Research - (2021) Volume 9, Issue 5
Evaluation of MBL Concerning All-on-4 Concept Using two Different Angles
Mohammad A Hameed* and Thair A Hasan
*Correspondence: Mohammad A Hameed, Department of Oral and Maxillofacial Surgery, College of Dentistry,, University of Baghdad, Iraq,
Abstract
Background: The “All-on-4” technique using 4 implants that has gained popularity in full arch edentulism cases in recent years was presented as a modern technique in implant-denture rehabilitation. Crestal bone loss has been postulated to have a multi-factorial etiology and can be considered to occur early or late in the lifetime of a dental implant. Aim: evaluation marginal bone level of dental implant related to all-on-4 concept. Materials and methods: This were a clinical prospective comparative study organized from February 2019 to March 2020 in the College of Dentistry Teaching Hospital, Department of Oral & Maxillofacial Surgery/Dental Implant Unit/ University of Baghdad. A total of 15 Iraqi patients aged 41-73 years, 9 males & 6 females were enrolled in this study receiving 80 dental implants (All-on-4 concept). Patients classified into two groups, group A (All-on-4 with 2 anterior axial and 2 posteriors with angulation of 17°) and group B (All-on-4 with 2 anterior axial and 2 posteriors with angulation of 30°). For both, the surgical site of dental implant was examined for the hard and soft tissues clinically and radiographically utilizing OPG and CBCT. Result: The measurements of the marginal bone level of dental implants reported significant change observed between T1 & T3, while there were no significant changes radiographically in cases between categories. Regarding to gender, the mean of MBL of dental implant in males registered a significant increase in T3 in comparison with T1 (P=0.012). On the other hand, there were non-significant radiographical changes regarding gender at different times. Success rate was 95.24% Conclusion: All-on-4–style full-arch dental implant procedures have one of the highest success rates, the present study showed good clinical outcomes when using All-on-4 concept. MBL had significant changes in both males and females. There was irrelevant clinical analysis result in comparison to the stastical analysis in relation to MBL with different variables.
Keywords
Eosinophil cell density, Oral squamous cell carcinoma, Giemsa stain
Introduction
The “All-on-4” technique using 4 implants that has gained popularity in full arch edentulism cases in recent years was presented as a modern technique in implant-denture rehabilitation by Malo in Lisbon, Portugal, for the first time in 2003 and the all-on-four concept that began to be used in atrophic full arch mandibular and in the maxilla in 2005 has emerged as Figure 1.
Figure 1: Schematic picture of mandibular “All-on-4” [2].
One of the early designs of the “All-on-4” style concept can be traced back to Mattsson, et al. whereby they treated 15 patients (68 implants) with severely resorbed edentulous maxilla by inserting 4 to 6 implants in the premaxilla to avoid sinus augmentation, they reported only one failed implant with 100% prosthesis stability in a 3 to 4.5 year period [1].
Biomechanical advantages of “All-on-4” design [1]
✓ Implants follow a dense bone structure.
✓ Longer implants can be placed by tilting them posteriorly.
✓ Tilting improves A-P spread of implants.
✓ A-P spread enhances load distribution for prosthesis.
✓ Shorten cantilever (maximum of 7 mm for maxilla and 1.5–2.0 _ A-P spread for mandible) reduces prosthetic fracture/ instability and marginal bone height stability.
✓ Marginal bone height of implants is maintained with rigid prosthesis.
✓ Tilted implants have similar success rate as traditional implants when splinted together.
Marginal bone level: Defined as the distance from the first bone implant contact (BIC) to the junction of the roughened micro thread and the smooth, beveled implant surface was determined at the mesial and distal aspect of the implant [3]. Marginal bone loss is evaluated from the radiography; this should not be greater than 1.5 mm in the first year (osteointegration period), and 0.1 mm during each successive year (follow-up period) [4].
When implants are loaded, they are subjected to some degree of micromotion; the displacement of the implant relative to bone generates stress and strain that will result in the local deformation of supporting interfacial tissues [5,6]. Micromotion and the ensuing local tissue deformation can affect bone healing, cause fibrous encapsulation, induce bone resorption, and lead to implant loosening [6,7]. The resorption of marginal bone usually begins from the bone cortex [8].
Crestal bone loss has been postulated to have a multi-factorial etiology [9] and can be considered to occur early or late in the lifetime of a dental implant. Here, early means within the first year after placement and crestal bone loss observed is a consequence of bone remodeling subsequent to surgical and restorative procedures and early loading challenges undertaken by an implant and its associated prosthesis [10,11], the cumulative effect of chronic etiological factors that are immunological (foreign body reaction), environmental, including patient factors such as motivation, smoking, bruxism, and infection/inflammation, and the influence of clinician (surgeon/prosthodontist) may influence late CBL [10,11].
Materials and Methods
Study sample
This was a clinical prospective comparative study organized from February 2019 to March 2020 in the College of Dentistry Teaching Hospital, Department of Oral & Maxillofacial Surgery/Dental Implant Unit/University of Baghdad. A total of 15 Iraqi patients aged 41-73 years, 9 males & 6 females were enrolled in this study receiving 80 DI (All-on-4 concept).
