Research - (2022) Volume 10, Issue 5
Evaluation of Palatal Bone Thickness and Density for the Assessment of the Site of Orthodontic Mini Screw Utilizing CBCT for Iraqi Arabic Population
Muntadher Shafeeq Hadi1* and Nidhal H Ghaib2
*Correspondence: Muntadher Shafeeq Hadi, Department of Orthodontics, College of Dentistry, University of Baghdad, Baghdad, Iraq, Email:
Abstract
Introduction: Ensuring adequate anchorage is often challenging in orthodontics because many of the various methods developed for reinforcing anchorage depend on patient compliance. The introduction of skeletal anchorage with mini screw implants, which is widely used in orthodontic treatments for expanding the boundary of tooth movement and has no patient compliance requirements. Many factors should be kept in mind when choosing the placement sites like soft tissue anatomy, inter radicular distance, sinus morphology, nerve location and buccolingual bone depth. Adequate bone at mini-implant placement site can influence the success or failure of anchorage. Hence, it is imperative to measure the thickness of the bone. The palatal area considered as the best anchorage site in the maxilla because it composed of dense cortical bone, also the hard and soft tissue guarantees the biomechanical stability for placement mini screw. Aim of study: Is to evaluate palatal bone thickness and density for mini screw placement and the effect of gender on palatal bone thickness and density using CBCT. Materials and method: The sample consisted of 60 CBCT scans from the database of patient of both genders with an age range of 18 to 24 years were included in the study. The Cone beam CT images of all the subjects will be taken from the database patients using a KaVo OP 3D CBCT unit. Mid palatal suture and incisive foramen will be used as sagittal and axial reference guide, respectively.
Result and Discussion: In this study, the palatal bone thickness based on data from 60 young adult subjects (30 male and 30 female), shows that palatal bone thickness ranges from (1.6 to 8.8 mm) with mean of (5.4mm) for male and (4.44 mm) for female, while the palatal bone density ranges from (260 to 510 HU) with mean of (340 HU) for male and (405 HU) for female. Conclusion: There is gradual decrease of bone thickness from anterior part of palate to the posterior. The bone thickness and density are significantly high at the anterior part of the mid palatal suture.
Keywords
Cone beam computed tomography, Bone thickness, Bone density, Mini-implant, Hounsfield unit (HU)
Introduction
The key for successful orthodontic treatment is based on anchorage control, which can be define as unwanted movement of anchor teeth and usually occurs when the posterior teeth move forward relative to the anterior teeth [1, 2]. In recent years, the introduction of skeletal anchorage with miniscrew implants, which is widely used in orthodontic treatments for expanding the boundary of tooth movement and has no patient compliance requirements [3]. They are routinely used in orthodontic practice because of their numerous advantages, including their low cost and simple surgical placement and removal [4]. Many factors should be kept in mind when choosing the placement sites likewise soft tissue anatomy, inter radicular distance, sinus morphology, nerve location, buccolingual bone depth [5]. Due to their small and convenient size of the miniscrew implant enables their use in many anatomical sites such as the retromolar area in the mandible, the buccal cortical plate in both the maxilla and the mandible [6, 7]. The palatal area considered as the best anchorage site in the maxilla because it composed of dense cortical bone, also the hard and soft tissue guarantees the biomechanical stability for placement mini screw [8, 9]. Bone quality and quantity play important roles in the success of mini-implants since stability is achieved by mechanical retention rather than by osseointegration as well as the thickness, type and health of the soft tissue [10]. Cortical bone thickness of less than 0.5mm is not suitable for mini screw placement, higher success rate has been reported with cortical bone at least 1.0mm thick [11]. Mini screw in the maxilla has less stability than in the mandible because of its porous nature [8]. The palate has become a popular site for inserting TADs because of its easy access, lack of vital structures, adequate keratinized tissue and low risk of root injury. Mid sagittal area of palate is a safe location for mini screw due to sufficient bone height provided by the nasal crest and thin keratinized soft tissue [12]. Because of the different growth pattern noted between a male and female, patient’s age and gender should be considered in the decision for the optimal implant site especially mid palatal region which mainly depend on patient maturation so this region should be avoided for adolescent patient because the palatal thickness was significantly lower in mixed dentition than in late mixed and permanent dentition for this reason, mid palatal implant have a high failure rate for adolescent due inadequate ossification [13]. A significant difference occurs in anteroposterior and mediolateral areas in the early mixed dentition, late mixed and permanent dentition [14]. Cone beam computed tomography (CBCT), a three-dimensional imaging modality, was reported to provide highly accurate and detailed image, permit the dental professional to visualize image in slices from any angle in any part of the image region and archived digitally what the conventional radiograph never showed [15]. So CBCT is an ideal modality for measuring palatal bone thickness and can be utilized for locating the ideal site for placement of orthodontic miniimplant [16].
