Research - (2020) Volume 8, Issue 1
Evaluate and Compare the Effect of Different Marginal Cement Space Parameter Setting in the CAD Software on the Marginal and Internal Fitness of Monolithic Zirconia Crowns with Different Types of Luting Agents (A comparative in vitro study)
Eman D Hammood* and Adel F Ibraheem
*Correspondence: Eman D Hammood, Department of Restorative and Aesthetic Dentistry, College of Dentistry, University of Baghdad, Iraq, Email:
Abstract
Objectives: The purpose of this in vitro study was to evaluate and compare the effect of different marginal cement space parameter setting in the CAD software on the marginal and internal fitness of monolithic zirconia crowns with different luting agent.
Materials and method: 48 sound human maxillary first permanent premolar teeth of comparable size and shape extracted for orthodontic purposes were collected and selected to be used in this in vitro study. All the dimensions of each crown were tested with using one way ANOVA in order to reduce the confounding variables. The teeth samples were divided into two main groups according to the different marginal cement space parameter setting (n=24) as following: Group I: 0 cement space around the margin and additional cement space of 80 Mm starting 1mm above the finish lines of the teeth. Group II: 25 Mm cement space around the margin and additional cement space of 80 Mm starting 1mm above the finish lines of the teeth. Each group was subdivided into three subgroups according to the type of luting material (n=8) :(IA, IIA) cemented with Rely X™ Ultimate adhesive,(IB, IIB) cemented with Rely X™ Unicem 200 self-adhesive and (IC, IIC) cemented with conventional Riva luting plus glass ionomer. The standard preparation for full counter monolithic zirconia crown restorations was done with light chamfer finishing line 0.8mm, axial reduction 1-1.5mm,occlso-axial height 4mm (palataly and buccally) ,anatomical occlusal reduction and total convergence angle 6 degree. The teeth were scanned with inEos X5 extra -oral digital scanner (Sirona, Germany) , then fabricated with Sirona In-Lab MC X5 milling device. The internal and marginal fitness of crown was evaluated by direct measurement of cement film thickness through sectioning procedure using a digital microscope at a magnification of60 X at eleven different measuring points for each specimen, which represented four different areas of measurement (margin, chamfer, axial and occlusal).
Results: The results of this study showed that the different marginal cement space parameter setting used was significantly improve the marginal and internal adaptation of monolithic zirconia crown restoration .The Rely X™ Ultimate adhesive luting agent had a lowest mean value of marginal discrepancy as compared with the other types of luting agent that was used in this study. Conclusions: using of 25μm cement space at the marginal area resulted in reducing the marginal and internal gaps. The Rely X™ Ultimate adhesive luting agent provided the lowest marginal and internal gaps as compared with other types of luting used in this study.
Keywords
Cement space, Hydraulic pressure, Marginal discrepancy
Introduction
The success of all ceramic restorations depends mainly on the marginal and internal fitness. A good marginal fitness is anticipated to minimize accumulation of dental plaque, secondary caries, pulpitis, which subsequently lead to damage the tooth structures and its supporting periodontium, then the long life of crown restoration decreases [1,2]. These defects are common reasons for the failure of crown restorations [3]. Kasloff, et al. said in order to achieve an ideal restoration, the crown must be made to fit intimately over the prepared tooth [4,5]. The clinically, acceptable limit of the marginal discrepancies is reported to be less than 120 μm [6]. A number of factors might affect the fitness of crown restoration such as the degree of convergence angle of preparation, location of the margin (sub or supra-gingival), quality of scanner-milling device–milling bur, thickness of cement spacer, amount and viscosity of luting cement, seating aid procedures such as vibratory techniques and type of loading during cementation either static or dynamic [7-9]. White, et al. in their study showed that the marginal discrepancy was increased after cementation [10,11].
Pilo et al. said when the crown restoration precisely fits the prepared tooth, the escape pathway of cement between the crown restoration and prepared tooth surface become more difficult [5,12]. The final effects are creation of premature, occlusal contacts, inappropriate proximal contacts, marginal discrepancies and lack of coziness [5]. Many methods have been suggested previously in order to minimize post cementation marginal discrepancy.
