Research - (2020) Volume 8, Issue 1
Evaluation of Implant Stability and Marginal Bone Level of Maxillary Immediate Implants Augmented with Two Different Bone Grafting Materials: A Comparative Study
Husam A Alnuaimy1* and Thair A Hassan2
*Correspondence: Husam A Alnuaimy, Department of Oral and Maxillofacial Surgery, College of Dentistry, University of Baghdad, Iraq, Email:
Abstract
Aim: The aim of this study were to evaluate dental implant stability and marginal bone level after immediate implant placement with simultaneous grafting of the peri-implant gap with either xenograft or alloplastic bone graft.
Materials and methods: Twenty two patients (18 females and 4 males) received 36 immediate dental implants inserted in maxillary fresh extraction sockets, was randomly assigned into two groups with peri-implant gap augmentation with either xenograft (Group A) or alloplastic bone graft (Group B). Implant stability measurements were measured by Periotest M device and marginal bone levels was measured with the aid of othropantomogram radiography, both measurements on immediate postoperative (Baseline) and after a period of six months.
Results: The percentage of change of secondary stability between the two groups was 191.8% reduction of Periotest values scores in group A and 175.7% reduction of scores in group B with no significant difference between them (pË0.05), marginal bone loss in group A was 1.5 mm mesialy and 1.57 mm distally, and for group B the marginal bone loss was 1.71 mm mesialy and 1.47 mm distally with no statistical significant difference between the two groups (pË0.05).
Conclusion: The findings of this study indicated no significant statistical differences in implant stability and marginal bone levels between immediate implants grafted with either type of bone substitutes.
Keywords
Immediate implant, Implant stability, Marginal bone loss, Guided bone regeneration, Xenograft, Alloplastic bone graft
Introduction
The concept of dental implantation throughout the years has gained widespread acceptance and proved to be a reliable and a predictable procedure for replacement of missing teeth, from the first protocol and the innovation of the term osseointegration by different placement and loading protocols have evolved in order to achieve earlier and stress-free surgical episodes, the original placement protocol were to leave the extraction socket to heal for a period up to 6 months. However resorption of the alveolar ridge after tooth extraction may considerably decrease the residual bone volume and prostheticaly driven positioning of the implant, especially in the buccal bundle bone of anterior maxillary area [1-4]. A shortened treatment time between teeth extraction and implant placement as well as a reduction in the amount of surgical episodes is becoming an essential requirement of patients in our daily practice. Therefore, the placement of implants immediately after tooth extraction has been proposed. Several studies advocated that peri-implant gap of less than 2 mm is shown to undergo spontaneous bone regeneration and achieve implant osseointegration however, if the horizontal defect dimension is larger than 2 mm, which ideally should be as immediate implant favorably should be positioned 2 mm from the buccal plate to avoid encroaching on the buccal plate and thereby contributing to resorption [5], the use of a bone grafting material with or without barrier membrane is merited for achieving adequate bone-to implant contact and good osseointegration [6,7]. The use bone substitutes and guided bone regeneration has been advocated to compensate bone resorption and achieve osseointegration around the immediate implants, The principle of guided bone regeneration (GBR) is using barrier membranes, either resorbable or non-resorbable to exclude certain cell types such as rapidly proliferating epithelium and connective tissue thus promoting the growth of slower‐growing cells capable of forming bone [8]. Various bone grafting materials were used to augment the periimplant gap all being Osseo conductive but with different properties of oseoinduction and Osseo genesis as autogenously bone grafts, allografts, xenograft and alloplastic bone substitutes [9,10]. Very few studies compared between those types of bone substitutes in peri-implant gap and to our knowledge no study compared between bovine xenograft bone substitute and alloplastic biphasic tri-calcium phosphate augmented around immediate dental implants in fresh extraction sockets.