Patients classified into two groups, group A (Allon- 4 with 2 anterior axial and 2 posteriors with angulation of 17°) and group B (All-on-4 with 2 anterior axial and 2 posteriors with angulation of 30°). For both, the surgical site of DI was examined for the hard and soft tissues clinically and radiographically utilizing OPG and CBCT. The total performed implants 80 DI was for both groups, 40 DI for each group.
Inclusion criteria
✓ Patient's ≤18 years with complete jaw edentulism.
✓ Patient was with good general condition or with other diseases that do not influence BHP.
✓ Completely edentulous maxilla and mandible or presence of teeth with an unfavorable long-term prognosis to be extracted.
✓ Adequate available alveolar bone height and width in between premolars regions.
✓ Patients who refused any kind of sinus augmentation procedure when the subantral distance being less than 3 mm and require 2- stage sinus lift procedure in maxilla, also patients refused to undergo any kind of Inferior Alveolar Nerve (IAN) transposition procedure (lateralization) view to insufficient alveolar bone height in the mandible.
Exclusion criteria
✓ Presence of local acute infection at the implant site or any evidence of local pathological conditions in implant zone.
✓ Poor oral hygiene and poor motivation to initiate/maintain good oral hygiene.
✓ Any systemic diseases or condition that influence bone healing.
✓ Anatomical limitation that interferes with performance with this procedure.
✓ Clinical evidence of parafunctional habits.
A preliminary preoperative OPG was taken as a standard radiograph for documentation and assessment of the available alveolar bone height taking in consideration the amount of magnification and important anatomical structures such as (the anterior wall of maxillary sinus, floor of nasal cavity, mandibular canal, and mental foramen), Also, it was important to identify the presence of any pathology in the implant zone and the relation of the proposed DI to the anatomical limitations. CBCT for indicated cases (candidates) was taken to evaluate the available bone of the maxilla and mandible in a 3-dimensions view.
Surgical procedure
Approaches “All-on-4”
In rehabilitation a crestal incision was made from first molar to first molar region with distally bilateral vertical buccal oblique incision, full-thickness mucoperiosteal flap reflection using Molt # 9 and\or Haworth periosteal elevator was performed to locate a bluish hue of maxillary sinus in maxilla and mental foramen in mandible, alveolar osteotomy was made with surgical bur, The ridge crest was trimmed to remove any sharp edges and irregularities using surgical bur and surgical handpiece, After a drilling with a ᴓ 2.4 mm drill to 10-mm depth using a dental engine handpiece set at 800 rpm and torque equal to 35 N/cm, an All-on-4 Guide (Trigonometer, Nucleoss Turkey) was placed in the midline. The contour of the guide should be adjusted so as it follows the opposing arch; this allows implants to be directed against the opposing arch for proper inclination. Starting with the anterior implant sites, drilling with a pilot drill (starter drill) at least 10 mm from the previously midline guide (lateral incisor position) according to jaw size and anatomical variation, sequential drilling until reaching the final size with 0°. The two axially anterior implants were inserted in the anterior region parallel to the midline following the jaw axially to avoid buccal bone plate penetration, Implant placed with 35 rpm speed using motorized way and then finally seated with manual ratchet, Posterior implant position at second premolar position with same technique and insertion torque. The exact location of the anterior wall of maxillary sinus was important to locate and with attention to locate and avoid damaging the mental nerve and neurovascular bundle clinically with direct vision because it allows the posterior implants to be placed angulated distally with either 17°or 30° with respect to the guide.
Raes, et al. [3] in their study utilized two views (coronal & sagittal) in the determination of the marginal bone level change around the fixture. The three-dimensional position of the implant in the dental arch of the patient could be stored by determination of the central point of the apical and coronal part of the implant. Subsequently, the software calculated a three-dimensional rotation and constructed horizontal planes perpendicular to the long axis of the implant and the marginal bone level was measured, Figure 2. The authors mentioned that when thin cortical bone was present adjacent to dental implants, the resolution of the CBCT was insufficient in comparison with light microscopy especially in case of thin buccal bone.
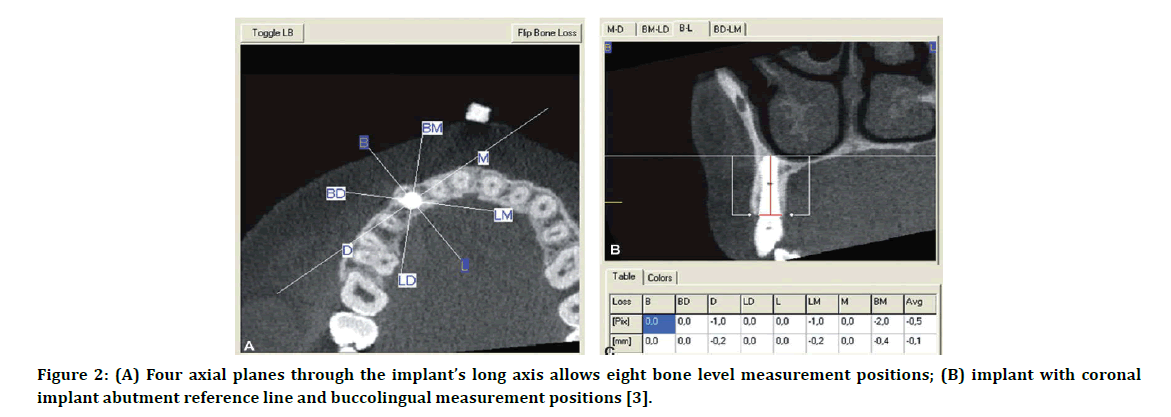
Figure 2: (A) Four axial planes through the implant’s long axis allows eight bone level measurement positions; (B) implant with coronal implant abutment reference line and buccolingual measurement positions [3].