These include:
1. Internal relief space [13,14], Many techniques have been suggested to provide the internal relief space, Hager et al. categorized the internal relief into subtractive and additive method [11,15]. Subtractive methods involve (a) Aqua regia etching was first discovered by Hollenback, et al. [16] (b) Internal mechanical grinding of castings (c) Internal carving of wax patterns before casting (d) Eelectrochemical milling [5,11,17]. The additive method involves application of diespacer onto the stone die or use of tin foil [18].
2. Venting [19].
3. Cement escape channels [13].
From all above studies showed that the best and most popular method to improve seating of crown restoration was the internal relief with die spacer.
Materials and Methods
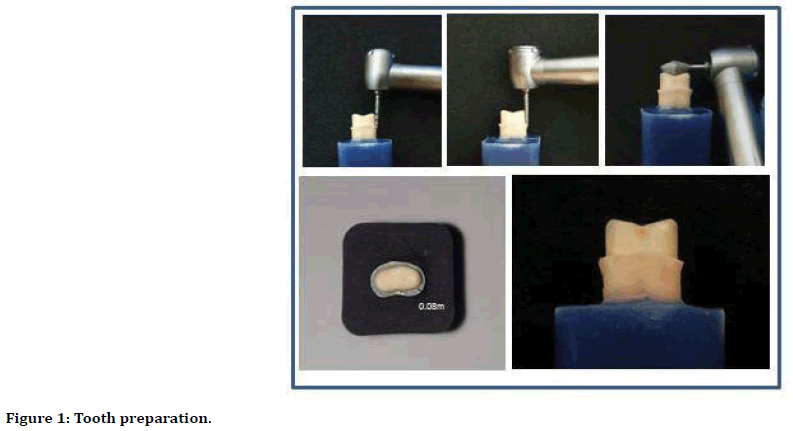
Forty–eight sound human teeth (maxillary first permanent premolar) of comparable shape and size extracted for orthodontic purposes were collected to be used in this in vitro study. All teeth were then embedded individually in cold cure acrylic resin block 2 mm below the CEJ. Dental surveyor was used to align the long axis of the tooth to be vertical to the horizontal plane of the mold. In order to achieve a standardized preparation for all teeth, the preparation was carried out by one operator. A modified dental surveyor was used to prepare the axial walls of the tooth to gate a constant degree of tapering according to the tapering of the preparation and finishing burs used. All the teeth were prepared to receive the monolithic zirconia crown restoration with the following features of preparation: Light chamfer finishing line with uniform thickness of 0.8 mm in depth, axial reduction 1-1.5 mm, occlso-axial height 4 mm (palataly and buccally), anatomical occlusal reduction and total convergence angle 6 degree (Figure 1).
Figure 1. Tooth preparation.
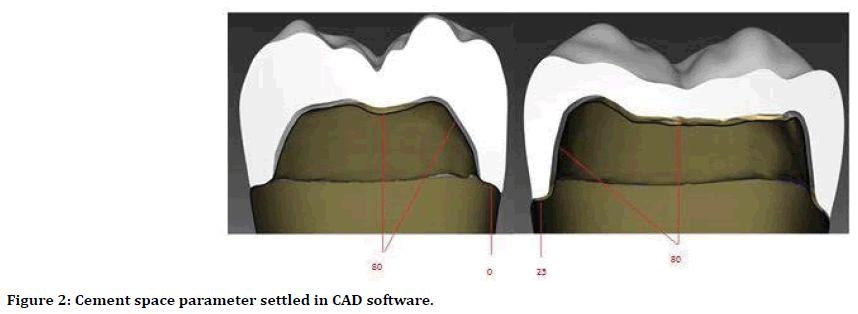
All the samples were scanned with the in Eos X5 extra-oral digital scanner (Sirona Dental Systems, Germany) with CEREC Premium software, version (16.1 ) to produce a 3D digital images for all the teeth, and randomly divided into two main groups I and II according to the design of cement space parameter (n=24): The cement space parameter in Group I was setted at 0 mm around the margin and additional cement space of 80 mm starting 1 mm above the finish lines of the teeth and for Group II was 25 mm around the margin and additional cement space of 80 mm starting 1 mm above the finish lines of the teeth (Figure 2).
Figure 2. Cement space parameter settled in CAD software.