Materials and Methods
A total of 22 patients, 18 females and 4 males aged between 25-70 years were enrolled in this study, the patients were randomly assigned into two groups (group A and group B) receiving a total of 36 dental implants (Nucleoss, Turkey) inserted immediately in fresh extraction sockets and the gap between the sockets walls and implants surfaces were filled with xenograft bone grafting material (Bonefill®, Bionnovation®, Brazil) group A., on the other hand an alloplastic bone grafting material (OSTEON™II Collagen, Dentium, Korea) were used for group B. This study was approved by the ethical committee of the College of Dentistry, University of Baghdad and all patients were given detailed information relating to the study aims and an informed consent representing the patient's approval to participate in this study.
Treatment planning
Clinical examination for the evaluation of facial symmetry, smile line and TMJ function. Along with oral hygiene status, periodontal condition and examination of the remaining teeth with attention to the teeth planned to be extracted, space analysis for the proposed implant site was performed to determine the suitability for dental implant placement which included measuring of intercoronal distance and the inter ridge distance using a vernier. A preoperative radiographically examination by orthopantomograms radiograph to evaluate the status of the accused teeth, angulation of the adjacent teeth, length of the root going to be extracted, the available bone height for implant placement, presence of any pathology, and proximity to the vital structures.
Surgical procedure
The surgical procedure was performed under local anesthesia of the planned surgical field with Lidocaine 2% (Septodent) at the site of implant in the maxilla using infiltration technique. Followed by a traumatic extraction and careful curettage of the extraction socket removing any remnants of periodontal ligaments, periapical lesion and granulation tissue followed by extensive irrigation with normal saline solution. A full mucoperiosteal flap was raised to expose the socket walls followed by sequential drilling with copious normal saline irrigation until the final drill according to implant system recommendations using dental engine hand piece set at 800 rpm and torque equal to 35 N/ cm. The implants were inserted by a surgical micro motor hand piece with a torque of 35 N/ cm and speed 35 rpm and finalized seating of the fixture completed manually with screw driver final position as shown in Figure 1. A gingival former is inserted into the fixture and the periotest device was used to measure primary stability as in Figure 2, the cover screw is then engaged in accordance to implant diameter. A collagen membrane were tucked in palatal attached mucosa and bone graft particles after preparation were condensed into the gap and the socket is then covered with collagen membrane as shown in Figure 3, this was followed by approximation of the flap and primary closure utilizing interrupted 3/0 braided black silk sutures. An OPG radiograph is taken at the day of the operation to serve as a baseline data for the marginal bone level.
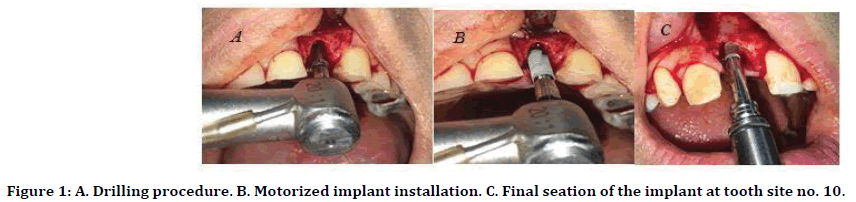
Figure 1. A. Drilling procedure. B. Motorized implant installation. C. Final seation of the implant at tooth site no. 10.
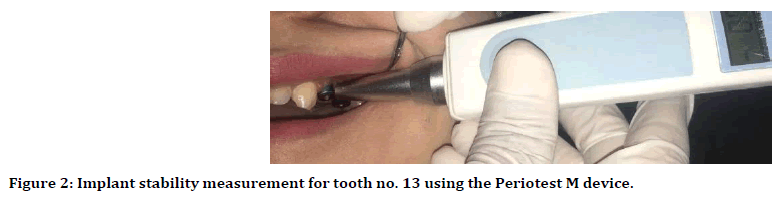
Figure 2. Implant stability measurement for tooth no. 13 using the Periotest M device.