After a discussion with the radiologist about the above-mentioned study to get more accurate results with standardization as possible in this study, the readings were done after the software calculated a three dimensional-rotation about 45ºof the coronal index distally in the axial view. This method indicated that there was an absolute difference in readings found in views with rotation or without rotation as seen in Figure 3.
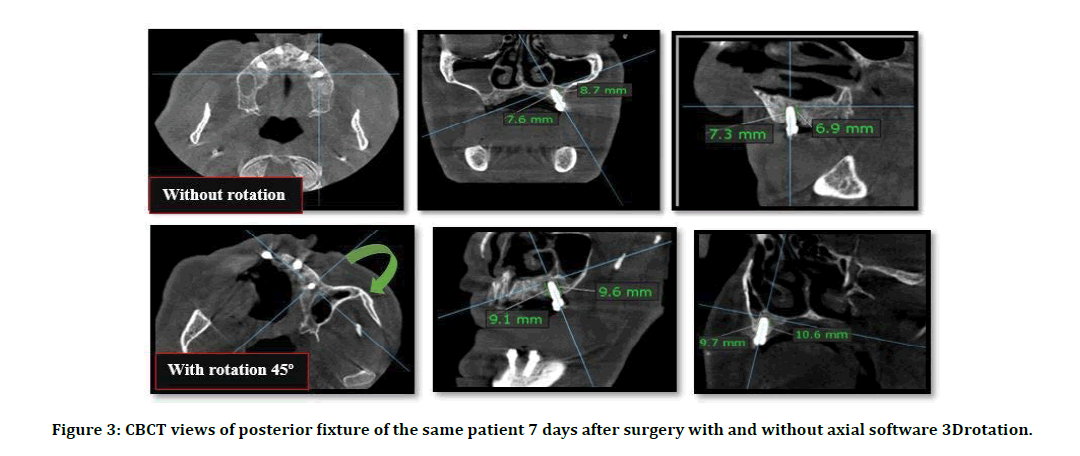
Figure 3: CBCT views of posterior fixture of the same patient 7 days after surgery with and without axial software 3Drotation.
For both groups, the patients were subjected to CBCT examination 7 days after surgery to determine the MBL as baseline data. CBCT is taken again after 12 weeks of healing period and 24 weeks following placement of DI and loading of the prosthesis. The evaluation was made with (KAVO OP 3D; Germany) and field of view (13 × ᴓ15 cm). According to the manufacturer the apparatus provides no distortion. Two views (coronal & sagittal) used in the determination of the marginal bone level change around the fixture. Initially, the three-dimensional position of the implant in the axial view was determined by the allocation of the central point of the implant. The software program calculated a three-dimensional rotation of the coronal index about 45˚ toward the distal side of all fixtures in the axial view. The marginal bone level was evaluated by determining the horizontal plane at the apical part and perpendicular to the long axis of the fixture. This resulted in four circumferential measurements buccomesial, linguomesial, buccodistal, linguodistal from the apical part of the implant to the margin of the crest. The average values of these sides also can be taken to estimate overall bone level change (Figures 4-6).
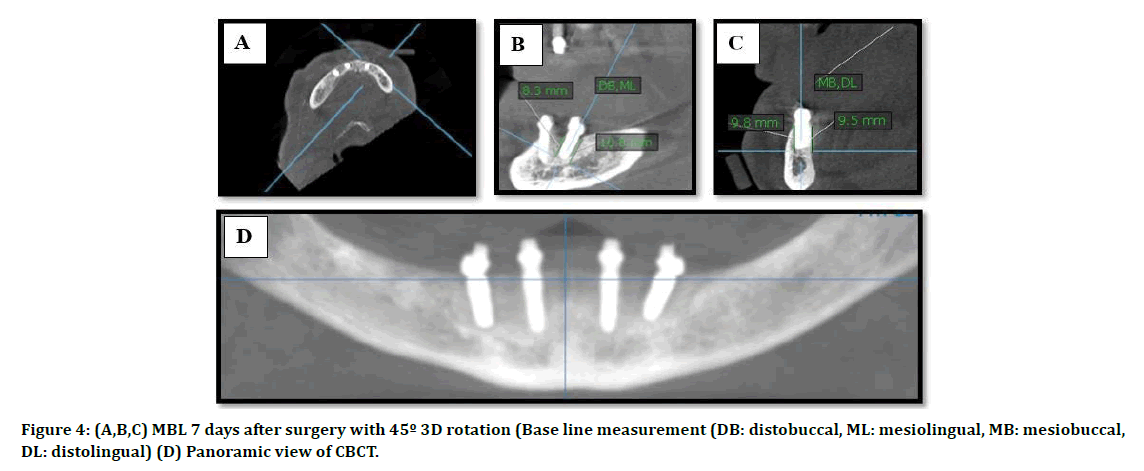
Figure 4: (A,B,C) MBL 7 days after surgery with 45º 3D rotation (Base line measurement (DB: distobuccal, ML: mesiolingual, MB: mesiobuccal, DL: distolingual) (D) Panoramic view of CBCT.
