Research - (2022) Volume 10, Issue 11
Evaluation of periodontal health status in patients undergoing fixed orthodontic treatment. A systematic review
Suhael Ahmed1*, Suha Basuhail2, Hadeel Basuhail2, Ghadeer Aldhafeeri2, Reem Jamaan Alghamdi2, Rana Ahmad Alaqel2, Suhailah Basuhail2 and Munirah Mohammed Alsuwaidan2
*Correspondence: Suhael Ahmed, Department of Oral and Mxillofacial surgery and Diagnostic Sciences, Riyadh Elm University, Riyadh, Saudi Arabia, Email:
Abstract
Background: The transmission of orthodontic forces through the stressed tissue matrix onto the local cells within the periodontal ligament and alveolar bone, stimulate the cells to release proinflammatory, angiogenic and osteogenic agents that activates the process of periodontal ligament and alveolar bone remodeling. Studies have suggested that orthodontic therapy when not fully controlled may influence the process of inflammation and the destruction of periodontium leading to increased loss of attachment. Objective: To evaluate updated scientific evidence on the relationship between fixed orthodontic therapy and periodontal health. Methods: A systematic literature search was performed using the Pubmed and other databases with keywords “orthodontic” and “periodontal” based on PRISMA 2020 guidelines. Articles published from January 2000 to September 2022 were included. The studies that satisfied the inclusion criteria were evaluated and classified as having low, moderate, or high methodology quality. Results: 12 articles were selected from a total of 864 searched articles after assessing the quality using cochrane ROB 2 assessment tool. Conclusions: The present systematic analysis suggests that there is moderate scientific evidence that a fixed appliance influences periodontal status; no article reported a high score.
Keywords
Orthodontic therapy, Periodontal status, Fixed appliance, Systematic review, Orthodontics effects
Introduction
The relationship between orthodontic procedures and periodontal status is considered a challenge, especially periodontal health during and after orthodontic treatment. Several studies have addressed the impact of fixed, removable, and myofunctional orthodontic/ orthopaedic appliances or retainers in relation to supragingival plaque accumulation and gingivitis. These supragingival conditions are reversible a few months after appliance removal in patients with a good standard of oral hygiene. Multiple studies have suggested that orthodontic treatment not only provides dental esthetics but has a strong psychosocial impact on patients as well [1]. Adult orthodontic patients having severe bone loss presents a continued challenge to clinicians. Healthy periodontium is usually associated with well-aligned dentition than crowded and maloccluded teeth. Studies believe that when orthodontic appliances are applied correctly the forces will not damage the periodontium surrounding it. Orthodontic appliances can also support the periodontal tightening and splinting where oral hygiene is present [2].
Gingival inflammation occur when there is a significant accumulation of plaque, thus leading to gingivitis (plaque-induced) which may manifest several patterns with visible signs and symptoms of inflammation that are localized in the gingiva, such as bleeding and edema, if left untreated it can progress to periodontitis which is characterized by the loss of supporting and surrounding bone [3]. Even if the dental plaque biofilm levels decreased, inflammatory infiltrates will still be available within the gingival tissues presented as a part of the physiologic immune system [4]. Bacteria present in plaque secrete multiple compounds such as antigens, toxins, and enzymes, which influence the initiation of an inflammatory response that is protective in nature but is also responsible for breakdown of periodontium, increase pocket depth and loss of teeth [5]. Inadequate and non-consistent oral hygiene activities such as tooth brushing and flossing, influence the accumulation of dental biofilms, which consequently relates for the initiation and progression of periodontal diseases. This indicates the importance of oral hygiene role in the prevention of periodontal diseases. Multiple research projects of experimental and clinical trials have agreed that periodontal health necessitates an efficient removal of dental plaque [6,7]. It is very important to maintain high-level of oral hygiene at home and adequate visits for professional cleaning during and after the completion of orthodontic therapy [8].
The transmission of orthodontic forces through the stressed tissue matrix onto the local cells within the periodontal ligament and alveolar bone, stimulate the cells to release proinflammatory, angiogenic and osteogenic agents that activates the process of periodontal ligament and alveolar bone remodeling [9]. Studies have suggested that orthodontic therapy when not fully controlled may influence the process of inflammation and the destruction of periodontium leading to increased loss of attachment [10]. A study explained that the orthodontic movement synergies with periodontal disease in influencing the breakdown through increasing the levels of proinflammatory cytokines [11]. Clear aligner therapy (removable orthodontic treatment) has been introduced into adult orthodontics recently, several advantages have been found including improved aesthetic results [12]. It constitutes clear plastic splints that cover all teeth and the marginal aspects of the gingiva which gradually move the teeth into an ideal arrangement. Multiple studies have also reported that periodontal health is not affected by this treatment modality, mainly due to its removable application not affecting the oral hygiene levels [12].