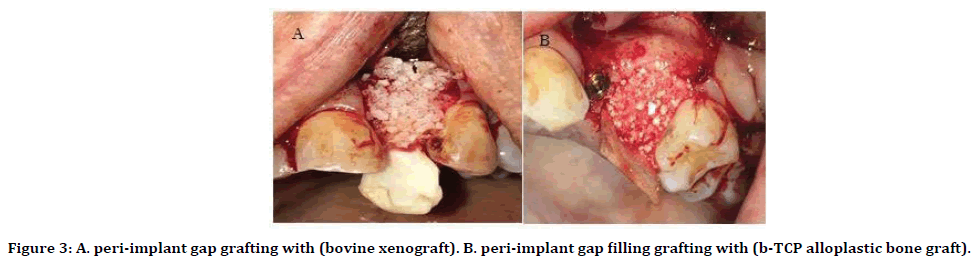
Figure 3. A. peri-implant gap grafting with (bovine xenograft). B. peri-implant gap filling grafting with (b-TCP alloplastic bone graft).
Follow up and data collection
After a period of six months another OPG radiograph is taken to evaluate the marginal bone level in comparison with baseline data using the Image J software as shown in Figure 4 at the same time implant uncovering with an envelope flap and removal of the cover screw, attachment of gingival former and measurements of implant secondary stability is carried with the Periotest M device to be compared with base line data.
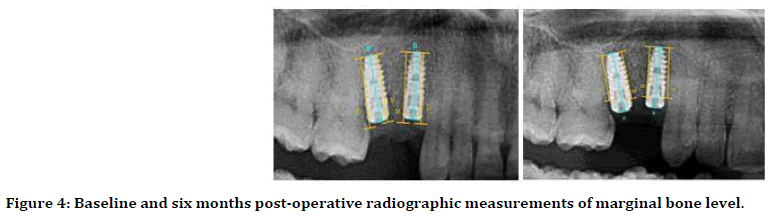
Figure 4. Baseline and six months post-operative radiographic measurements of marginal bone level.
Statiscal analysis
The data analyzed using Statistical Package for Social Sciences (SPSS) version 25. The data presented as mean, standard deviation and ranges. Paired t-test was used to compare the continuous variables between primary and secondary readings.
Results
The total number of patients enrolled in this study were 22 (18 females and 4 males) with mean age of 41 years and standard deviation (SD) of ± 13.5 years of which received a total of 36 immediate implants inserted in fresh extraction sockets of which 34 implants were included in this study with two early implant failures and a survival rate of 94 %. In this study the mean of PTV of the primary stability (ranged from -3.1 to 7.9) was (+2.81 ± 2.7) for group A (xenograft) and (+2.6 ± 3.7) for group B (alloplastic bone graft), while the mean of PTV of secondary stability (ranged from (-5.6 to + 3.0) was (-1.38 ± 2.96) for group A and values of (-1.28 ± 2.62) for group B. Since the periotest values vary greatly between (-8 to + 50) PTV, percentage of change were used to express the change from primary to secondary stability after the period of six months in both test groups, being 191.8 % reduction of PTV scores in group A (Xenograft) and 175.7 % reduction of scores in group B (Alloplastic bone graft) with no significant difference between them (P Value=0.826) as shown in Table 1.
| Type of bone graft | Percentage of change in secondary compared to primary implant stability score Mean ± SD | P-Value |
|---|---|---|
| Xenograft | 191.8 ± 178.0 | 0.826 |
| Alloplast | 175.7 ± 231.6 |
Table 1: Percentage of change of secondary to primary implant stability.
The results of this study demonstrated marginal bone loss in mesial and distal sides around the immediately inserted implants after the healing period of six months, the measurements were established by OPG radiograph with base line data (at time of implant installation) of primary bone level of (13.58 ± 19.3) mm mesialy and (13.16 ± 1.5 ) mm distally and the secondary bone level after the period of six months were (12.08 ± 2.63) mm mesialy and (11.59 ± 2.17) mm distally with for group A (Xenograft bone substitute) While the measurements for group B (alloplastic bone substitute) were Primary bone levels of (14.01 ± 1.2) mm mesialy and (13.97 ± 1. 8) mm distally mm and secondary bone levels of (12.3 ± 2.11) mm mesialy and (12.5 ± 1.77) mm distally for group B. The difference between secondary and primary bone levels represented marginal bone loss which in group A (xenograft) were (1.5) mm mesialy and (1.57) mm distally, for group B (aloplastic bone graft) the marginal bone loss were (1.71) mm mesialy and (1.47) mm distally and a mean. No statistical significant difference (P˃0.05) was found between the two groups as shown in Table 2.