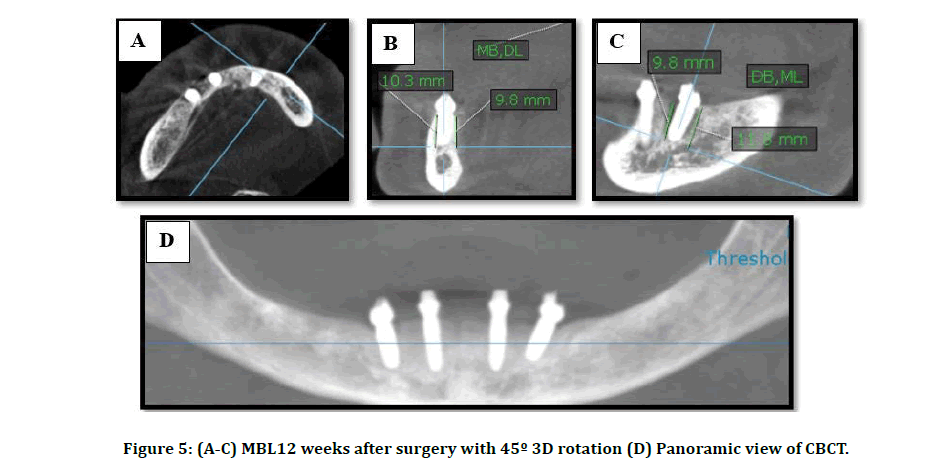
Figure 5: (A-C) MBL12 weeks after surgery with 45º 3D rotation (D) Panoramic view of CBCT.
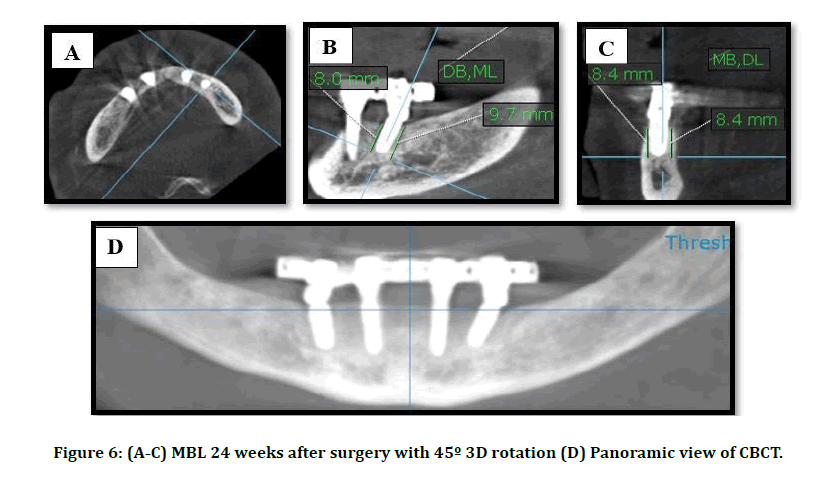
Figure 6: (A-C) MBL 24 weeks after surgery with 45º 3D rotation (D) Panoramic view of CBCT.
Results
Fifteen patients contributed to this study aged from 41-73 years with an average of 59.8 years. The highest percentage (73.3%) was reported >50y as demonstrated. This study included 9 males and 6 females (60% vs 40%) respectively with a male to female ratio of 1.5:1. Eighty-four DI were installed in twenty-one jaws according to All-on-4 concept, one case dropped out after four weeks. Nine male patients (twelve jaws) were contributed in this study with six females (eight jaws) as explained in Figure 7.