Then the crowns were milled with the same milling machine MC X5 (Sirona Dental System, Germany), from pre-sintered monolithic KATANATM zirconia disc, then fired in fire HTC speed (Sirona, Germany), glazed and sandblasted with aluminum oxide particles ≤ (50 μm) at max. Pressure of 2.5 bars at a distance of 10 mm for 15 sec. Each main group was divided into three subgroups according to the type of cement material (n=8) :(IA,IIA) Rely X™ Ultimate adhesive luting agent(3M ESPE, Germany), (IB,IIB) cemented with Rely X™ Unicem 200 self-adhesive luting agent (3M ESPE, Germany) and (IC,IIC) conventional Riva luting plus glass ionomer cement (SDI, Australia).
The cement was painted over the entire surfaces then placed over its respective tooth with rocking movement and maximum index finger pressure as in the clinical situation. For the purpose of standardization, the crown with its respective tooth was then seated inside the sample holding and cementation device and was kept under load (5 kg) for 6 min. The internal and marginal fitness of crown was evaluated by direct measurement of cement film thickness in mm through sectioning procedure. The measurements were done using a digital microscope at a magnification of 60 X with (Dino-capture) software and Image J software (version 1.5) (U.S. National Institutes of Health, Bethesda, MA, USA) at eleven different measuring points for each specimen, which represented four different areas of measurement (margin, chamfer, axial and occlusal) (Figure 3).
Figure 3. The sectioned samples.
Results
The descriptive statistical results for all subgroups showed, the highest mean value of the gap was recorded at the occlusal area. While the lowest mean value of the gap was recorded mostly at the marginal area (Table 1). T-test showed that different cement space designs were significantly affect both marginal and internal fitness of the tested monolithic zirconia crown restoration (p=0.000) (Table 2) while the result of 1-Way ANOVA test indicated that different types of luting agents were significantly affect the adaptation of zirconia crown (p ≤ 0.005). The Turkey HSD test revealed statistical differences between group IA-IB, IA-IC in both marginal and internal areas, while difference between IB- IC in the marginal area only. On the other hand, these differences noticed between IIA-IIB and IIA-IIC in marginal area only (Table 3). The Pearson’s correlation test was showed a moderate positive correlation between the marginal and internal gaps within Group I and weak negative correlation within Group II (Table 4).
| Groups | Subgroups | Areas | N | Mean | Std. Deviation | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| Group I | A | Marginal | 8 | 61.12 | 5.14 | 56.02 | 68.2 |
| Chamfer | 8 | 75.17 | 5.78 | 67.29 | 85.19 | ||
| Axial | 8 | 87.34 | 8.77 | 71.3 | 99.83 | ||
| Occlusal | 8 | 138.86 | 12.56 | 120.14 | 151.71 | ||
| Internal | 8 | 95.45 | 3.58 | 88.76 | 99.82 | ||
| B | Marginal | 8 | 76.68 | 4.1 | 70.14 | 82.04 | |
| Chamfer | 8 | 76.36 | 7.8 | 65.3 | 89.9 | ||
| Axial | 8 | 92.1 | 5 | 83.38 | 96.46 | ||
| Occlusal | 8 | 146.93 | 9.51 | 129.31 | 159.06 | ||
| Internal | 8 | 105.58 | 4.8 | 97.17 | 114.41 | ||
| C | Marginal | 8 | 70.85 | 6.53 | 61.36 | 80.53 | |
| Chamfer | 8 | 74.53 | 2.94 | 68.3 | 76.97 | ||
| Axial | 8 | 98.32 | 9.76 | 82.47 | 109.09 | ||
| Occlusal | 8 | 137.04 | 16.09 | 113.56 | 159.82 | ||
| Internal | 8 | 102.88 | 5.29 | 93.57 | 109.52 | ||
| Group II | A | Marginal | 8 | 45.17 | 4.85 | 37.34 | 50.23 |
| Chamfer | 8 | 58.23 | 6.65 | 46.83 | 65.28 | ||
| Axial | 8 | 56.59 | 8.61 | 45.48 | 66.66 | ||
| Occlusal | 8 | 64.36 | 9.73 | 54.68 | 83.82 | ||
| Internal | 8 | 63.47 | 7.42 | 54.88 | 74.89 | ||
| B | Marginal | 8 | 50.32 | 3.26 | 46.02 | 55.12 | |
| Chamfer | 8 | 47.87 | 11.18 | 32.64 | 59.91 | ||
| Axial | 8 | 54.66 | 5.17 | 48.88 | 65.15 | ||
| Occlusal | 8 | 71.72 | 4.37 | 65.05 | 79.74 | ||
| Internal | 8 | 58.08 | 4.81 | 50.01 | 65.19 | ||
| C | Marginal | 8 | 54.79 | 3.2 | 51.13 | 60.08 | |
| Chamfer | 8 | 58.41 | 6.79 | 50.12 | 69.33 | ||
| Axial | 8 | 59.75 | 5.32 | 50.47 | 65.3 | ||
| Occlusal | 8 | 65.3 | 4.39 | 60.35 | 73.21 | ||
| Internal | 8 | 60.73 | 4.96 | 55.31 | 69.25 |
Table 1: Descriptive statistics of the gap at the different areas of the six subgroups measured in μm.