The interlinked relationship existing between periodontal tissues and tooth movement processes suggest that orthodontic treatment has an important impact in overcoming associated problems, but if movement became excessive beyond the anatomic boundaries of the alveolar process then it will further contribute in the destruction of the periodontium [13]. This study aims to systematically review available studies in literature that are concerned about the relationship between fixed orthodontic treatment and periodontal health.
Aim
To evaluate updated scientific evidence on the relationship between fixed orthodontic therapy and periodontal health.
Materials and Methods
Study inclusion and exclusion criteria
Following the PRISMA 2020 flowchart, articles were first excluded according to the title and abstract; if titles were not written in English language or were irrelevant to the scope of the review. Screening of full texts were done according to eligibility criteria. Studies included were randomized control trial, clinical trial; prospective and retrospective, an observational study; either cohort or case-control study, cross-sectional study, patients needed an orthodontic appliances or have undergone orthodontic treatment; either fixed orthodontic appliance or Invisalign system (removable orthodontic appliance) were outcomes have been compared, clinical findings were correlated with underlying cause if it was due to mechanical or microbiological activity. According to the exclusion criteria, studies of irrelevant topics and that are not related to the review topic either due to use of different orthodontic appliance or that haven’t correlated the relationship between orthodontic treatment and periodontal health, studies not written in English language nor full text is available, case reports, case series, systematic reviews, meta-analysis, literature reviews were excluded.
Search strategies
Databases have been searched to answer the focus question of this review, “Is the periodontal health of patients who have undergone orthodontic treatment affected by the fixed appliances?”. The electronic databases that were searched included: Medline/ PubMed, Cochrane Library, Scielo, Web of Science, and Scopus from January 2000 until 15 September 2022. Keywords used to identify relevant articles included: orthodontics, orthodontic treatment, fixed orthodontic treatment, fixed orthodontic appliance, periodontics, periodontal health, periodontium. PRISMA 2020 statement and flow diagram were used to select the articles. Total of 12 articles were identified after excluding duplicates (Table 1).
| Criteria | Determinants |
|---|---|
| Population | The patients that have undergone or will undergo orthodontic treatment with fixed appliances |
| Intervention | Fixed orthodontic treatment |
| Comparison | Comparison of orthodontic treatment other than fixed appliance |
| Outcome | Periodontal changes associated with fixed orthodontic treatment |
Table 1: PICO table to determine eligibility of research question.
Data extraction
Data from the selected study including author name, year of publication, article aim, demographics, included groups (study and control) mean age and number of participants if applicable, the process of study conduction, study outcomes relating fixed orthodontic appliance and periodontal health and conclusion were retrieved and summarized in Table 2.
| Literature | Research Design | Research Purpose | Subject | Result | Conclusions |
|---|---|---|---|---|---|
| Sheibaninia, et al. [14] | Case control | To evaluate the correlation between the use of fixed orthodontic appliances and periodontal conditions. | 60 female participants. Mean age of 15 years. Two groups: Study group; undergoing orthodontic treatment (n=30) Control group; not undergoing orthodontic treatment (n=30) |
Gingival bleeding; 50% in the control group, 76.7% in the study group (P<0.3). Gingival recession; 3.3% in the control group, 0% in the study group (P<0.9). Gingival hyperplasia. 13.3% in the control group, 46.4% in the study group (P<0.005). |
Fixed orthodontic appliances rise the probability of experiencing gingival bleeding and Hyperplasia. |
| Gomes, et al. [15] | Case control | To evaluate periodontal conditions in individuals who had undergone orthodontic treatment with fixed appliances. |
54 (23 males, 31 females) participants. Mean age of 23 years Two groups: Study group; underwent orthodontic treatment (n=29) Control group; not undergone orthodontic treatment (n=25) |
Visible plaque index, gingival bleeding index, bleeding on probing; Not significant between the groups. Periodontal probing depth; Not significant between the groups. Significant for canines. Clinical attachment loss; Not significant between groups. Significant for canines. |
The use of orthodontic appliances is not certainly related to aggravating periodontal problems. |
| Jiao, et al. [16] | Retrospective cohort study | To evaluate if periodontal status in patients with stage IV/grade C periodontitis was affected after fixed orthodontic treatment. | 24 (8 males, 16 females) participants. Age not considered. Individuals included: patients with stage IV/grade C periodontitis that received combined periodontal and orthodontic treatments. |
The only clinical parameter with statistically significant improvement was bleeding on probing. Probing depth, bleeding on probing, percentage of relative bone height; no change was detected after orthodontic treatment. |
Periodontal stability can be obtained for patients with stage IV/grade C periodontitis after orthodontic treatment. |
| Calniceanu, et a. [17] | Clinical trial | To assess specific site-level changes that occurred due to orthodontic forces in adult patients with severe periodontal disease that underwent standard periodontal therapy. |
13 (5 males, 8 females) participants. Mean age of 36 years Individuals included: patients previously treated for severe generalized periodontitis were given fixed orthodontic appliances. |
Clinical nor microflora parameters showed significant differences in the between baseline and 6 months of orthodontic treatment. | The presence of periopathogens doesn’t negatively affect periodontal health during orthodontic treatment in adult patients treated for severe periodontitis. |