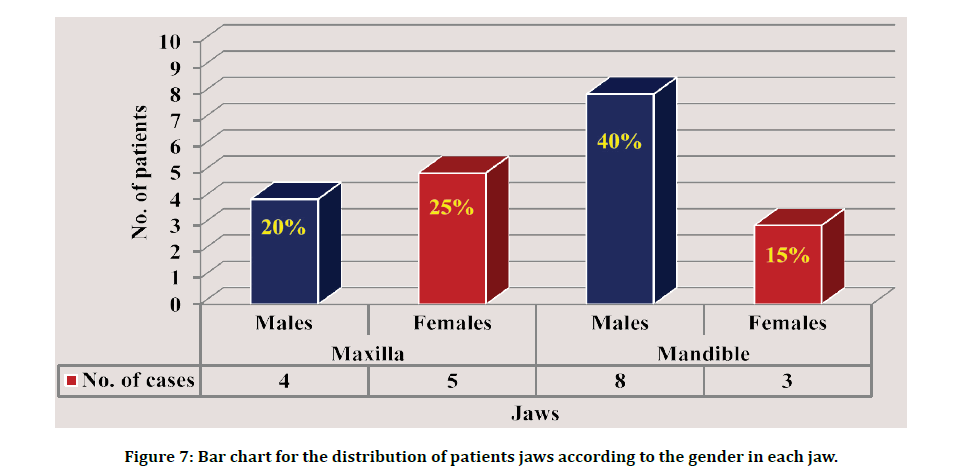
Figure 7: Bar chart for the distribution of patients jaws according to the gender in each jaw.
Effect of time on the MBL of dental implants
The measurements of the marginal bone level of dental implants reported significant change observed between T1 & T3, while there were no significant changes radiographically in cases between categories as presented in table 1 based on classification of Misch, et al. [12].
Table 1: Descriptive statistics and effect of time on the MBL of dental implants.
| Alveolar wall | Time | Descriptive statistics | Time difference | Radiographic analysis | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Difference of MBL | ||||||||||
| No. | Mean | S.D. | Min. | Max. | p-value | Remained | Changed | p-value | ||
| Overall | T1 | 20 | 10.96 | 0.86 | 9.38 | 12.53 | 0.001** | 17 (85%) | 3 (15%) | 1 |
| T3 | 20 | 10.57 | 0.67 | 9.33 | 11.8 | |||||
| Axial | T1 | 20 | 10.95 | 1.11 | 8.41 | 12.53 | 0.009* | 18 (90%) | 2 (10%) | 1 |
| T3 | 20 | 10.58 | 1 | 8.68 | 12.28 | |||||
| Post. | T1 | 20 | 11 | 1.03 | 9.18 | 13.3 | 0.007* | 17 (85%) | 3 (15%) | 1 |
| T3 | 20 | 10.56 | 0.94 | 8.73 | 12.25 | |||||
Correlation of time and gender difference regarding the MBL of dental implants at each region
Regarding to gender, the mean of MBL of DI in males registered a significant increase in T3 in comparison with T1 (P=0.012). On the other hand, there were non-significant radiographical changes regarding gender at different times as illustrated in a Table 2.
Table 2: Time and gender difference regarding the MBL of dental implants at each region.
| Region | Time | Descriptive Statistics | Gender difference | Radiographic analysis | Comparison p-value | |||||||
| Males (No.=12) | Females (No.=8) | Difference of MBL | ||||||||||
| Male | Female | |||||||||||
| Remain | Change | Remain | Change | |||||||||
| Mean | S.D. | Mean | S.D. | p-value | 11 (92%) | 1 (8%) | 6 (75%) | 2 (25%) | 1 | |||
| Overall | T1 | 11.05 | 0.83 | 10.82 | 0.94 | 0.578 | ||||||
| T3 | 10.71 | 0.67 | 10.29 | 0.52 | 0.143 | |||||||
| Time difference | t-test | 2.98 | 2.39 | |||||||||
| p-value | 0.012* | 0.048* | ||||||||||
| Axial | T1 | 11.33 | 0.69 | 10.36 | 1.41 | 0.053 | 12 (100%) | 0 (0%) | 6(75%) | 2 (25%) | 1 | |
| T3 | 10.98 | 0.69 | 9.99 | 1.13 | 0.025* | |||||||
| Time difference | t-test | 3.62 | 1.31 | |||||||||
| p-value | 0.004** | 0.231 | ||||||||||
| Angled | T1 | 10.81 | 1.18 | 11.28 | 0.73 | 0.337 | 11 (92%) | 1 (8%) | 6 (75%) | 2 (25%) | 1 | |
| T3 | 10.54 | 1.01 | 10.59 | 0.91 | 0.905 | |||||||
| Time difference | t-test | 2.39 | 2.19 | |||||||||
| p-value | 0.035* | 0.064 | ||||||||||
Angle difference in the posterior region regarding the MBL of dental implants
Table 3 demonstrate there was a significant change in statistical analysis (P=0.024) between angles and there were no clinical differences in the comparison between DI angles at different time.
Table 3: Relation of DI angle to MBL.
| Time | Descriptive Statistics | Angle difference | ||||
|---|---|---|---|---|---|---|
| 17º (No.=10) | 30º (No.=10) | |||||
| Mean | S.D. | Mean | S.D. | p-value | ||
| T1 | 10.95 | 1.08 | 11.05 | 1.02 | 0.84 | |
| T3 | 10.64 | 0.75 | 10.47 | 1.14 | 0.705 | |
| Time | t-test | 2.72 | 2.13 | |||
| difference | p-value | 0.024* | 0.062 | |||
| Radiographic analysis | remain | 9 (90%) | 8 (80%) | |||
| Change | 1 (10%) | 2 (20%) | ||||
| Comparison (McNemar test) p-value | 1 | 1 | ||||
Correlation of time and jaw differences regarding the MBL of dental implants at each time
The mean of MBL around DI in the mandibular jaw was significantly increased at T3 than T1 (10.50 VS 10.99) (P=0.007), from the other side, there was no significant difference in maxilla at time difference as described in Table 4.