| Subgroups | Area | Groups | N | Mean | Std.Deviation | t | Sig. |
|---|---|---|---|---|---|---|---|
| A | Marginal | I | 8 | 61.12 | 5.14 | 6.38 | 0 |
| II | 8 | 45.17 | 4.85 | ||||
| Internal | I | 8 | 95.45 | 3.58 | 10.99 | 0 | |
| II | 8 | 63.47 | 7.42 | ||||
| B | Marginal | I | 8 | 76.68 | 4.1 | 14.22 | 0 |
| II | 8 | 50.32 | 3.26 | ||||
| Internal | I | 8 | 105.58 | 4.8 | 19.76 | 0 | |
| II | 8 | 58.08 | 4.81 | ||||
| C | Marginal | I | 8 | 70.85 | 6.53 | 6.25 | 0 |
| II | 8 | 54.79 | 3.2 | ||||
| Internal | I | 8 | 102.88 | 5.29 | 16.43 | 0 | |
| II | 8 | 60.73 | 4.96 |
Table 2: T-test for comparison of the marginal and internal gaps between the two main groups.
| Areas | Groups I | Mean Difference (I-J) | Std. Error | Sig. |
| Marginal | IA IB | -15.55750* | 2.6762 | 0.000 (HS) |
| IA IC | -9.72750* | 2.6762 | 0.004 (S) | |
| IB IC | -9.72750* | 2.6762 | 0.004 (S) | |
| internal | IA IB | -10.12375* | 2.30743 | 0.001 (HS) |
| IA IC | -7.42625* | 2.30743 | 0.011 (S) | |
| IB IC | 2.6975 | 2.30743 | 0.484(NS) | |
| Areas | Groups II | Mean Difference (I-J) | Std. Error | Sig. |
| Marginal | IIA IIB | -5.15000* | 1.92236 | 0.036 (S) |
| IIA IIC | -9.61375* | 1.92236 | 0.000 (HS) | |
| IIB IIC | -4.46375 | 1.92236 | 0.075(NS) | |
| internal | IIA IIB | 5.39 | 2.92623 | 0.181(NS) |
| IIA IIC | 2.7375 | 2.92623 | 0.624(NS) | |
| IIB IIC | -2.6525 | 2.92623 | 0.642(NS) |
Table 3: Turkey test for compassion of marginal and internal gps among subgroups (according to the type of luting agent).
| Groups | r | p value | Sig. |
|---|---|---|---|
| I | 0.604 | 0.004 | HS |
| II | -0.381 | 0.066 | NS |
Table 4: Correlation between marginal and internal gap of the two main groups.
Discussion
The results of this study showed that a different spacer design and different types of luting agents used were significantly affect the marginal and internal fitness of monolithic zirconia crown restoration, thus the null hypothesis was rejected. The statistical results revealed that using of 25 μm spacer instead of 0 μm around the marginal area could reduce the value of marginal and internal discrepancies, this result can be explained by the fact that using 25 μm space at the margin lead to increase the escape pathway of luting material and reducing the hydraulic pressure that was generated within the crown, thus improving the marginal and internal adaptation of the monolithic zirconia crown. Also some author in their studies showed the setting of spacer at 0 μm around the marginal area was leading to intimate contact between the fitting surface of restoration and tooth preparation at the marginal area of finishing line [9,13,14,20]. Resulting in increased the frictional resistance at that area, then increasing the hydraulic pressure and incomplete seating, this finding can be clearly supported when comparing the occlusal film thickness of spaced and unspaced groups at the marginl area. Occlusal film thickness recorded with 25 μm spacer had been reduced to the half that recorded with 0 μm as shown in Table (1).