Material and Methods
The sample consisted of 60 CBCT scans from the database of the Iraqi Arabic patients (30 males and 30 females) with their age range was between 18-24 years, this retrospective study carried out at university of Baghdad college of dentistry department of oral surgery and Ghazy Alhariri hospital\maxillofacial department during the period from September 2019 to February 2021.
The CBCT images of all the subjects were taken using a KaVo OP 3D CBCT unit (Figure 1). The images were reconstructed with OnDemand3D software which has an inbuilt measurement tool to measure total palatal bone thickness and density.
Figure 1: On demand 3D dental Imaging System (version 1.0.10.746).
Out of 200 CBCT scans that were taken from the data base only 60 scans were compatible with included criteria that will be mentioned later. the samples were divided into two main group according to the gender (30 scans for male and 30 scans for female) and each group was divided into two groups according to the side (15 scans for right side and 15 scans for left side). Specific criteria were considered in the selection of the sample depending on case sheet at the oral surgery and maxillofacial department to get more information about medical history of the patients, presence of systemic disease that effect bone health such as diabetes mellitus, hypertension and hormonal disorders. Patients with full erupted of permanent teeth with no missing teeth (excluding the third molars), no pathologic lesions or abnormalities of the maxilla, no radiographic signs of periapical disease, no syndromes of cleft palate, and no pathological lesion in the palate, which determined by radiographic examination (CBCT) of each subject, were included in this study, while patients who had palataly positioned impacted tooth, blurred or unclear image were excluded from the study.
Method
After selection of the CBCT scan from the database of patient depending on the inclusion criteria, at first locating the incisive foramen which is the reference anatomic landmark for anteroposterior points, and then locating the mid palatal suture which represent the land mark for the mediolateral points (figure 2 and figure 3).
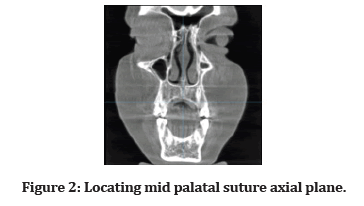
Figure 2:Locating mid palatal suture axial plane.
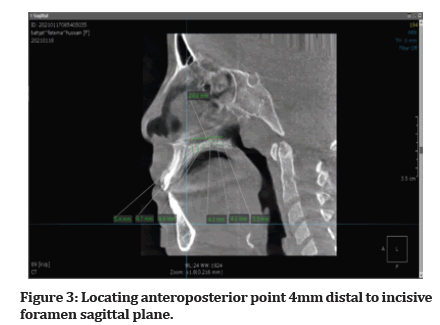
Figure 3:Locating anteroposterior point 4mm distal to incisive foramen sagittal plane.
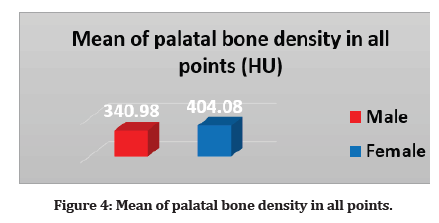
Figure 4:Mean of palatal bone density in all points.
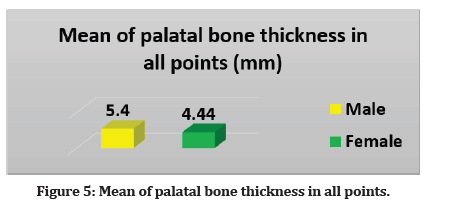
Figure 5:Mean of palatal bone thickness in all points.
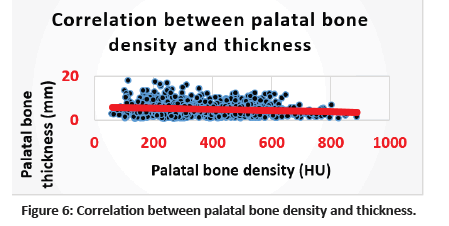
Figure 6:Correlation between palatal bone density and thickness.
A 4mm distal to the incisive represent the first point of the anteroposterior points and the measurement of thickness and density continue posteriorly for each 4mm till point 24 mm near the molars area this measurement was done at the mid palatal suture (the 0 point of the mediolateral points) and was repeated at 6mm and 12mm from the mid palatal suture. The ondemand software has a built-in measurement tool that used in the measurement of bone thickness and density. The measurements of palatal bone density were made in each point defined previously using the Hounsfield unit (HU) equivalent pixel intensity value scale in the software program.