| Salvesen, et al. [18] | Retrospective cohort study | To evaluate the periodontal status in patients undergoing orthodontic retention control and possible risk indicators. | 211 (96 males, 115 females) participants. Mean age of 21 years Individuals included: patients who underwent orthodontic retention control between three to ten years after orthodontic treatment |
Periodontal parameters were within the limits of healthy periodontium clinically. Fixed retainers and older age are the only variables that were significantly associated with increased calculus. |
Long-term fixed retainers have no harmful effect on the periodontium alone. Additional factors may increase the risk of plaque deposits and increased probing pocket depths. |
| Madariaga, et al. [19] | Clinical trial | To evaluate the periodontal health of orthodontic patients with supportive periodontal therapy in a 3-month follow-up |
40 (14 males, 26 females) participants. Mean age of 28 years Two groups: Fixed group: patients ongoing multibracket fixed therapy (n=20) Clear aligners group; patients in treatment with clear aligners (n=20) |
Statistically significant decrease in both groups was found for pocket depth, bleeding on probing and plaque index. No significant difference based on type of appliance used. |
Patients undergoing orthodontic treatment with fixed appliances and clear aligners did not show differences in gingival health when followed by a dental hygienist. |
| Levrini, et al. [20] | Clinical trial | To compare the periodontal health and the microbiological changes in patients treated with fixed orthodontic appliances and Invisalign system. | 77 (25 males, 52 females) participants. Mean age of 24.3 years Three groups: Invisalign group (n=32) Fixed orthodontic appliances group (n=35) Control group (n=10) |
The Invisalign group showed superior results in terms of periodontal health and total biofilm mass compared to the fixed orthodontic appliance group. | Patients undergoing orthodontic treatment with the Invisalign System show better periodontal health when compared to patients in treatment with fixed orthodontic appliances. |
| Liu, et al. [21] | Clinical trial | To examine periodontal changes and the relative quantity of subgingival Porphyromonas gingivalis during orthodontic treatment. | 48 (13 males, 35 females) participants. Mean age of 17 years Two groups: Group A; patients who were at the beginning of orthodontic treatment (n=28) Group B; patients who were at the completion of orthodontic treatment (n=20) |
There was a significant increase in Plaque and gingival index during the first 3 months of appliance placement but a significant decrease in Plaque index, gingival index, and probing pocket depth during the first 6 months after appliance removal. Subgingival P. gingivalis were high at the end of orthodontic treatment, and they decreased significantly after appliance removal. |
Fixed orthodontic treatment is conducive to dental plaque accumulation and gingival inflammation., it may imply a potential risk to periodontal health in certain patients. |
| Liu, et al. [21] |
Clinical trial | To evaluate and compare the microbiological and periodontal changes occurring in adolescents during orthodontic therapy with removable and fixed appliances. |
50 participants. Aged 10-18 years Two groups: Group 1; treated with Invisalign aligners (n=25) Group 2; treated with fixed orthodontic appliances (n=25) |
None of the patients was positive for the periodontal anaerobes analyzed. The plaque index, probing depth and bleeding on probing were significantly lower in the group treated with Invisalign than in the group treated with fixed brackets. Compliance with oral hygiene was significantly higher in the group treated with Invisalign than in the group treated with fixed brackets. |
Teenagers treated with Invisalign aligners display better compliance with oral hygiene, less plaque, and fewer gingival inflammatory reactions than their patients treated with fixed appliances. |
| Corbett, et al. [22] | Observational cross-sectional | To compare the periodontal health of maxillary and mandibular anterior teeth retained with two types of fixed retainers. | 74 (30 males, 44 females) participants. Mean age of 17 years Two groups: Group 1; treated with a straight twisted wire retainer (n=35) Group 2; treated with a wave-type retainer (n=39) |
There was no significant difference between the two retainer groups regarding plaque index, gingival crevicular fluid volume, calculus index, recession, bleeding on probing, and pocket probing depths. | No clinical difference was found in the periodontal health of anterior teeth retained with a SR or WR for a period of 2 to 4 years. |
| Al-Moghrabi, et al. [23] | Randomized control trial | To compare the stability of treatment and periodontal health with fixed vs removable orthodontic retainers over a 4-year period |
42 (10 males, 32 females) participants. Mean age of 21 years Two groups: FR group; treated with fixed retainers(n=21) VFR group; treated with vacuum-formed retainers (n=21) |
Both groups showed similar periodontal outcomes with significant gingival inflammation and plaque levels. | Fixed retention offers the potential benefit of improved preservation of alignment of the mandibular labial segment in the long term. However, both types of retainers were associated with gingival inflammation and elevated plaque scores. |
| Gastel, et al. [24] | longitudinal, prospective | To monitor patients' microbiological and clinical parameters from bracket placement to 3 months after treatment. | 24 (10 males, 14 females) participants. Mean age of 15 years sub- and supragingival microbes periodontal probing depth (PPD), bleeding on probing (BOP), and gingival crevicular fluid (GCF) flow were assessed at baseline (T1), at bracket removal (T2), and 3 months post-treatment (T3). |
Sub- and supragingival colony-forming units ratio decreased significantly at T2 compared with T1. Clinical parameters PPD, POB, and GCF flow showed a significant increase between T1 and T2. Between T2 and T3 these variables decreased significantly but remained significantly higher than at T1 [except for BOP values at the bonded sites (P = 0.0646)]. |
Placement of fixed orthodontic appliances has an influence both on microbial and clinical periodontal parameters, which were only partly normalized, 3 months following the removal of the appliances. |
Table 2: Summarized data of the 12s included studies.
