical Density (O.D.) at 450 nm.
Statistics
All data collected in the present study was expressed in the form of mean ± standard deviation where statistical significance was assessed using SPSS version 23.0 for windows (SPSS Inc., Chicago, IL). Chi square test was used to assess statistical significance between age, gender and periodontal status with and without diabetes mellitus. One way Anova was used to assess statistical significance between groups.
Results
The results of the present study indicate that mean glycA concentration in GCF was highest in group 3. Descriptive statistics of study groups were given in Table 1. The mean glycA concentrations obtained were mentioned in Table 2. The study population consisted of 30 individuals with an age range of 20-60 years, out of which seventeen were males and thirteen were females. There is no significant difference between the gender and the expression of glycA, shown in Table 2.The p value for one way ANOVA between groups was less than 0.05, indicating that there is a statistical difference in expression within the groups, that is, between healthy, periodontitis or healthy, periodontitis with diabetes mellitus or periodontitis, periodontitis with diabetes mellitus or periodontitis, periodontitis with diabetes mellitus. The mean difference between different groups was shown in Figure 1. One way anova was used to analyse the statistical difference between the three groups. The p value for the statistical tests were given in Table 1.
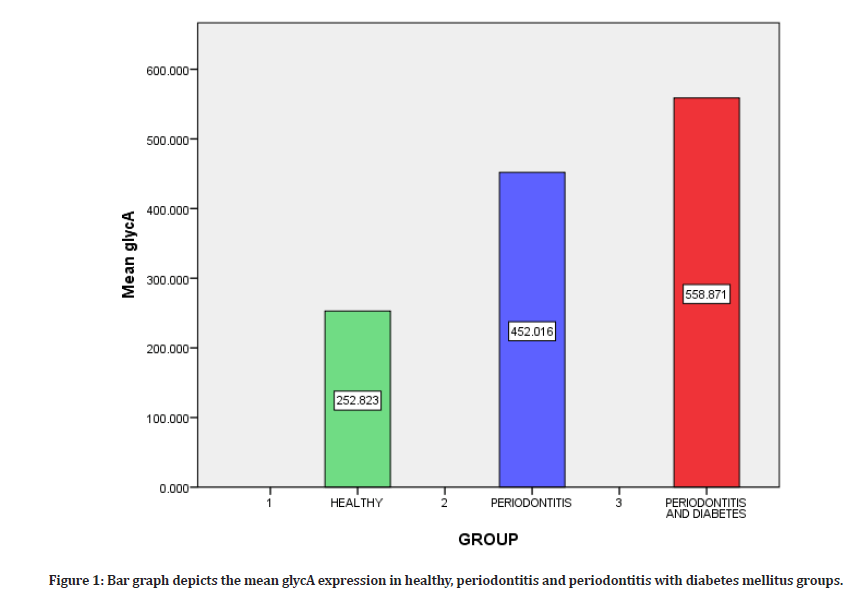
Figure 1: Bar graph depicts the mean glycA expression in healthy, periodontitis and periodontitis with diabetes mellitus groups.
| S. No | Data | Mean | P Value |
|---|---|---|---|
| 1 | Group I | 252.82 | 0 |
| Group II | 452.06 | ||
| 2 | Group III | 452.06 | 0 |
| Group III | 558.87 | ||
| 3 | Group III | 558.87 | 0 |
| Group I | 252.82 | ||
| P value is less than 0.005, significant difference is seen between groups | |||
| Group1=Healthy | |||
| Group2=periodontitis | |||
| Group3=periodontitis with diabetes mellitus | |||
Table 1: Statistical differences between different groups by one way Anova test.
| S.NO | Gender | Groups | Mean | P Value |
|---|---|---|---|---|
| 1 | MALE | I | 211.02 | 0.098 |
| 17 | II | 471.1 | ||
| III | 566.93 | |||
| 2 | FEMALE | I | 315.52 | 0.078 |
| 13 | II | 423.38 | ||
| III | 550.8 | |||
| P value is more than 0.005, there is no statistical difference between gender and expression | ||||
| Group1=Healthy | ||||
| Group2=periodontitis | ||||
| Group3=periodontitis with diabetes mellitus | ||||
Table 2: Statistical difference between different groups and gender. Level comparison between group 1, 2, 3 with gender.
Discussion
Periodontitis is a chronic inflammatory disease, the interaction between host and pathogen activates proinflammatory cascade reactions. This results in secretion of TNF alpha and interleukin 1 beta, which in turn causes connective tissue destruction and bone resorption. These increased pro-inflammatory cytokines induce insulin resistance and decrease insulin action, which in turn causes accumulation of AGE (advanced glycation end products). AGE proteins react with macrophage AGE receptors; this interaction causes the synthesis and secretion of TNF alpha and interleukin 1 beta which leads to increased oxidative stress. Thus increased cascade reactions cause connective tissue degradation, activation of collagenases and MMPs.