In order to have a complete picture about the crown seating, different levels of adaptation (marginal, chamfer, axial, occlusal) were evaluated and comparing among them regarding the type of luting agent [21,22,23,24].
Regarding the spacer of 0 μ, when comparing statistical results of its subgroups Table (1), it had been noticed that the lowest mean value of the marginal gap measurement was mainly in subgroups cemented with Rely X™ Ultimate adhesive luting agent followed by conventional Riva luting plus glass ionomer cement.
While the spacer of 25 μ, it had been observed that the lowest mean value of the marginal gap measurement was mainly in subgroups cemented with Rely X™ Ultimate adhesive luting agent followed by Rely X™ Unicem 200 selfadhesive luting agent.
This result could be due to:
1. Low film thickness of Rely X TM Ultimate adhesive luting agent (12 μm) when compared with the other two cements: Rely X™ Unicem 200 (18 μm) and Riva luting plus GIC (17 μm).
2. High flow- ability of Rely X TM Ultimate adhesive luting agent when compared with the other two cements that were used in this study due to has a low viscosity and fine particle size as compared with the other mentioned cements [12,25,26,27].
3. From the results mentioned above, showed that the new spacer design used in this study was attributed to improve the seating of monolithic zirconia crown even, with the cement which had a highest film thickness among the other cements used in this study, that recorded a highest mean gap values with the traditional CAD/CAM design.
The correlation test between the marginal and internal gap for Group I revealed a moderate positive relation between them, with highly statistical significant difference, the positive person`s correlation means that when the marginal gap increased, the internal gap increased. This could be due to the fact that all the steps of teeth preparation and crown fabrication were done under highly controlled and standardized condition. This finding was in agreement with the study of other previous studies who all found a positive relation between the marginal and internal gaps [22,23,28]. From a clinical point of view, this may give an indication that any crown restoration with poor marginal adaptation will mostly have poor internal adaptation.
While the correlation test for Group II revealed a weak negative relation between them, with no statistical significant difference (the negative person`s correlation means that the relation between the marginal ad internal gaps was inverse). This finding is in agreement with study of Borba [28] that showed a negative correlation between the marginal and internal gaps, and found an additional adaptation procedure in the internal area that would not significantly improve restoration fit in the marginal area. The mean values of the marginal and internal gaps of the two main groups of this study fall within the clinically acceptable limits. The direct comparison of the results of this study with the other studies was not available, because there were no other comparable published studies available.
Conclusion
The using of a spacer at the marginal area of the finishing line results in reducing marginal and internal gaps when compared with spacer free design at the marginal area. The Rely X™ Ultimate adhesive luting agent provided the lowest marginal and internal gaps as compared with other types of cement used in this study.
References
- Valderhaug J, Ellingsen JE, Jokstad A. Oral hygiene, periodontal conditions and carious lesions In patients treated with dental bridges. A 15-year clinical and radiographic jottow up study. J Clin Periodont 1993; 20:482-489.
- Syrek A, Reich G, Ranftl D, et al. Clinical evaluation of all-ceramic crowns fabricated from intraoral digital impressions based on the principle of active wave front sampling. J Dent 2010; 38:553-559.
- Sailer I, Feher A, Filser F, et al. Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. International Journal of Prosthodontics, 2007; 20:383-388.
- Kasloff Z. Casting technique and some varipibles. J Prost Dent 1961; 11:533-536.
- Mule SA, Dange SP, Khalikar AN, et al. Effect of varying layers of two die spacers on precementation space of full coverage restorations. J Indian Prosthodont Society 2014; 14:67-75.
- Holmes JR, Bayne SC, Holland GA, et al. Considerations in measurement of marginal fit. J Prost Dent 1989; 62:405-408.
- Boeddinghaus M, Breloer ES, Rehmann P, et al. Accuracy of single-tooth restorations based on intraoral digital and conventional impressions in patients. Clin Oral Invest 2015; 19:2027-2034.
- Shamseddine L, Mortada R, Rifai K, et al. 2016. Marginal and internal fit of pressed ceramic crowns made from conventional and computer-aided design and computer-aided manufacturing wax patterns: an in vitro comparison. The Journal of prosthetic dentistry, 2016; 116:242-248.