Quality and risk of bias assessment of selected studies
Risk of bias and quality assessment was done using Cochrane ROB 2 risk of bias assessment tool for the selected articles. Domains assessed included: bias arising from randomization process, bias due to deviations from the intended interventions, bias due to missing outcome data, bias in measurement of the outcome and bias in selection of the reported results. According to the risk of bias tool used, included studies could receive a maximum score of nine which indicates the methodological quality, thus indicates the risk of bias. Studies scored 7–9 points were considered being a low risk of bias article; 5–6 points were considered medium-level risk of bias article and those scored less than five points were considered high risk of bias. Of the included 12 articles in this review, 2 were of high risk, one had some concerns and 9 had low risk of bias (Table 3). The randomized control trials, retrospective studies, methodological quality assessment was conducted using the modified Newcastle-Ottawa scale, which covered 3 aspects, patient selection, comparability between study groups and assessment of the outcome.
| Authors | D1 | D2 | D3 | D4 | D5 | Overall |
|---|---|---|---|---|---|---|
| Jiao, et al. [16] | Description: Icon Description automatically generated |
Description: Badge Unfollow with solid fill | Description: Badge Follow with solid fill | |||
| Calniceanu, et al. [17] | Description: Badge Follow with solid fill | Description: Badge Follow with solid fill | Description: Badge Unfollow with solid fill | Description: Badge Follow with solid fill | Description: Icon Description automatically generated |
Description: Icon Description automatically generated |
| Gomes, et al. [15] | Description: Badge Unfollow with solid fill | Description: Badge Follow with solid fill | Description: Badge Follow with solid fill | Description: A picture containing shape Description automatically generated |
||
| Salvesen, et al. [18] | Description: Badge Unfollow with solid fill | Description: Badge Follow with solid fill | Description: Badge Question Mark with solid fill | Description: Badge Unfollow with solid fill | Description: Icon Description automatically generated |
Description: Icon Description automatically generated |
| Sheibaninia, et al. [14] | Description: Badge Follow with solid fill | Description: Badge Follow with solid fill | Description: Badge Follow with solid fill | Description: Badge Question Mark with solid fill | Description: Icon Description automatically generated |
Description: Icon Description automatically generated |
| Liu, et al. [21] | Description: Badge Question Mark with solid fill | Description: Badge Follow with solid fill | Description: Badge Unfollow with solid fill | Description: Badge Follow with solid fill | Description: Icon Description automatically generated |
Description: Icon Description automatically generated |
| Gastel, et al. [24] | Description: Badge Question Mark with solid fill | Description: Badge Follow with solid fill | Description: Icon Description automatically generated |
Description: Badge Question Mark with solid fill | ||
| Levrini, et al. [20] | Description: Badge Follow with solid fill | Description: Badge Follow with solid fill | Description: Badge Unfollow with solid fill | Description: Badge Follow with solid fill | Description: A picture containing shape Description automatically generated |
Description: Icon Description automatically generated |
| Abbate, et al. [25] | Description: Badge Follow with solid fill | Description: Badge Follow with solid fill | Description: Badge Follow with solid fill | Description: Badge Follow with solid fill | Description: Icon Description automatically generated |
|
| Al-Moghrabi, et al. [23] | Description: Badge Follow with solid fill | Description: Badge Follow with solid fill | Description: Icon Description automatically generated |
Description: A picture containing shape Description automatically generated |
Description: Icon Description automatically generated |
Description: Icon Description automatically generated |
| Madariaga, et al. [19] | Description: Badge Follow with solid fill | Description: Badge Follow with solid fill | Description: Icon Description automatically generated |
Description: Icon Description automatically generated |
Description: Icon Description automatically generated |
|
| Corbett, et al. [22] | Description: Icon Description automatically generated |
Description: Icon Description automatically generated |
Description: Icon Description automatically generated |
Description: A picture containing shape Description automatically generated |
Description: Icon Description automatically generated |
Table 3: Risk of bias assessment with the recommended approach of Cochrane ROB 2.
