Research - (2022) Volume 10, Issue 1
Estimation of Incidence and Awareness of Obstructive Sleep Apnea in Class II Malocclusion in Young Age Adult Population as Compared to Class I Malocclusion in Vidharba Population Using Questionnaire and Lateral Cephalogram
Renuka Talla*, Ranjit Kamble, Jeni Ann Mathew and Karthika Nambiar
*Correspondence: Renuka Talla, Department of Orthodontics and Dentofacial Orthopaedics, Sharad Pawar Dental College and Hospital, Datta Meghe Medical Sciences, Sawangi (Meghe), Wardha (Maharastra), India, Email:
Abstract
The condition known as Obstructive sleep apnea (OSA) has few characteristic features which include recurring collapse of the upper airway when asleep which further leads to frequent and repetitive episodes of desaturation leading to awakening. If Obstructive Sleep Apnea (OSA) is left untreated it may affect the “Neuro-cognitive” function of the individual. Berlin questionnaire is one of the screening tools which is simple and can be used widely. A total of 200 patients were selected within the age group of 18-30 years for the study. Based on the skeletal pattern all the patients were divided into two groups with each group containing 100 patients’ skeletal class I and skeletal class II. With the above questionnaire it was found out if the patient is aware of his/her condition i.e. OSA. After the patients completed the questionnaire, lateral Cephalometric was taken to evaluate. Statistically significant difference was found for PFH, PHB, SPAS, MAS, IAS, and TGH. Study indicates that the awareness of Obstructive sleep apnea (OSA) among the individuals is poor. Our study has shown high estimate of Obstructive sleep apnea (OSA) in skeletal class II cases when compared to skeletal class I.
Keywords
Obstructive sleep apnea, Skeletal class ii, Berlin questionnaire, Hyoid bone
Introduction
The condition known as Obstructive sleep apnea (OSA) has few characteristic features which include recurring collapse of the upper airway when asleep which further leads to frequent and repetitive episodes of desaturation leading to awakening. The condition has become common with an alarming rise in the prevalence of Obstructive Sleep Apnea (OSA), the apnea-hypopnea index (AHI) has shown the rates of moderate to severe Obstructive Sleep Apnea to be upto 50% in the recent studies [1].
Obstructive Sleep Apnea (OSA)may lead to severe medical complications. Obstructive sleep apnea may be an etiological factor for hypertension, ischemic heart disease, stroke , congestive heart failure, intolerance to glucose and also impotence. If Obstructive Sleep Apnea (OSA) is left untreated it may affect the “Neuro-cognitive” function of the individual. Obstructive Sleep Apnea show symptoms like daytime sleepiness, decreased concentration and memory which can all lead to increased risk of accidents. Based on studies as well as published data Obstructive Sleep Apnea is said to be under-recognized throughout the world mainly in the primary care settings [2].
However, the population at risk is quite large and the screening appropriately remains to be limited. Berlin questionnaire is one of the screening tools which is simple and can be used widely. This questionnaire has been studied in primary care settings. This questionnaire aids in classifying the individuals into high risk and low risk groups of Obstructive Sleep Apnea (OSA) based on their symptoms like snoring, obesity, sleepiness and hypertension. In a primary care population. This questionnaire has specificity as well as positive predictive value [3].
In recent years Cephalometric has become important not only in dentistry but also in other fields such as evaluation of the airway and diagnosis of OSA-hypoapnea syndrome. The most commonly and practically used method is the Cephalometric. Cephalometry has served as an exceptional tool for the analysis and planning of a treatment but has also helped in diagnosis of the individuals with Obstructive Sleep Apnea (OSA). Abnormal dentofacial morphologies such as constricted airway particularly the upper airway, micrognathia, altered position of hyoid bone, steepening of the mandibular plane, large tongue and long face as well as increased ANB angle have been registered in such individuals.
As lateral cephalometry is considered as the standard radiograph for viewing dentofacial structures. In the current study the lateral cephalometry is used to evaluate the soft tissues such as the UA, to analyse the extent of collapse of UA which include the tongue (thickness and macroglossia or micrognathia) in upright position [4]. Indepth study of the soft palate as well as the upper airway can be carried out with this study [5].
There is a steady increase in the awareness of the OSA throughout the world in the past three decades yet the acquaintance and alertness of OSA among the general population is very less considering the vast population and the amount of cases going undiagnosed. Extensive investigation among population has not been recorded. In light of paucity of studies conducted in Vidarbha population, this study is being conducted to estimate the incidence of Obstructive Sleep Apnea (OSA) and to assess the awareness of OSA among these subjects.