| Type of bone graft | Bone level in relation to implant | Marginal bone resorption (mm) | P - Value | |
|---|---|---|---|---|
| Primary Mean ± SD | Secondary Mean ± SD | |||
| Mesial | ||||
| Xenograft | 13.58 ± 19.3 | 12.08 ± 2.63 | 1.5 | 0.698 |
| Alloplastic | 14.01 ± 1.2 | 12.3 ± 2.11 | 1.71 | |
| Distal | ||||
| Xenograft | 13.16 ± 1.5 | 11.59 ± 2.17 | 1.57 | 0.205 |
| Alloplastic | 13.97 ± 1. 8 | 12.5 ± 1.77 | 1.47 | |
Table 2: Mean marginal bone resorption between the bone graft study groups.
Discussion
While immediate implant placement in fresh extraction socket has proved to be a predictable and unswerving technique for instantaneous replacement of hopeless teeth, the challenge remains for selecting implant diameter that exactly matches the socket alveolar wall in spite of the improvements in surface designs of the fixtures and drilling procedures, clinical studies has revealed that the closer the implant to the buccal wall of the socket the more resorption take place [11]. On the other hand the peri-implant gap dimensions of more than 2 mm has the need for augmentation procedures [12,13], the current study applied two bone substitutes that are most frequently used in bone augmentation procedure. Implant stability measurements has shown improved secondary stability with both types of grafts this is attributed to qualities of the applied bone grafts leading to stabilization and bone formation around the implant thus increasing in the bone implant contact (BIC) which coincide with the results stating values of periotest are decreased when surface area connection are increased [14,15]. Coinciding with other studies establishing that the bone grafting procedure increase bone/implant contact and improve the osseointegration of implants placed in fresh extraction socket [16] in agreement with this study a randomized, controlled clinical trial concluded new bone formation and boneto- implant contact around implants with a sandblasted, acid-etched surface was found to be equivalent between sinuses augmented with βCP or DBB [17]. In addition to implant stability several studies evaluated marginal bone resorption around immediate implants due to the process of active bone remodeling with different bone grafts with after 3,6,12 months, in this study mean marginal bone resorption was up to 1.5 mm coinciding studies reporting up to 1.9 mm of bone loss [18,19] and reporting to be higher than other studies reporting minimum marginal bone loss down to 0.4 mm [20,21] that process with different results ranging from 2 mm to down to a minimum marginal bone resorption of 0.474 mm variations of bone resorption rates may be explained by different measurement and statistical methods in addition to different designs, surface treatment of fixtures and different surgical protocols.
Conclusion
Within the limitations of this study a conclusion can be drawn that bone grafting procedures are valuable for increasing secondary stability obtaining osseointegration with no superior type of bone graft upon the other with both types similarly failing to maintain marginal bone level.
References
- Brånemark PI, Breine U, Adell R, et al. Intra-osseous anchorage of dental prostheses: I. Exp Studies 1969; 3:81-100.
- Van der Weijden F, Dell'Acqua F, Slot DE. Alveolar bone dimensional changes of post‐extraction sockets in humans: A systematic review. J Clin Periodontol 2009; 36:1048-1058.
- Pagni G, Pellegrini G, Giannobile WV, et al. Postextraction alveolar ridge preservation: biological basis and treatments. Int J Dent 2012; 2012:1-13.
- Hansson S, Halldin AJJodb. Alveolar ridge resorption after tooth extraction: A consequence of a fundamental principle of bone physiology. J Dent Biomec 2012; 3:1-17.