Results
Flow diagram
In this systematic review authors followed the PRISMA 2020 flow diagram as represented in Figure 1. In the identification stage, 864 articles were found in the initial search with 523 articles from Medline, 122 articles from PubMed, 113 articles from web of science and 106 from Scopus. Duplicates found simultaneously between multiple databases were removed. In the screening stage, articles were removed according to the titles and abstract summaries, a total of 12 articles remained after elimination. Further removal was done after reading the whole articles and relating them with the inclusion and exclusion criteria. In this systematic review 12 articles were selected, and all were assessed for risk of bias.
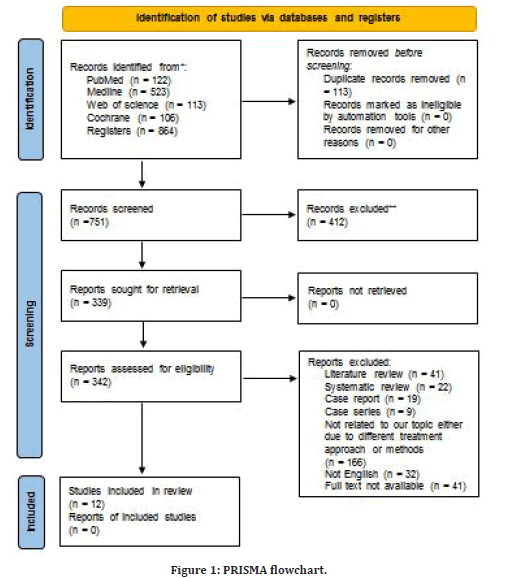
Figure 1: PRISMA flowchart.
Study characteristics
Most studies included in this systematic review were clinical trials, their sample sizes ranged from as low as 13 in the study by Calniceanu, et al. [17] to as high as 77 in studies by Levrini, et al. [20]. While case control studies had a sample size of about 55 patients [14,15]. Both randomized control trials included about 40 patients [23,25]. The Retrospective cohort studies had major differences in sample sizes, ranging from as low as 24 [16] to as high as 211 [18]. One of the included studies was an observational cross-sectional study and included 74 patients [22]. Another study was a longitudinal prospective study, which included 24 patients [24].
Within the twelve studies included, only three studies considered a control group to compare with study group which used fixed orthodontic appliances, where number of participants was comparable between groups [14,15,20]. Five studies compared between two groups such as: A group undergoing fixed orthodontic treatment and a group treated with Invisalign system [19,23,25] or comparing two types of fixed appliances [22] or according to the stage of treatment [21]. Four studies consisted of studying only one group that have undergone orthodontic treatment [16], Calniceanu, et al. [17,18,24].
In six studies, quantity of male and female participants were comparable [15-18,19,22,24] One study only included females [14]. There was no information reported regarding distribution of males and females in one study [25].
Participants mean age was comparable which mostly included younger individuals ranging from 10 years old [25] to 36 years old [17]. In a study conducted by Jiao, et al. [18] age of participants was not considered [16].
All included studies in this review investigated the relationship between fixed orthodontic treatment and periodontal health. In various aspects. Two studies evaluated its effect on periodontally compromised patients with severe periodontitis [16,17]. Two studies correlated the relationship with use of fixed orthodontic appliances compared to healthy individuals [14,15]. Four studies looked into both clinical and microbiological aspects of the relationship existing between fixed orthodontic treatment and periodontal conditions [20,21,24,25]. One study only compared between removable and fixed retainers [23]. One study compared between two types of fixed retainers [22]. One study correlated the relation of fixed orthodontic treatment and periodontal health with oral hygiene level and one study reviewed the possible risk factors associated with the proposed relation [18].