Material and Methods
The study has been conducted on patients reporting to the dental college who were diagnosed with “skeletal class I and class II malocclusions”. A total of 200 patients were selected within the age group of 18-30 years for the study. The exclusion parameter for patients suffering from disorders and syndromes chiefly like respiratory and developmental and of any systemic origin as well as any skeletal abnormality and patients with metabolic disorders which are contraindicated for radiation exposure remained. All the patients were told about the procedure and a written consent was taken from all the patients and ethical clearance was obtained from the ethical committee of the institute before the commencement the study.
Based on the skeletal pattern all the patients were divided into two groups with each group containing 100 patients’ skeletal class I and skeletal class II. After the patient reported to the department, a questionnaire was handed over to the patient for surveying the awareness regarding Obstructive Sleep Apnoea.
Questionnaire
This questionnaire comprises of 10 sets of questions organized into three categories that attempt in assessing the awareness of the respondent's as well as the knowledge and their attitude towards OSA (Figure 1) The first section is regarding snoring, the second section is regarding daytime fatigue and sleepiness, and the last section is regarding the medical history and anthropometric measures such as hypertension and BMI. This questionnaire categorises the individuals into high risk or low risk of OSA depending on the self-reports of “daytime sleepiness, snoring, hypertension and obesity” (Figure 2).
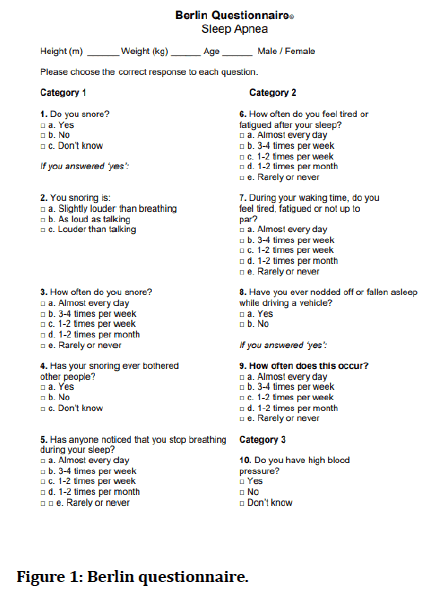
Figure 1: Berlin questionnaire.
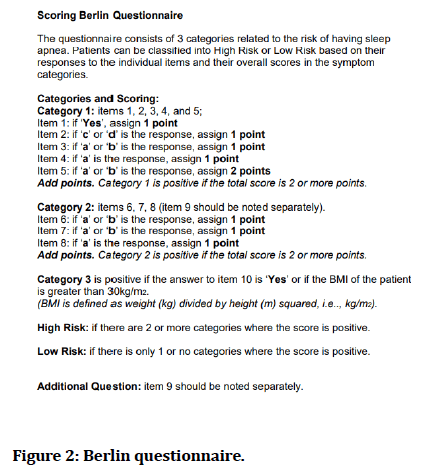
Figure 2: Berlin questionnaire.
This questionnaire likewise includes information about “age, sex, height and weight”. The responses are further analysed by the medical staff and based on this analysis the scoring is carried out. Positive responses in at least two categories indicate that the individual is at high risk of Obstructive Sleep Apnea (OSA).
With the above questionnaire we found out if the patient is aware of his/her condition i.e. OSA. The scoring was done and patients were categorised into high or low risk depending on the patient’s response. With this questionnaire an affirmation is obtained regarding the patient’s awareness and amount of risk of Obstructive Sleep Apnea (Figure 2).
After the patients completed the questionnaire, lateral cephalometry was taken to evaluate. All the patients were subjected to “Cephalometric radiographic examination” using the standard protocols (Figures 3 and 4).
Figure 3: Cephalometric radiographic examination.

Figure 4: Cephalometry.
Angular measurement
• SNA: It is derived by the angle between Nasion to
Sella and Point A.
• SNB: It is derived by the angle between the plane
constructed from Nasion to Sella and Point B.
• ANB: Difference between SNA and SNB denotes ANB.