- De Paula Silveira AC, Chaves SB, Hilgert LA, et al. Marginal and internal fit of CAD-CAM-fabricated composite resin and ceramic crowns scanned by 2 intraoral cameras. J Prosthet Dent 2017; 117:386-392.
- White SN, Kipnis V. Effect of adhesive luting agents on the marginal seating of cast restorations. J Prosthet Dent 1993; 69:28–31.
- Aditya P, Madhav VNV, Bhide SV, et al. Marginal discrepancy as affected by selective placement of die-Spacer: an in vitro study. J Indian Prosthodont Society 2012; 12:143–148.
- Pilo R, Cardash HS, Baharav H, et al. Incomplete seating of cemented crowns: a literature review. J Prosthet Dent 1988; 59:429–433.
- Eames WB, O'Neal SJ, Monteiro J, et al. Techniques to improve the seating of castings. J Am Dent Assoc 1987; 96:432–437.
- Grajower R, Zuberi Y, Lewinstein I. Improving the fit of crowns with die-spacers. J Prosthet Dent 1989; 61:555–563.
- Hager TS, Gardner FM, Edge MJ. The effect of selective die-spacer placement techniques on seatability of casting. J Prosthodont 1993; 2:56–60.
- Hollenback GM. Precision gold inlays made by a simple technic. J Am Den Assoc 1943; 30:99–109.
- Campagni WV, Preston JD, Reisbick MH. Measurement of paint-on die spacers used for casting relief. J Prosthet Dent 1982; 47:606-611.
- Fusayama T, Ide K, Hosoda H. Relief of resistance of cement of full cast crowns. J Prosthet Dent 1964; 14:354–364.
- Jørgensen KD. Factors affecting the film thickness of zinc phosphate cements. Acta Odontologica Scandinavica 1960; 18:479-490.
- Oliva RA, Lowe JA. Effect of die spacer on the seating of cast restorations on composite core preparations. J Prosthet Dent 1987; 58:29-35.
- Majeed MA, Al-Adel SK. Evaluation of the marginal and internal fitness of full contour CAD/CAM crowns made from zirconia, lithium disilicate, zirconia-reinforced lithium silicate and hybrid dental ceramic by silicone replica technique (A comparative In vitro study). J Gen Environ Resour Conserv 2016; 4:10-20.
- Al-Atyaa ZT, Majeed MA. Comparative Evaluation of the marginal and internal fitness of monolithic CAD/CAM zirconia crowns fabricated from different conventional impression techniques and digital impression using silicone replica technique (An in vitro study). Biomed Pharmacol J 2018; 11:477-490.
- AL-Hawwaz ZM. Ibraheem AF. Marginal and internal fitness of full contour CAD/CAM fabricated zirconia crowns using different digital intra-oral scanners (An In vitro Study). J Eur Applied Microbiol 2018; 12:839-844.
- Albert FE, El-Mowafy OM. Marginal adaptation and microleakage of Procera All-ceramic crowns with four cements. J Prosthet Dent 2004; 17:529-35.
- Pilathadka S, Slezák R, Vahalová D, et al. Influence of different luting agents on the marginal discrepancy of procera® All ceram alumina crown copings: An experimental study. Acta Medica Hradec Kralove 2008; 51:13.
- Hmaidouch R, Neumann P, Mueller WD. Influence of preparation form, luting space setting and cement type on the marginal and internal fit of CAD/CAM crown copings. Int J Comput Dent 2011; 14: 219-226.
- Ali AAA, Sabea NR. Comparison of marginal adaptation, internal fitness and microleakage of zolid, zirconia and empress 2 all-ceramic crown materials (An in vitro study). Mustansiriya Dent J 2018; 10:184-192.
- Borba M, Cesar PF, Griggs JA, et al. Adaptation of all-ceramic fixed partial dentures. Dent Material 2011; 27:1119-1126.
Author Info
Eman D Hammood* and Adel F Ibraheem
Department of Restorative and Aesthetic Dentistry, College of Dentistry, University of Baghdad, IraqCitation: Eman D Hammood, Adel F Ibraheem, Evaluate and Compare the Effect of Cement Space Parameters Set in the CAD Software on the Marginal and Internal Fitness of Monolithic Zirconia Crowns with Different Luting Agent (A Comparative In vitro Study), J Res Med Dent Sci, 2020, 8(1): 74-80.
Received: 26-Dec-2020 Accepted: 17-Jan-2020