Discussion
Two of the articles included in this review studied the effect of orthodontic treatment on pathologically involved periodontium, whether patient has periodontitis or previously had periodontitis and have been treated. This topic has been discussed in multiple studies, as for a successful orthodontic treatment the base which the periodontium should be healthy to give such results, so the relationship has an effect both ways. Jiao, et al. [16] evaluated periodontal status after orthodontic treatment on patients with stage IV/grade C periodontitis. Study reported that there was no change detected on bleeding on probing, probing depth nor percentage of relative bone height after fixed orthodontic treatment. There were several predisposing factors that led to decrease in bone height including, being a female, excessive horizontal and vertical overlap, crowding, initial probing depth and bone height. The study concluded that periodontal stability in periodontally compromised patients with periodontitis stage IV/grade C, can be obtained after orthodontic treatment [16,17] it evaluated the changes that occur at specific sites within the periodontium due to orthodontic treatment in patients who had periodontitis and been treated. The study reported that there were no significant differences in both clinical and microflora parameters between baseline and after 6 months of orthodontic treatment. The study concluded that pathogens associated with periodontal disease don’t harmfully affect the periodontium that have previously undergone periodontic therapy by the forces exerted by orthodontic treatment [17]. Evidence based studies suggest that fixed orthodontic treatment can be safely and satisfactorily executed if adequate oral hygiene is maintained even if previous disease was present [26]. A recent randomized control trial by Gehlot, et al. [27] emphasized that orthodontic treatment doesn’t significantly affect the periodontium after periodontal stabilization have been achieved [27].
Two articles discussed the relationship between fixed orthodontic treatments on periodontal health. Gomes et al. [15] evaluated the periodontal changes associated with orthodontic treatment. The study reported that plaque and bleeding indices, pocket depth and clinical attachment loss were not significantly different between patients that have undergone orthodontic treatment and who didn’t. The study concluded that orthodontic treatment doesn’t have an effect jeopardizing the periodontium [15]. Salvesena, et al. [18] evaluated the periodontal status of patients undergoing orthodontic treatment and any risk indicator associated. The study reported that measured clinical parameters were within the healthy periodontium limits. Some of the risk indicators include, older age and fixed orthodontic appliance were significantly associated with calculus formation, thus increasing probability of inflammation. The study concluded fixed orthodontic treatment doesn’t harmfully affect the periodontium alone, but there are predisposing factors such as increased plaque accumulation and pocket depth [18]. Both studies revealed that there is no association between orthodontic therapy and harmful effect on the periodontium. Previous systematic reviews confirmed that fixed orthodontic treatment generally does not have harmful effects on periodontal tissues when a good oral hygiene is maintained [28].
Three articles discussed the inflammatory impact of fixed orthodontic treatment on the periodontal health. Sheibaninia et al. evaluated the correlation between use of fixed orthodontic appliances and periodontal conditions. The study reported that gingival bleeding and hyperplasia were higher in study group compared to control group, while gingival recession was higher in control group. The study concluded fixed orthodontic therapy will increase the probability of patients experiencing gingival bleeding and hyperplasia [14]. Liu et al. evaluated the periodontal changes and quantity of P. gingival is during orthodontic treatment. The study proposed that there was significant increase in plaque and bleeding index during first 3 months of fixed orthodontic placement. There was significant decrease in plaque and bleeding indices and pocket depth during the first 6 months after removal of fixed orthodontic appliance. As for bacterial count, P. number of gingival is was higher at the end of the treatment and have decreased significantly after orthodontic appliance removal. The study concluded that fixed orthodontic treatment increase dental plaque accumulation and inflammation, thus can be a causative factor compromising gingival health in some patients [21]. Gastel et al. [24] evaluated changes that occur due to orthodontic treatment from bracket placement to 3 months within treatment, both clinical and microbiological parameters. The study reported that microbiological colonies decreased after bracket removal compared to beginning of treatment. The various clinical parameters (pocket depth, bleeding on probing, gingival crevicular fluid flow etc.) significantly increased from brackets time of placement to removal. The study concluded that fixed orthodontic treatment have an impact on both microbes and clinical findings, it would minor become normal after 3 months of removal [24]. Plaque has been reported to be the most provoking factor for initiation, progression, and recurrence of periodontal inflammation and diseases. After placement of a fixed orthodontic appliences most patients experience minimal amount of gingival inflammation [29]. The resulted gingival inflammation surrounding the fixed orthodontic bands usually leads to pseudo-pockets, which regress within weeks after the band removal of the brackets [30].