Hard tissue linear measurement (Figure 5)
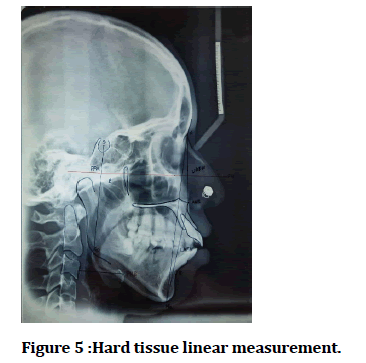
Figure 5:Hard tissue linear measurement.
• Upper anterior facial height (UAFH): It is derived
from N to the anterior nasal spine.
• Lower anterior facial height (LAFH): It is derived
from ANS to menton.
• Posterior facial height (PFH): It is derived from Sella
(S) to the Gonion (Go).
• Position of hyoid bone: It is derived from anterior
hyoid (AH) to the cervical column measured parallel to Frankfort horizontal plane (FH), the horizontal
position of the hyoid bone.
Linear measurement of upper airway space and soft tissue
• Superior posterior airway space (SPAS): It is derived
from a point on the posterior outline of the soft palate
extending to the closest point on the pharyngeal wall.
• Middle airway space (MAS): It is measured from the
intersection of the posterior border of the tongue and
the inferior border of the mandible to the closest
point on the posterior pharyngeal wall.
• Inferior airway space (IAS): It is measured between
the posterior pharyngeal wall and the point of
intersection of the tongue with hyoid bone.
• Tongue length (TGL): It is measured between the tip
of the tongue and the base of the deepest point of
epiglottis.
• Tongue height (TGH): It is the linear distance between
line drawn perpendiculars to the TGL line to a point
on the most superior curvature of the tongue dorsum.
• Soft palate length (PNS − P): The linear distance
between posterior nasal spine (PNS) and P (Figure 6).
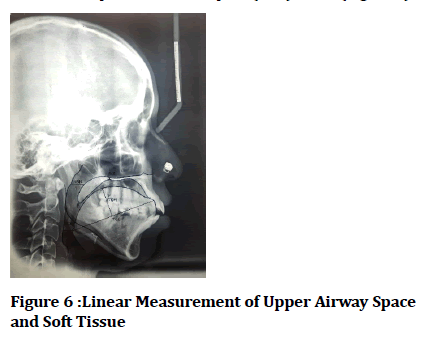
Figure 6:Linear Measurement of Upper Airway Space and Soft Tissue.
Measurement of upper airway and soft-tissue area (Figure 7)
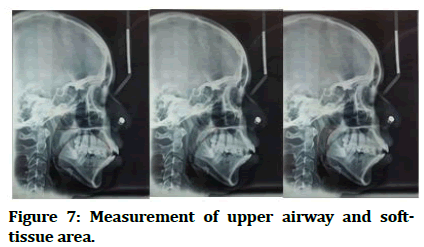
Figure 7:Measurement of upper airway and softtissue area.
• Nasopharynx: The area outlined by a line between R
and PNS, an extension of the palatal plane to the
posterior pharyngeal wall, and the posterior
pharyngeal wall.
• Oropharynx: The area outlined by the inferior border
of the nasopharynx, the posterior surface of the soft
palate and tongue, a line parallel to the palatal plane
through the point Et, and the posterior pharyngeal
wall.
• Hypo pharynx: The area outlined by the inferior
border of the oropharynx, the posterior surface of the
epiglottis, a line parallel to the palatal plane through
the point C4, and the posterior pharyngeal wall.
• Tongue: The area outlined by the dorsal configuration
of the tongue surface and lines that connect TT,
retrognathion (RGN), hyoidale (H), and Eb.
• Soft palate: The area confined by the outline of the
soft palate that starts and ends at PNS through P.
These parameters were evaluated in all the patients and compared between class I malocclusion and class II skeletal malocclusion cases.
Results
Questionnaire responses showed that in class I group out of 100 samples only 18.6% individuals were aware of Obstructive Sleep Apnea whereas in class II group out of 100 individuals23.8% individuals were aware of Obstructive Sleep Apnea (OSA). Students unpaired t test using the descriptive and inferential statistics, the statistical analysis was carried out. The software which was used for the analysis was SPaS 27.0 version and p<0.05 is considered as level of significance. Angular measurements SNA, SNB and ANB showed statistical significance (p<0.05) as the angles suggested the maxillomandibular relationship in the respective skeletal classes. (Table 1, Figure 8).