Table 4: Relation of time and jaw differences regarding the MBL of dental implants at each time.
| Region | Time | Descriptive Statistics | Jaw difference | ||||
|---|---|---|---|---|---|---|---|
| Maxilla (No.=9) | Mandible (No.=11) | ||||||
| Mean | S.D. | Mean | S.D. | p-value | |||
| Overall | T1 | 10.92 | 0.96 | 10.99 | 0.81 | 0.86 | |
| T3 | 10.6 | 0.74 | 10.5 | 0.57 | 0.747 | ||
| Time | t-test | 1.68 | 3.35 | ||||
| difference | p-value | 0.1 | 0.007* | ||||
| Radiographic analysis | Remain | 8 (89%) | 9 (82%) | ||||
| change | 1 (11%) | 2 (18%) | |||||
| Comparison (McNemar test) p-value | 1 | 1 | |||||
| Axial | T1 | 10.8 | 1.6 | 11.07 | 0.52 | 0.603 | |
| T3 | 10.59 | 1.35 | 10.58 | 0.66 | 0.993 | ||
| Time difference | t-test | 1.24 | 2.3978 | ||||
| p-value | 0.249 | 0.019 | |||||
| Radiographic analysis | Remain | 8 (89%) | 10 (91%) | ||||
| change | 1 (11%) | 1 (9%) | |||||
| Comparison (McNemar test) p-value | 1 | 1 | |||||
| Angled | T1 | 11.04 | 0.62 | 10.97 | 1.3 | 0.889 | |
| T3 | 10.61 | 0.91 | 10.51 | 1.01 | 0.823 | ||
| Time difference | t-test | 1.48 | 3.31 | ||||
| p-value | 0.178 | 0.008 | |||||
| Radiographic analysis | Remain | 8 (89%) | 1 (11%) | ||||
| Change | 9 (82%) | 2 (18%) | |||||
| Comparison (McNemar test) p-value | 1 | 1 | |||||
Relation of time and age difference regarding the MBL of dental implants at each region
Regarding the gender, the MBL was significantly increased around dental implant in patients >50y to patients ≤ 50y (P=0.003) at different time, not only but also, the axial and angled DI in age >50y. Showed significant change in MBL at different time (P=0.003 & 0.013) respectively as explained in a table 5.
Table 5: Association of time and age difference regarding the MBL of dental implants at each region.
| Region | Time | Descriptive Statistics | Age difference | ||||
|---|---|---|---|---|---|---|---|
| ≤50 (No.=4) | >50 (No.=16) | ||||||
| Mean | S.D. | Mean | S.D. | p-value | |||
| Overall | T1 | 10.6 | 0.89 | 11.04 | 0.85 | 0.372 | |
| T3 | 10.18 | 0.52 | 10.63 | 0.64 | 0.21 | ||
| Time difference | t-test | 1.19 | 3.6 | ||||
| p-value | 0.318 | 0.003** | |||||
| Radiographic analysis | Remain | 3 (75%) | 14 (87%) | ||||
| change | 1 (25%) | 2 (13%) | |||||
| Comparison (McNemar test) p-value | 1 | 1 | |||||
| Axial | T1 | 10.14 | 1.3 | 11.15 | 1.01 | 0.107 | |
| T3 | 9.55 | 0.51 | 10.84 | 0.92 | 0.016* | ||
| Time difference | t-test | 1.05 | 3.59 | ||||
| p-value | 0.371 | 0.003** | |||||
| Radiographic analysis | Remain | 2 (50%) | 16 (100%) | ||||
| change | 2 (50%) | 0 (0%) | |||||
| Comparison (McNemar test) p-value | 1 | 1 | |||||
| Angled | T1 | 11.07 | 0.6 | 10.98 | 1.12 | 0.89 | |
| T3 | 10.83 | 0.61 | 10.49 | 1.01 | 0.535 | ||
| Time difference | t-test | 1.22 | 2.81 | ||||
| p-value | 0.309 | 0.013* | |||||
| Radiographic analysis | Remain | 4 (100%) | 13 (81%) | ||||
| Change | 0 (0%) | 3 (19%) | |||||
| Comparison (McNemar test) p-value | 1 | 1 | |||||
Discussion
There was a significant decrease (P= 0.001) in the level of crestal bone at the 3rd measurement in patients treated according to the all-on-4 implants concept in overall DI with mean difference of (-0.39 mm), this may be due to bone reaction to surgical trauma, implant design and occlusal load resulting from long spans created between fixtures of all on 4 prosthesis. This is enforced by Hassan, et al. [13] who claimed that all on four group showed a significant higher bone loss than All on 6 group after 6 and 12 months. This could be attributed to several reasons; the long spans created by the all-on-4 prosthesis compared to short spans created by all on 6 ones make the prosthesis more susceptible to deformation and bending during occlusal forces. Thus, higher stresses are transmitted to the implants and could be responsible for increasing bone loss. On the other side, all on 6 creates stiffer framework, which is less susceptible to deformation. Moreover, the presence of cantilever even it was short (first molar only) may transmit increased overload for implant-support system, especially the distal implants.