Results
The total number of study patients was 60 (30 males and 30 females). All of them were underwent CBCT scans to evaluate the effect of gender on palatal bone thickness and density. The data analyzed using Statistical Package for Social Sciences (SPSS) version 26. The data presented as mean, standard deviation and ranges. Categorical data presented by frequencies and percentages. Independent t-test (two tailed) was used to compare the continuous variables according gender. Pearson’s correlation test (r) was used to assess correlation between palatal bone density and thickness. A level of P – value less than 0.05 was considered significant.
Comparison in palatal bone density according gender
Considering palatal bone density, mean of palatal bone density in male in all point 340.98 (SD ± 161.5), while mean of palatal bone density in female 404.08 (SD ± 166.3); Table 1 and Figure 4 statistically, a significant difference in female was found compared to that in male.
| Palatal bone density (HU) | Gender | P - Value | |
|---|---|---|---|
| Male Mean ± SD | Female Mean ± SD | ||
| 340.98 ± 161.5 | 404.08 ± 166.3 | 0.001 | |
Table 1: Mean of palatal bone density in all points.
Comparison in Palatal Bone Thickness According Gender
Regarding thickness of palatal bone in all points according gender. Mean of palatal bone thickness in male was 5.4mm (SD ± 3.1) while in female 4.44 mm (SD ± 2.6) as shown in Table 2 and Figure 5 there is a significant difference in males compared to that in females.
| Palatal bone thickness (mm) | Gender | P - Value | |
|---|---|---|---|
| Male Mean ± SD | Female Mean ± SD | ||
| 5.4 ± 3.1 | 4.44 ± 2.6 | 0.001 | |
Table 2: Mean of palatal bone thickness in all points.
Correlation between palatal bone density and thickness
Correlation between palatal bone density and thickness is shown in Table 3 and Figure 6. Statistically significant negative correlation was detected between palatal bone density and thickness (r= - 0.151, P= 0.001).
| Palatal bone thickness (mm) | Palatal bone density (HU) | |
|---|---|---|
| r | P - Value | |
| -0.151 | 0.001 | |
Table 3: Correlation between palatal bone density and thickness.
Discussion
Thickness Differences
In the present study, the palatal bone thickness based on data from 60 young adult subjects (30 males and 30 females) according to the specific criteria of the sample shows that palatal bone thickness ranges from (1.6 to 8.8 mm) with mean of (5.4mm) for male and (4.44 mm) for female. It’s found that the highest thickness at median and paramedian regions 4mm from the incisive foramen, followed by area at 8mm from the incisive foramen. The palatal bone thickness is the least at 24mm posterior to the incisive foramen. The palatal bone thickness reduced considerably from the anterior to the posterior region of the palate. The present results are in line with [17, 18] both studies evaluate the palatal bone thickness for placement of mini-implant using CBCT, and similar to [19] who found that the highest palatal bone thickness in the lateral anterior palate [20, 21]. Reported more palatal bone thickness in male than female which similar to this study finding.
Density Differences The present study, based on data from 60 young adult subjects (30 males and 30 females), shows that palatal bone density ranges from (260 to 510 HU) with mean of (340 HU) for male and (405 HU) for female. Bone density varies between subjects and sites. Our results indicated that the area of high density in cortical bone extended 16 mm posterior to the incisive foramen in the mid palatal suture of the measured area and 6 mm in the laterally to the palatal suture. These are in line with [22] who reported that the most suitable area for implant placement in the palate was located 4 to 12 mm posterior to the incisive foramen and 3 to 6 mm paramedian to the suture [23]. Concluded that the density of the mid palatal suture was high enough to support mini-implants. He also suggested that the reported 10% failure rate of micro-implants inserted in the palatal area may be due to other factors than bone density.
Side Differences
In the present study there is no difference in bone density and thickness between right and left side of the palatal bone and this finding is in line with [24].
Conclusion
The palatal bone thickness was higher in the anterior part of the palate (between the canine and first premolar), so there are chances that bone to mini-implant contact area will be more; thus, primary stability of the mini-implant will be more. However, at the same time, the palatal bone density is highest in between the canine and first premolar area, thus will require higher torque for the insertion of mini-implants.
Funding
There was no funding association with this work.
Availability of Data and Materials
All data analyzed during this study are included in this published article.
Authors' Contributions
All authors of this study have read and approved the manuscript.
Financial Support and Sponsorship
Nil.
Declaration of Conflicting Interests
All authors declare that there are no commercial associations that might create a conflict of interest in connection with the submitted manuscripts.
References
- Mallat Z, Corbaz A, Scoazec A, et al. Interleukin-18/interleukin-18 binding protein signaling modulates atherosclerotic lesion development and stability. Circ Res 2001; 89:e41-5.
- Wehrbein H, Merz BR, Diedrich P. Palatal bone support for orthodontic implant anchorage-a clinical and radiological study. Eur J Orthod 1999; 21:65-70.
- Moe SM, Chen NX. Mechanisms of vascular calcification in chronic kidney disease. J Am Soc Nephrol 2008; 19:213-6.