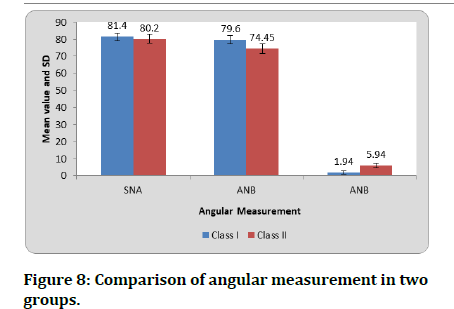
Figure 8:Comparison of angular measurement in two groups..
| Class I | Class II | t-value | p-value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| SNA | 81.4 | 2.27 | 80.2 | 2.64 | 2.03 | 0.046* |
| ANB | 79.6 | 2.47 | 74.45 | 2.82 | 8.1 | 0.0001* |
| ANB | 1.94 | 0.99 | 5.94 | 1.32 | 14.24 | 0.0001* |
Table 1: Comparison of angular measurement in two groups.
Statistically significant difference was found for Posterior facial height (PFH) (p<0.05).
The position of hyoid bone (PHB) also showed statistically significant difference with larger values in class I group when compared to class II (Table 2, Figure 9).
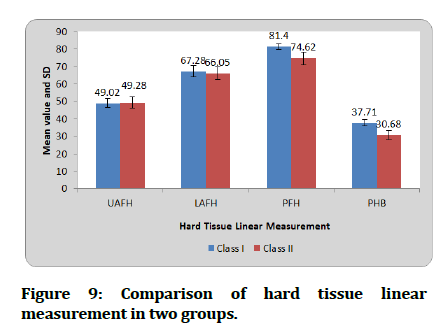
Figure 9:Comparison of hard tissue linear measurement in two groups.
| Class I | Class II | t-value | p-value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| UAFH | 49.02 | 2.65 | 49.28 | 3.28 | 0.36 | 0.72 |
| LAFH | 67.28 | 3.16 | 66.05 | 3.65 | 1.5 | 0.13 |
| PFH | 81.4 | 1.64 | 74.62 | 3.59 | 10.12 | 0.0001* |
| PHB | 37.71 | 1.67 | 30.68 | 2.63 | 13.33 | 0.0001* |
Table 2: Comparison of Hard Tissue Linear Measurement in Two Groups.
The comparison of airway analysis of the “upper and lower airway space” in both the groups showed a significant statistical difference in Superior posterior airway space (SPAS), Middle airway space (MAS), Inferior airway space (IAS). The tongue height (TGH) showed statistically significant difference (p<0.05), tongue height in class II group was found to be less when compared to the class I group. How ever there was no statistical significance for tongue length (TGL). Statistically significant difference was also seen with nasopharynx, oropharynx and hypo pharynx. (Tables 3 and 4, Figures 10 and 11).
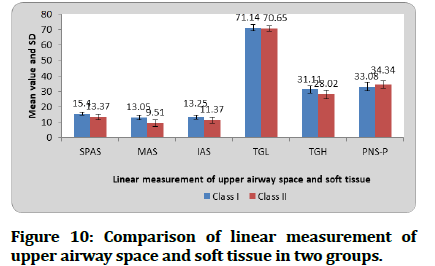
Figure 10:Comparison of linear measurement of upper airway space and soft tissue in two groups.
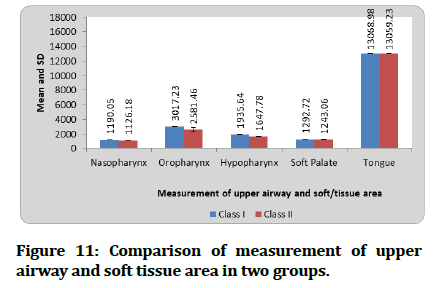
Figure 11:Comparison of linear measurement of upper airway space and soft tissue in two groups.
| Class I | Class II | t-value | p-value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| SPAS | 15.4 | 1.09 | 13.37 | 1.68 | 5.98 | 0.0001* |
| MAS | 13.05 | 1.25 | 9.51 | 2.09 | 8.58 | 0.0001* |
| IAS | 13.25 | 1.29 | 11.37 | 1.98 | 4.7 | 0.0001* |
| TGL | 71.14 | 1.86 | 70.65 | 1.76 | 1.11 | 0.27 |
| TGH | 31.11 | 2.47 | 28.02 | 2.75 | 4.92 | 0.000* |
| PNS-P | 33.08 | 2.64 | 34.34 | 2.27 | 2.13 | 0.037* |
Table 3: Comparison of linear measurement of upper airway space and soft tissue in two.