Three articles discussed and compared removable and fixed orthodontic appliances and their effect on periodontal health. Levrini, et al. [20] evaluated the periodontal health and microbiological changes associated in patients undergoing fixed orthodontic treatment and Invisalign system. The study reported that patients treated with Invisalign system showed better periodontal health and lower quantity of pathological microbes compared to those who have been treated with fixed orthodontic appliances. The study concluded that orthodontic treatment using Invisalign system is better than fixed orthodontic appliances for the periodontal health [20] Abbate, et al. [25] evaluated and compared microbiological and periodontal changes that occur with orthodontic therapy by removable and fixed appliances. The study reported that the plaque index, probing depth and bleeding on probing all were significantly lower in patients treated with Invisalign system compared to patients treated with fixed brackets. Oral hygiene compliance was better in those treated with Invisalign system. The study concluded that teenagers that were treated with Invisalign aligners had better compliance with oral hygiene, less plaque and gingival inflammatory reactions than patients treated with fixed appliances [25]. Al-Moghrabi, et al. [23] evaluated and compared the stability of orthodontic treatment and periodontal health with fixed and removable retainers for 4 years. The study reported that both fixed and removable retainers showed similar periodontal outcomes with significant gingival inflammation and plaque levels. The study concluded that even though orthodontic appliances provide improved teeth alignment, both types were associated with gingival inflammation and elevated plaque scores [23]. Multiple studies compared various types of orthodontic treatment and it was collectively proposed that removable appliances such as Invisalign system had better periodontal health, as there was less plaque accumulation thus less inflammation [31]. Another article included in this review discussed the relation of the orthodontic appliances and periodontal health, focusing on oral hygiene as an influencing factor. Madariaga et al. evaluated periodontal health with supportive periodontal therapy on patients undergoing orthodontic treatment. The study reported that there was statistically significant decrease in pocket depth, bleeding on probing and plaque index in patients with fixed and removable appliances. The study concluded that if patients followed up with oral hygienist, both appliance types show similar impact on periodontal health.
Other study compared two types of fixed orthodontic wires and its effect on the periodontium. Corbett, et al. [22] evaluated and compared periodontal health of upper and lower anterior teeth retained with two types of fixed wires. The study reported that there was no significant difference in the various parameters including plaque index, gingival crevicular fluid volume, calculus index, recession, bleeding on probing, and pocket probing depths between both retainers. The study concluded that there was no clinical difference between straight twisted wire retainer and wave-type retainer when followed for 2-4 years [22,32,33].
Conclusion
This systematic review suggests that fixed orthodontic appliances using during orthodontic treatment has moderately affected periodontal health, increasing inflammation perception mainly due to increased plaque accumulation. If good and sufficient oral hygiene measures are maintained by the patient during treatment, then inflammation levels would decrease and become minimal.
Limitations
Only two studies were randomized control trials and only three studies considered a control group, which hinders generalization of review results. There were significant differences in age and sex distribution between compared studies. Aims and intentions of studies included had differences thus meta-analysis was not possible to conduct for this review. Further studies are needed to confirm results and specify the specific factors which are associated with the studied relationship.
References
- Gazit-Rappaport T, Haisraeli-Shalish M, Gazit E. Psychosocial reward of orthodontic treatment in adult patients. Eur J Orthod 2010; 32:441-446.
- Ristoska S, Dzipunova B, Stefanovska E, et al. Orthodontic treatment of a periodontally affected adult patient (case report). Open Access Macedonian J Med Sci 2019; 7:2343.
- Katancik JA, Kumarswamy A, Branch-Mays GR, et al. Infections of the periodontal apparatus. Head, Neck and Orofacial Infections: An Interdisciplinary Approach E-Book 2015; 189.
- Lang NP, Bartold PM. Periodontal health. J Periodontol, 2018; 89:S9-S16.
- Loesche WJ. Microbiology of dental decay and periodontal disease. Medical Microbiology. 4th Edn. 1996.
- Lertpimonchai A, Rattanasiri S, Vallibhakara SA, et al. The association between oral hygiene and periodontitis: A systematic review and meta-analysis. Int Dent J 2017; 67:332-343.
- dos Santos JN, Coelho TD, Cury PR, et al. The effect of dental plaque level and self-performed oral hygiene on periodontal status: A cross-sectional study in Brazilian Indigenous. J Health Biol Sci 2021; 9:1-6.
- Murakami S, Mealey BL, Mariotti A, et al. Dental plaque–induced gingival conditions. J Clin Periodontol 2018; 45:S17-S27.
- Feller L, Khammissa RA, Schechter I, et al. Biological events in periodontal ligament and alveolar bone associated with application of orthodontic forces. Scientific World J 2015; 2015.
- Årtun J, Urbye KS. The effect of orthodontic treatment on periodontal bone support in patients with advanced loss of marginal periodontium. Am J Orthod Dentofacial Orthop 1988; 93:143-148.
- Boas Nogueira AV, Chaves de Souza JA, Kim YJ, et al. Orthodontic force increases interleukin-1ß and tumor necrosis factor-a expression and alveolar bone loss in periodontitis. J Periodontol 2013; 84:1319-1326.
- Boyd RL. Periodontal and restorative considerations with clear aligner treatment to establish a more favorable restorative environment. Compendium 2009; 30.
- Antoun JS, Mei L, Gibbs K, et al. Effect of orthodontic treatment on the periodontal tissues. Periodontology 2017; 74:140-157.
- Sheibaninia A, Saghiri MA, Showkatbakhsh A, et al. Determining the relationship between the application of fixed appliances and periodontal conditions. African J Biotechnol 2011; 10:16347-16350.