Wu, et al. [14] in their vivo study stated that cantilever loading had a large effect on the bone stress and strain around dental implants in allon- four treatment. Higher bone stress and strain might increase the risk of bone overloading and the stress and strain in the surrounding bone in all-on-4 treatment with four Osseo integrated dental implants was not markedly influenced by the implant design.
This in agreement with Krennmair, et al. [15] who advocated that with 148/176 implants (37 patients, drop-out: 15%) followed for 3 years reported a significant (p < 0.001) annual differences of MBL alterations over time.
Babbush, et al. [16] in their study, one hundred sixty-nine patients (n=856 implants) stated that the mean marginal bone loss noted from baseline to the follow-up was 0.14 ± 0.59 mm (P =0.001). The duration of follow-up had no effect on the degree of marginal bone loss (P=0.154). There was no effect on the extent of marginal bone loss.
In the present study, the 2nd readings of the bone level were significantly decreased in regarding to males and >50y patients, this may be due to heavy biting force in males than females in addition to the most of males neglect oral health care and loss their teeth as consequence to the progressive periodontal disease that may result in early teeth loss.
These explanations are approved by Werbelow, et al. [17] who mentioned, that among the older patient group, leading to higher prevalence of peri-implantitis and MBL than female this approved by many studies report a higher risk for peri-implant bone loss in these patients; however, the long-term survival rate does not significantly differ mentioned by
In recent study, there was a significant decrease in MBL in the mandible with mean difference of (-0.49mm) compared to high resorption rate of maxilla (-0.32mm) this may be contributed to poor oral hygiene noticed by researcher which may be increased incidence of periimplantitis and consequently MBL, this disagrees with Browaeys, et al. [18] who found no statistically significant differences between both jaws (p=0.278).
Considering DI angles relation to the maxilla, the study presented a non-significant loss of the marginal bone in both axial and angled implants with the mean difference (-0.21 &-0.43) mm, this may be contributed to enthusiastic instruct the patients to clean the area beneath the prosthesis and the use of soft diet and in addition to that all four implants connected by metal bar, so the force distribute equally and reduce occlusal force. This is in the same line with the study of Sthita, et al. [19] who claimed that the mean marginal bone loss was 0.46mm in the mandible and 0.09 mm in the maxilla seen below the implant abutment interface. The marginal bone loss is higher in this study for tilted implants was 0.37 mm as compared to the axial implants 0.27 mm, the marginal bone loss around tilted implants was higher and was statistically significant (p=0.539>0.05).
These results are not in accordance with study of Werbelow, et al. [17] on 23 patients and the restoration of 170 dental implants in 32 edentulous jaws. They stated that the angulation of the implants had no influence on radiographic bone loss. Hopp, et al. [20] advocated in their study, that the marginal bone loss at 5 years follow up be not significantly affected by the implant orientation (axial/tilted) in the maxillary bone this is not in same line with recent result of research. The present study in cross line with Browaeys, et al. [18] who performed a multivariate analysis (mixed-model) to examine differences in bone loss between implants in the upper and lower jaw and between straight and tilted implants and showed that bone loss was not significantly different between straight and tilted implants (p=0.605) after 3 years.
Radiographical analysis of MBL
Success (optimum health): < 2 mm radiographic bone loss from initial surgery.
Satisfactory survival: 2–4 mm radiographic bone loss.
Compromised survival: Radiographic bone loss >4 mm (less than 1/2 of implant body).
Failure (clinical or absolute failure)
Radiographic bone loss >1/2 length of in this respect, the radiographical analysis presented in this research is the first performed to report crestal bone loss data 24 weeks after implant restoration using a flap surgical technique. In the one hand, the stastical analysis registered significant changes in MBL in relation to different variables like: Total DI in relation to time, gender, mandible and to patient's age >50 y (P=0.001, M=0.012 & F= 0.048, 0.007 & 0.003) respectively. These result in contrast from the radiographic point of view that demonstrated no significant changes in relation to the previous variables (P=1).
On the other hand, some statically analysis that recorded non-significant changes in relation to different variables like axial and angled DI in relation to females (P= 0.231& 0.064), angled30º DI (0.062), total DI in maxilla (P= 0.100) & overall DI in patients ≤50 y (P= 0.318), these noted in accordance with radiographic analysis that presented with non-significant changes (P=1) for all previously mentioned variables respectively.