| Class I | Class II | t-value | p-value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Nasopharynx | 1190.05 | 6.62 | 1126.18 | 35.3 | 10.51 | 0.0001* |
| Oropharynx | 3017.23 | 20.5 | 2581.46 | 288.6 | 8.91 | 0.0001* |
| Hypopharynx | 1935.64 | 9.14 | 1647.78 | 35.37 | 46.6 | 0.0001* |
| Soft Palate | 1292.72 | 8.51 | 1243.06 | 31.95 | 8.83 | 0.0001* |
| Tongue | 13068.98 | 58.67 | 13059.23 | 53.76 | 0.72 | 0.47 |
Table 4: Comparison of measurement of upper airway and soft-tissue area in two groups.
Discussion
Several questionnaire surveys for Obstructive Sleep Apnea (OSA) have been carried out in several studies to assess the awareness and the degree of severity. Our study is carried out to assess the awareness of “Obstructive Sleep Apnea (OSA)” among the individuals by means of the help of the questionnaire and evaluate the individuals with the help of lateral cephalography. A validated Berlin questionnaire was used for the study. Two groups were selected for the study, “skeletal class I and skeletal class II”. A total of 200 samples were selected within the age group of 18-30 years for the study. The patients suffering from disorders and syndromes chiefly like respiratory and developmental and of any systemic origin as well as any skeletal abnormality and patients with metabolic disorders which are contraindicated for radiation exposure remained excluded from the study as the individuals had to undergo lateral cephalography after the questionnaire for the study. The distribution of 200 samples as two groups was based on the type of skeletal class into skeletal class I and skeletal class II such that each group consisted of 100 samples.
The results for questionnaire showed that out of all the questions most patients in the questionnaire marked snoring as a symptom. Snoring is an important indicator of Obstructive sleep apnea. Berlin questionnaire not only aids in knowing the awareness of the individual to Obstructive Sleep Apnea but also gives an estimate of the severity of the disease. From the questionnaire we found that there was low understanding and poor acquaintance of Obstructive sleep Apnea among the people.
Cephalometrics has been used for several years now for evaluation of growth assessment and development assessment. It has aided scrutiny of anomalies of dental, skeletal as well as soft tissue structures. In our study we have used lateral cephalography for the evaluation of Obstructive Sleep Apnea (OSA). A normal nasal airway depends on the anatomical dimensions of the airway which can be evaluated by lateral cephalography. The classification of the groups was carried out on the basis of ANB angle. i.e. “Skeletal Class I and Skeletal Class II” cases.
When the posterior facial height (PFH) was evaluated, it was found that there was significant difference in posterior facial height (PFH). With the increase in posterior facial height there was an increase in tongue area subsequently, this is supported by study conducted by Hwang et al [6]. Our study has shown that the facial height has an influence on the airway space showing that with an increase in posterior facial height (PFH) there was increase in Superior posterior airway space (SPAS) , Middle airway space (MAS) and Inferior airway space (IAS).
Our study has shown that the dimensions of soft palate length (PNS–P) in class II cases were larger when compared to class I cases. Jena et al in his study evaluated the sagittal mandibular development effects on the dimensions of the awake pharyngeal airway passage and found out that the length of soft palate (PNS – P) was greater due to the backward positioning of the tongue causing compression of the soft palate resulting in the decreased thickness and increased length. This study is in support to our findings and also explains that it is common among the subjects who snore and have Obstructive sleep apnea than the normal individuals [7].
In our study the position of hyoid bone (PHB) also showed statistically significant difference with larger values in class I group when compared to class II. The skeletal configuration showed a correlation with the position of hyoid bone antero-posteriorly in relation cervical vertebrae (C3). Our findings are supported by Abu et al. as in his study he found the hyoid bone was positioned upwards and backwards [8]. Hyoid bone has a great impact in maintenance of upper airway dimensions.
Kalgotra et al. in their study found that tongue was placed closer to the pharyngeal wall in skeletal class II cases [9]. In our study there was reduced airway space in skeletal class II cases. This study supports our finding of reduced Superior posterior airway space (SPAS), Middle airway space (MAS) and Inferior airway space (IAS) in skeletal class II cases as the tongue is placed closer to the pharyngeal wall in turn reducing the airway space.