In the same way increased insulin resistance leads to degradation of the connective tissue and activation of MMPs, and accumulation of more and more AGE proteins which results in thrombosis and release of more proinflammatory cytokines. Because of accumulation and thrombosis, there is a decreased migration of neutrophils and PMNs, thus causing the microflora to invade more and cause more tissue destruction. Thus periodontitis and diabetes have a two way relationship [11].
GlycA is an NMR signal produced by the glycan groups of acute-phase glycoproteins. It is already proved that glycA is associated with diabetes mellitus [12], rheumatoid arthritis [13] and psoriasis [10]. Periodontitis along with diabetes mellitus cause more inflammation and destruction compared to periodontitis alone. A study conducted by Connelly et al on glycA levels revealed that glycA test can be used for clinical application and also as a diagnostic marker for future risk assessment of type 2 diabetes mellitus [14]. Several studies have shown that there is a positive correlation between expression of glycA and diabetes mellitus [13,14]. A database study conducted on glycA demonstrates that glycA is a biomarker for chronic inflammation, neutrophil activity and risk for future severe infection [15]. Results obtained from the current study shows that glycA is more prominently measured in samples of patients suffering from periodontitis with diabetes mellitus than periodontitis samples than healthy samples in a descending order. P value is 0.000, which shows that there is a statistical difference in the expression of glycA in three groups. Statistically there was no difference between gender and expression of glycA.
Conclusion
GlycA concentrations in GCF rose in periodontitis, according to this study. GlycA levels rose in tandem with the severity of periodontal disease (as measured by clinical criteria). As a result, GlycA in GCF could be used as a possible indicator of inflammatory activity in periodontal disease. This is the only study that we are aware of that estimates and compares GlycA levels in GCF with periodontitis and diabetes mellitus. The larger the amount of periodontal tissue loss in the current investigation, the higher the mean GlycA concentration. GlycA could be used as a biomarker with more research. Future study involving a large sample size is required.
References
- Newman MG, Takei H, Klokkevold PR, et al. Carranza's clinical periodontology. Elsevier Health Sciences 2011.
- Socransky SS, Haffajee AD. Periodontal microbial ecology. Periodontol 2005; 38:135-187.
- Who Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the international diabetes federation diabetes Atlas. Diabetes Res Clin Pract 2019; 157:107843.
- King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: Prevalence, numerical estimates, and projections. Diabetes Care 1998; 21:1414-1431.
- Löe H. Periodontal disease: The sixth complication of diabetes mellitus. Diabetes Care 1993; 16:329-334.
- Preshaw PM, Alba AL, Herrera D, et al. Periodontitis and diabetes: A two-way relationship. Diabetologia 2012; 55:21-31.
- Otvos JD, Shalaurova I, Wolak-Dinsmore J, et al. GlycA: A composite nuclear magnetic resonance biomarker of systemic inflammation. Clin Chem 2015; 61:714-723.
- Ballout RA, Remaley AT. GlycA: A new biomarker for systemic inflammation and cardiovascular disease (CVD) risk assessment. J Laborat Precision Med 2020; 5.
- Bell JD, Brown JC, Nicholson JK, et al. Assignment of resonances for ‘acute-phase glycoproteins in high resolution proton NMR spectra of human blood plasma. FEBS Letters 1987; 215:311-315.
- Joshi AA, Lerman JB, Aberra TM, et al. GlycA is a novel biomarker of inflammation and subclinical cardiovascular disease in psoriasis. Circ Res 2016; 119:1242-1253.
- Grossi SG, Genco RJ. Periodontal disease and diabetes mellitus: A two‐way relationship. Ann Periodontol 1998; 3:51-61.
- Lorenzo C, Festa A, Hanley AJ, et al. Novel protein glycan–derived markers of systemic inflammation and C-Reactive protein in relation to glycemia, insulin resistance, and insulin secretion. Diabetes Care 2017; 40:375-382.
- Ormseth MJ, Chung CP, Oeser AM, et al. Utility of a novel inflammatory marker, GlycA, for assessment of rheumatoid arthritis disease activity and coronary atherosclerosis. Arthritis Res Ther 2015; 17:1-8.
- Connelly MA, Gruppen EG, Wolak-Dinsmore J, et al. GlycA, a marker of acute phase glycoproteins, and the risk of incident type 2 diabetes mellitus: Prevend study. Clin Chem Acta 2016; 452:10-107.
- Ritchie SC, Würtz P, Nath AP, et al. The biomarker GlycA is associated with chronic inflammation and predicts long-term risk of severe infection. Cell Systems 2015; 1:293-301.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Paladugu Devi Navya1*, Kaarthikeyan G1 and Selvi Raj J2
1Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical sciences (SIMATS), Saveetha University, Chennai, India2Department of Biochemistry, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical sciences(SIMATS), Saveetha University, Chennai, India
Received: 20-Aug-2022, Manuscript No. jrmds-22-51925; , Pre QC No. jrmds-22-51925(PQ); Editor assigned: 22-Aug-2022, Pre QC No. jrmds-22-51925(PQ); Reviewed: 06-Sep-2022, QC No. jrmds-22-51925(Q); Revised: 09-Sep-2022, Manuscript No. jrmds-22-51925(R); Published: 16-Sep-2022