- Park CL, Helgeson VS. Introduction to the special section: growth following highly stressful life events--current status and future directions. J Consult Clin Psychol 2006; 74:791.
- Carano A, Velo S, Incorvati C, et al. Clinical applications of the Mini-Screw-Anchorage-System (MAS) in the maxillary alveolar bone. Prog Orthod 2004; 5:212-35.
- Poggio PM, Incorvati C, Velo S, et al. “Safe zones”: a guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod 2006; 76:191-7.
- Wu L, Gao Y, Liu J, et al. Event-triggered sliding mode control of stochastic systems via output feedback. Automatica 2017; 82:79-92.
- Stoughton C, Lupton RH, Bernardi M, et al. Sloan digital sky survey: early data release. Astron J 2002; 123:485.
- Chang HP, Tseng YC. Miniscrew implant applications in contemporary orthodontics. Kaohsiung J Med Sci 2014; 30:111-5.
- Moon JE, Park YJ, Ryu JH, et al. Initial validation of GOCI water products against in situ data collected around Korean peninsula for 2010–2011. Ocean Sci J 2012; 47:261-77.
- Motoyoshi I, Nishida SY, Sharan L, et al. Image statistics and the perception of surface qualities. Nature 2007; 447:206-9.
- Ryu K, Lee HR, Kim WG. The influence of the quality of the physical environment, food, and service on restaurant image, customer perceived value, customer satisfaction, and behavioral intentions. Int J Contemp Hosp Manag 2012.
- Gracco A, Lombardo L, Cozzani M, et al. Quantitative evaluation with CBCT of palatal bone thickness in growing patients. Prog Orthod 2006; 7:164-74.
- Freitas AO, Marquezan M, Nojima MD, et al. The influence of orthodontic fixed appliances on the oral microbiota: a systematic review. Dental Press J Orthod 2014; 19:46-55.
- Garib DG, Yatabe MS, Ozawa TO, et al. Alveolar bone morphology under the perspective of the computed tomography: defining the biological limits of tooth movement. Dental Press J Orthod 2010; 15:192-205.
- Warrier CU, Babu MP, Manjula P, et al. Isotopic characterization of dual monsoon precipitation–evidence from Kerala, India. Curr Sci 2010: 1487-95.
- King TS, Chinchilli VM, Wang KL, et al. A class of repeated measures concordance correlation coefficients. J Biopharm Stat 2007; 17:653-72.
- Bonangi R, Kamath G, Srivathsa HS, et al. Utility of CBCT for the measurement of palatal bone thickness. J Stomatol Oral Maxillofac Surg 2018; 119:196-8.
- Manimegalai S, Manjula P. Thermodynamic and adsorption studies for corrosion inhibition of mild steel in aqueous media by Sargasam swartzii (brown algae). J Mater Environ Sci 2015; 6:1629-37.
- Ching YC, Rahman A, Ching KY, et al. Preparation and characterization of polyvinyl alcohol-based composite reinforced with nanocellulose and nanosilica. BioResources 2015;10:3364-77.
- Franz M, Lopes CT, Huck G, et al. Cytoscape. js: a graph theory library for visualisation and analysis. Bioinformatics 2016; 32:309-11.
- Bernhart T, Vollgruber A, Gahleitner A, et al. Alternative to the median region of the palate for placement of an orthodontic implant. Clin Oral Implants Res 2000; 11:595-601.
- Jung BA, Kunkel M, Göllner P, et al. Success rate of second-generation palatal implants: preliminary results of a prospective study. Angle Orthod 2009; 79:85-90.
- Park J, Park J, Jang S, et al. FTFD: an informatics pipeline supporting phylogenomic analysis of fungal transcription factors. Bioinformatics 2008;24: 1024-5.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Muntadher Shafeeq Hadi1* and Nidhal H Ghaib2
1Department of Orthodontics, College of Dentistry, University of Baghdad, Baghdad, Iraq2Department of Dentistry, AL-Israa university college, Iraq
Citation: Sangiya K, C Naveen Kumar, Phytochemical Analysis, Evaluation of Palatal Bone Thickness and Density for the Assessment of the Site of Orthodontic Mini Screw Utilizing CBCT for Iraqi Arabic Population, J Res Med Dent Sci, 2022, 10 (5):83-87.
Received: 02-May-2022, Manuscript No. JRMDS-22-62391; , Pre QC No. JRMDS-22-62391 (PQ; Editor assigned: 04-May-2022, Pre QC No. JRMDS-22-62391 (PQ; Reviewed: 18-May-2022, QC No. JRMDS-22-62391; Revised: 23-May-2022, Manuscript No. JRMDS-22-62391 (R); Published: 30-May-2022