The tongue height (TGH) showed statistically significant difference (p<0.05), tongue height in class II group was found to be less when compared to the class I group. There was no statistical significance found with the tongue length (TGL) between the skeletal class I and skeletal class II, Our findings are supported by the study conducted by Torgut et al. in which, the tongue height in class II cases were less when compared to class I and class III [10]. In our study, no significant difference was found in tongue length between malocclusions.
Conclusion
To conclude, our study indicates that the awareness of Obstructive sleep apnea (OSA) among the individuals is poor. Only about 1 in 10 individuals were aware of Obstructive sleep apnea (OSA). Our study has shown high estimate of Obstructive sleep apnea (OSA) in skeletal class II cases when compared to skeletal class I. The evaluation of lateral cephalography of the individuals indicated that there was significant difference in posterior facial height (PFH). With the increase in posterior facial height there was an increase in tongue area, Superior posterior airway space (SPAS), middle airway space (MAS) and Inferior airway space (IAS) subsequently.
The effect of development of mandible in sagittal plane affects the dimensions of the pharyngeal airway passage and length of soft palate (PNS–P) due to the backward positioning of the tongue. There was also a correlation with the position of hyoid bone antero-posteriorly in relation cervical vertebrae (C3).
Tongue height in class II group was found to be less whereas; the tongue length was not affected. The positioning of tongue in skeletal class II cases was found to be closer to the pharyngeal wall when compared to skeletal class I cases.
References
- Sia CH, Hong Y, Tan LW, et al. Awareness and knowledge of obstructive sleep apnea among the general population. Sleep Med 2017; 36:10-17.
- BaHammam AS, Alrajeh MS, Al-Jahdali HH, et al. Prevalence of symptoms and risk of sleep apnea in middle-aged Saudi males in primary care. Saudi Med J 2008; 29:423.
- Hiestand DM, Britz P, Goldman M, et al. Prevalence of symptoms and risk of sleep apnea in the US population: Results from the national sleep foundation sleep in America 2005 poll. Chest 2006; 130:780-786.
- Laxmi NV, Talla H, Meesala D, et al. Importance of cephalographs in diagnosis of patients with sleep apnea. Contemp Clin Dent 2015; 6:S221.
- Kaur S, Rai S, Sinha A, et al. A lateral cephalogram study for evaluation of pharyngeal airway space and its relation to neck circumference and body mass index to determine predictors of obstructive sleep apnea. J Indian Acad Oral Med Radiol 2015; 27:2.
- Hwang YI, Lee KH, Lee KJ, et al. Effect of airway and tongue in facial morphology of prepubertal Class I, II children. Korean J Orthod 2008; 38:74-82.
- Jena AK, Singh SP, Utreja AK. Sagittal mandibular development effects on the dimensions of the awake pharyngeal airway passage. Angle Orthod 2010; 80:1061-1067.
- Abu Allhaija ES, Al-Khateeb SN. Uvulo-glosso-pharyngeal dimensions in different anteroposterior skeletal patterns. Angle Orthod 2005; 75:1012-1018.
- Kalgotra S, Mustag M. Position of tongue in skeletal class II & class III. A cefalometric study. J Dent Med Sci 2016; 15:33-38.
- Torgut AG, Akan S. Mandibular symphysis morphology in different skeletal malocclusions and its correlation with uvulo-glossopharyngeal structures. CRANIO 2021; 39:533-540.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Renuka Talla*, Ranjit Kamble, Jeni Ann Mathew and Karthika Nambiar
Department of Orthodontics and Dentofacial Orthopaedics, Sharad Pawar Dental College and Hospital, Datta Meghe Medical Sciences, Sawangi (Meghe), Wardha (Maharastra), IndiaCitation: Renuka Talla, Ranjit Kamble, Jeni Ann Mathew, Karthika Nambiar, Estimation of Incidence and Awareness of Obstructive Sleep Apnea in Class II Malocclusion in Young Age Adult Population as Compared to Class I Malocclusion in Vidharba Population Using Questionnaire and Lateral Cephalogram, J Res Med Dent Sci, 2022, 10(1): 6-12
Received: 14-Dec-2021, Manuscript No. JRMDS-21-44628; , Pre QC No. JRMDS-21-44628 (PQ); Editor assigned: 16-Dec-2021, Pre QC No. JRMDS-21-44628 (PQ); Reviewed: 30-Dec-2021, QC No. JRMDS-21-44628; Revised: 04-Jan-2022, Manuscript No. JRMDS-22-44628 (R); Published: 11-Jan-2022