Conclusion
All-on-4–style full-arch dental implant procedures have one of the highest success rates of any treatment in dental treatments; the technique is also among the most difficult and can be fraught with obstacles. The present study showed good clinical outcomes when using two tilted and two axial implants and a fixed prosthesis for rehabilitation of the edentulous ridges. Survival rate if DI was 95.24% and patients benefited from the use of the All-on-4 treatment concept. However, unacceptable ongoing bone loss may be a warning sign of future problems and needs clinical attention. Overloading and surgery-related aspects need to be further experience as possible as much. MBL had significant changes in both males and females. There was irrelevant clinical analysis result in comparison to the statistical analysis in relation to stability and MBL with different variables.
References
- Chan MH, Holmes C. Contemporary “All-on-4” concept. Dent Clin 2015; 59:421-470.
- Weir D. Implant treatment planning for the edentulous patient: A graftless approach to immediate loading. Nature Publishing Group 2011.
- Raes F, Renckens L, Aps J, et al. Reliability of circumferential bone level assessment around single implants in healed ridges and extraction sockets using cone beam CT. Clin Implant Dent Related Res 2013; 15:661-672.
- Boronat A, Peñarrocha M, Carrillo C, et al. Marginal bone loss in dental implants subjected to early loading (6 to 8 weeks postplacement) with a retrospective short-term follow-up. J Oral Maxillofac Surg 2008; 66:246-250.
- Haiat G, Wang HL, Brunski J. Effects of biomechanical properties of the bone–implant interface on dental implant stability: From in silico approaches to the patient's mouth. Annual Review Biomed Eng 2014; 16:187-213.
- De Barros e Lima Bueno R, Dias AP, Poncea KJ, et al. Bone healing response in cyclically loaded implants: comparing zero, one, and two loading sessions per day. 2018; 85:152-161.
- Wazen RM, Currey JA, Guo H, et al. Micromotion-induced strain fields influence early stages of repair at bone–implant interfaces. Acta Biomater 2013; 9:6663-6674.
- Liu Y, Wang J. Influences of microgap and micromotion of implant–abutment interface on marginal bone loss around implant neck. Arch Oral Biol 2017; 83:153-160.
- Bryant SR. Oral implant outcomes predicted by age-and site-specific aspects of bone condition: National Library of Canada 2001.
- Linkevicius T, Puisys A, Vindasiute E, et al. Does residual cement around implant‐supported restorations cause peri‐implant disease? A retrospective case analysis. Clin Oral Implant Res 2013; 24:1179-1184.
- Naveau A, Shinmyouzu K, Moore C, et al. Etiology and measurement of peri-implant crestal bone loss (CBL). J Clin Med 2019; 8:166.
- Misch CE, Perel ML, Wang HL, et al. Implant success, survival, and failure: The International Congress of Oral Implantologists (ICOI) Pisa consensus conference. Implant Dent 2008; 17:5-15.
- Hassan SSM, Emarah AAEBM. All on 4 versus all on 6 implant concepts for rehabilitation of edentulous maxilla. Short term randomized clinical and radiographic study. Egyptian Dent J 2020; 66:659-670.
- Wu AYJ, Hsu JT, Fuh LJ, et al. Biomechanical effect of implant design on four implants supporting mandibular full-arch fixed dentures: In vitro test and finite element analysis. J Formosan Med Assoc 2020; 119:1514-1523.
- Krennmair S, Weinländer M, Forstner T, et al. Factors affecting peri‐implant bone resorption in four Implant supported mandibular full‐arch restorations: A 3‐year prospective study. J Clin Periodont 2016; 43:92-101.
- Babbush CA, Kanawati A, Kotsakis GA. Marginal bone stability around tapered, platform-shifted implants placed with an immediately loaded four-implant-supported fixed prosthetic concept: A cohort study. Int J Oral Maxillofac Implant 2016; 31.
- Werbelow L, Weiss M, Schramm A. Long-term follow-up of full-arch immediate implant-supported restorations in edentulous jaws: A clinical study. Int J Implant Dent 2020; 6:1-8.
- Browaeys H, Dierens M, Ruyffelaert C, et al. Ongoing crestal bone loss around implants subjected to computer‐guided flapless surgery and immediate loading using the All‐on‐4® concept. Clin Implant Dent Related Res 2015; 17:831-843.
- Sthita Gurrala VD, Francis Akkara. All-on-4 dental implant concept in immediate rehabilitation of failing dentition–A prospective study to evaluate the efficacy and cost effectiveness in Indian population. J Dent Health Oral Disorder Therapy 2020; 11:12-16.
- Hopp M, de Araújo Nobre M, Maló P. Comparison of marginal bone loss and implant success between axial and tilted implants in maxillary all‐on‐4 treatment concept rehabilitations after 5 years of follow‐up. Clin Implant Dent Related Res 2017; 19:849-859.
Author Info
Mohammad A Hameed* and Thair A Hasan
1Department of Oral and Maxillofacial Surgery, College of Dentistry,, University of Baghdad, IraqCitation: Sundus Abdul-Alhussain Jasim, Shorouq M Abass, Effect of Alum Disinfectant Solutions on Some Properties of a Heat-Cured Acrylic Resin, J Res Med Dent Sci, 2021, 9 (5):132-139.
Received: 27-Apr-2021 Accepted: 18-May-2021 Published: 31-May-2021