- Mehta H, Shah S. Management of buccal gap and resorption of buccal plate in immediate implant placement: A clinical case report. J Int Oral Health 2015; 7:72-82.
- Greenstein G, Cavallaro J. Managing the buccal gap and plate of bone: Immediate dental implant placement. Dent 2013; 32:70-72.
- Caneva M, Salata LA, De Souza SS, et al. Hard tissue formation adjacent to implants of various size and configuration immediately placed into extraction sockets: An experimental study in dogs. Clin Oral Implants Res 2010; 21:885-890.
- Elgali I, Omar O, Dahlin C, et al. Guided bone regeneration: Materials and biological mechanisms revisited. Eur J Oral Sci 2017; 125:315-37.
- Benic GI, Mokti M, Chen CJ, et al. Dimensions of buccal bone and mucosa at immediately placed implants after 7 years: A clinical and cone beam computed tomography study. Clin Oral Implants Res 2012; 23:560-566.
- Jun SH, Park CJ, Hwang SH, et al. The influence of bone graft procedures on primary stability and bone change of implants placed in fresh extraction sockets. Maxillofac Plast Reconstr Surg 2018; 40:8.
- Tomasi C, Sanz M, Cecchinato D, et al. Bone dimensional variations at implants placed in fresh extraction sockets: A multilevel multivariate analysis. Clin Oral Implants Res 2010; 21:30-36.
- Botticelli D, Berglundh T, Buser D, et al. The jumping distance revisited: An experimental study in the dog. Clin Oral Implant Res 2003; 14:35-42.
- Ortega-Martinez J, Perez-Pascual T, Mareque-Bueno S, et al. Immediate implants following tooth extraction. A systematic review. Med Oral Patol Oral Cir Bucal 2012; 17:251-261.
- Kim NS, Vang MS, Yang HS, et al. Comparison of stability in titanium implants with different surface topographies in dogs. J Adv Prosthodont 2009; 1:47-55.
- Hsu JT, Shen YW, Kuo CW, et al. Impacts of 3D bone-to-implant contact and implant diameter on primary stability of dental implant. J Formos Med Assoc 2017; 116:582-590.
- Santos PL, Gulinelli JL, Telles Cda S, et al. Bone substitutes for peri-implant defects of postextraction implants. Int J Biomat 2013; 2013:307136.
- Lindgren C, Sennerby L, Mordenfeld A, et al. Clinical histology of microimplants placed in two different biomaterials. Int J Oral Maxillofac Implants 2009; 24:1093-1100.
- Hafez WK, Hakam MM. Evaluation of marginal bone stability around immediate implants. Clin Implant Dent Related Res 2012; 14:792-807.
- Tadi D, Pinisetti S, Gujjalapudi M, Kakaraparthi S, et al. Evaluation of initial stability and crestal bone loss in immediate implant placement: An in vivo study. J Int Soc Prev Comm Dent 2014; 4:139-144.
- Lindgren C, Mordenfeld A, Hallman. A prospective 1‐year clinical and radiographic study of implants placed after maxillary sinus floor augmentation with synthetic biphasic calcium phosphate or deproteinized bovine bone. Clin Implant Dent Relat Res 2012; 14:41-50.
- Gangar R, Sadhwani BS, Anchlia S, et al. Immediate placement implant in fresh extraction socket: A clinical study of seven cases. Int J Oral Implant Clin Res 2013; 4:7-15.
Author Info
Husam A Alnuaimy1* and Thair A Hassan2
1Department of Oral and Maxillofacial Surgery, College of Dentistry, University of Baghdad, Iraq2Iraqi Scientific Council of Maxillofacial Surgery, Iraqi Board for Medical Specialization, Iraq
Citation: Husam A Alnuaimy, Thair A Hassan, Evaluation of Implant Stability and Marginal Bone Level of Maxillary Immediate Implants Augmented with Two Different Bone Grafting Materials: A Comparative Study, J Res Med Dent Sci, 2020, 8(1):139-143.
Received: 13-Jan-2020 Accepted: 30-Jan-2020