- Gomes SC, Varela CC, Da Veiga SL, et al. Periodontal conditions in subjects following orthodontic therapy. A preliminary study. Eur J Orthod 2007; 29:477-481.
- Jiao J, Xin TY, Shi J, et al. Evaluation of periodontal status after orthodontic treatment: A pilot study on patients with stage IV/grade C periodontitis. Chin J Dent Res 2019; 22:229-239.
- Calniceanu H, Stratul SI, Rusu D, et al. Changes in clinical and microbiological parameters of the periodontium during initial stages of orthodontic movement in patients with treated severe periodontitis: A longitudinal site-level analysis. Exp Ther Med 2020; 20:1.
- Salvesen BF, Grytten J, Rongen G, et al. Periodontal status in long-term orthodontic retention patients up to 10 years after treatment–a cross-sectional study. Acta Odontol Scand 2021; 79:623-629.
- Pango Madariaga AC, Bucci R, Rongo R, et al. Impact of fixed orthodontic appliance and clear aligners on the periodontal health: A prospective clinical study. Dent J 2020; 8:4.
- Levrini L, Mangano A, Montanari P, et al. Periodontal health status in patients treated with the Invisalign® system and fixed orthodontic appliances: A 3 months clinical and microbiological evaluation. Eur J Den 2015; 9:404-410.
- Liu H, Sun J, Dong Y, et al. Periodontal health and relative quantity of subgingival Porphyromonas gingivalis during orthodontic treatment. Angle Orthod 2011; 81:609-615.
- Corbett AI, Leggitt VL, Angelov N, et al. Periodontal health of anterior teeth with two types of fixed retainers. Angle Orthod 2015; 85:699-705.
- Al-Moghrabi D, Johal A, O'Rourke N, et al. Effects of fixed vs removable orthodontic retainers on stability and periodontal health: 4-year follow-up of a randomized controlled trial. Am J Orthod Dentofacial Orthop 2018; 154:167-174.
- van Gastel J, Quirynen M, Teughels W, et al. Longitudinal changes in microbiology and clinical periodontal parameters after removal of fixed orthodontic appliances. Eur J Orthod 2011; 33:15-21.
- Abbate GM, Caria MP, Montanari P, et al. Periodontal health in teenagers treated with removable aligners and fixed orthodontic appliances. J Orofac Orthop 2015; 76:240-250.
- Willmot D. Orthodontic treatment and the compromised periodontal patient. Eur J Dent 2008; 2:1-2.
- Gehlot M, Sharma R, Tewari S, et al. Effect of orthodontic treatment on periodontal health of periodontally compromised patients: A randomized controlled clinical trial. Angle Orthod 2022; 92:324-332.
- Bollen AM. Effects of malocclusions and orthodontics on periodontal health: Evidence from a systematic review. J Dent Educ 2008; 72:912-918.
- Al-Haddad KA, Al-Hebshi NN, Al-Ak’hali MS. Oral health status and treatment needs among school children in Sana’a City, Yemen. Int J Dent Hygiene 2010; 8:80-85.
- Alfuriji S, Alhazmi N, Alhamlan N, et al. The effect of orthodontic therapy on periodontal health: A review of the literature. Int J Dent 2014; 2014.
- Azaripour A, Weusmann J, Mahmoodi B, et al. Braces versus Invisalign®: gingival parameters and patients’ satisfaction during treatment: A cross-sectional study. BMC Oral Health 2015; 15:1-5.
- Gorbunkova A, Pagni G, Brizhak A, et al. Impact of orthodontic treatment on periodontal tissues: a narrative review of multidisciplinary literature. Int J Dent 2016; 2016.
- Meeran NA, Parveen MJ. The scope and limitations of adult orthodontics. Indian J Multidiscip Dent 2011; 2.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Suhael Ahmed1*, Suha Basuhail2, Hadeel Basuhail2, Ghadeer Aldhafeeri2, Reem Jamaan Alghamdi2, Rana Ahmad Alaqel2, Suhailah Basuhail2 and Munirah Mohammed Alsuwaidan2
1Department of Oral and Mxillofacial surgery and Diagnostic Sciences, Riyadh Elm University, Riyadh, Saudi Arabia2Princess Nourah Bint Abdul Rahman University, Riyadh, Saudi Arabia
Received: 17-Oct-2022, Manuscript No. jrmds-22-77508; , Pre QC No. jrmds-22-77508(PQ); Editor assigned: 19-Oct-2022, Pre QC No. jrmds-22-77508(PQ); Reviewed: 02-Nov-2022, QC No. jrmds-22-77508(Q); Revised: 07-Nov-2022, Manuscript No. jrmds-22-77508(R); Published: 15-Nov-2022
