Research - (2022) Volume 10, Issue 12
Evaluation of the quantity of the single use plastic waste products in dental practice and hospital setup
Ankita Bajaj1*, Aayushi Sangal2, Shivani Dadwal Salaria3, Sunny Tandon2, Rajeev Kumar Singh4 and Visuja Chaudhary5
*Correspondence: Ankita Bajaj, Oral and Maxillofacial Surgeon, HH Dental and Maxillofacial Centre, India, Email:
Abstract
Objectives: Aim: To estimate the amount of single-use plastic trash created by dental treatment in Indian healthcare system. Methods: Observational studies were carried out at four dental practices and the clinics of a dental teaching hospital in India. As a result, competent and calibrated observers monitored all aspects of dental care from exams to endodontic procedures to direct-placement fillings to implant dentistry. Items such as pre- and post-pandemic personal protective equipment (PPE) were included as well. Results: Every time a patient is treated, common surgery set up generic products contributes a substantial amount plastic garbage. For each process, an average of twenty-one single-use plastic (SUP) garbage products (averaging 354 g in mass) are utilized (including set up and clean up). Pre-COVID-19 PPE was raised from 14 to 19 pieces during the epidemic. An approximately 50/50 distribution of plastics is used to make SUP objects, whether they are made from a single plastic or a combination of plastics (heteropolymers). Conclusions: There is a significant amount of single-use plastic used by the dentistry industry at the point of service, which ends up in the clinical waste stream. It is estimated that single-use plastic was used in every healthcare operation during the COVID 19 epidemic. PPE (personal protective equipment) usage rose dramatically throughout the pandemic. Clinical Significance: Companies in the oral healthcare industry have the chance to test out and execute waste management strategies focused on reduction, recovery, and recycling if they want to move toward a circular plastics economy in their industry.
Keywords
Pandemic, COVID-19, Plastics economy
Introduction
The seas receive an estimated 8 million metric tons of plastic garbage annually [1,2]. Furthermore, plastic pollution has a broad range of harmful consequences on the natural environment [3-7]. Plastic pollution is a major problem in the healthcare industry, as well as other industries [8,9]. More than 590,000 tonnes of garbage were generated by England's NHS providers in 2016/17. The concept of first, do no harm [10,11] is directly conflicted by the plastic contamination in healthcare services. One-time-use plastic items, such as Personal Protective Equipment (PPE), have become more important in the wake of the recent coronavirus (COVID-19) outbreak. Plastic pollution and life-saving PPE are the same thing.
It is a very recent trend in healthcare to employ plastic things, particularly single-use devices. In the 1950s, plastic items were initially used in healthcare as a practical and long-lasting replacement to conventional materials [12]. A short-term cost reduction was built into the product design from the start because of its multi-purpose use. Antibiotic-resistant bacteria and new illnesses like AIDS, Ebola, and SARS all emerged in the 1980s, causing the situation to drastically shift. Tuberculosis and malaria became more common. As a result of the convergence of these factors, a drug-free alternative to medicines was developed. Following numerous factors, including as the HIV/AIDS epidemic, the adoption of Universal Precautionary Measures and Single Use Plastics was conceivable [12]. The emergence of v-CJD (variant Creutzfeldt-Jacob disease) in the early 2000s provided new motivation for the usage of singleuse devices and single-dose pack-aged materials. In 2009, the Health Technical Memoranda (HTM) was introduced to consolidate these efforts of infection prevention and control. As a result of this accomplishment, new manufacturing processes with lower unit costs quickly emerged, allowing for the mass production of plastic goods. At first, the widespread use of plastic objects in dentistry was not considered an issue [13]. Dental offices in India were determined to be just "minor waste producers," according to an audit conducted in the early 1990s. Since a result, most practices at the time were not required to pay for waste management companies, as they could utilize local government rubbish collection services instead. It is still too early to see widespread use of plastic products as cross-infection controls. Single use plastic objects (SUPs) such as gloves, cups, and other things accounted up between 23 and 91% of the total garbage, according to research conducted by Farmer, et al. [14] a nine-fold increase in waste was recorded as a side effect of implementing Universal Precautions, according to the same assessment.
There has been an increase in the usage of plastic in dental restorative materials as a result of the rising use of resinbased composite (RBC) restoratives and the progressive phase-out of dental amalgam [15]. RBC materials, which are touted as the most frequent alternative to dental amalgam, have its own environmental issues [16-22].
When it comes to marine contamination, plastic trash has arisen as a global public problem since 2010. In addition, there has been an increase in studies on plastic waste in healthcare and dentistry [23]. Over half (53 percent) of all plastic trash generated in the UK's healthcare industry [24] is expected to come from the healthcare sector, which is expected to generate 6.3 million tons of plastic garbage by 2030.
Because equipment, commodities, and packaging fulfill the needs of all stakeholders, they are now essential for the safe and economical delivery of healthcare. When it comes to a risk-averse industry, what is up goods fulfill all of the major criteria and give the requisite clinical and public confidence by using fresh, clean and/or sterile devices every time with zero chance of contamination. Laws are in place in India to protect the safety of individuals receiving oral health treatment [13,23]. As a consequence of this kind of one-sided legislative regulation focused only on patient safety, the cost of waste services increased by 58% [25,26]. There are a number of reasons why SUP-based biomedical waste created by consumers and professional oral healthcare providers (such as clinical sun-dries and restorative materials) ads to a highly wasteful linear economy for SUPs as a consequence of these numerous factors:
Since SUPs are increasingly being used in oral healthcare, a baseline of data is needed to identify the total use of SUPs and therefore act as a driver to reverse the trend of what is up utilization. Stakeholders throughout the supply chain will benefit from this information, which will help them find ways to eliminate or recycle SUPs in their respective roles and in the overall chain. The study's goal is to count and weigh the single-use plastic items used in India primary care clinical dentistry settings to provide oral health care services (by mass and quantity). To ensure that oral healthcare services are delivered safely, two scenarios are considered: “Oral healthcare products and PPE (personal protective equipment) prescribed by the Indian government (COVID-19 control measures, June 2020) [27].”
Methods
As part of the procedure, all of the dental treatment that is being provided to adults in primary care settings in India was counted, weighed, and recognized. Data collection tools for particular dental procedures were devised, developed, and validated during the course of a fourweek pilot research at the hospital for undergraduates. An itemized list of what is up products (and their principal packing) was supplied in the data collection tool, which allowed for the insertion of additional things not specified. Endodontic treatment, periodontics, and restorative (direct placement restoration) and removable prosthodontics were also examined as part of the study (dental extractions, minor oral surgery and biopsies).
Researchers who have practical experience with patientcentered clinical therapy participated in this study. It was important that the investigators were impartial, non-participatory, and not in the way of the treatment itself. They were well-versed in the data collecting procedure and ensured that all clinical governance standards and health and safety requirements were followed. The following data was gathered and analyzed by the investigators: Observed patient-based clinical procedures and the date, time, and location of each what is up item employed. As a part of the study, a clinician and a dental nurse were observed doing clinical patient interventions. No personal or identifying information about the patient or the medical team was recorded. Dental primary care clinics, which included government and private dental offices and a dental teaching hospital, were used for the research. Primary dental care in India is provided through dental offices and teaching hospitals that are deemed to be completely typical of their kind. The observations were put through a risk assessment to make sure everyone was safe and to keep things running as smoothly as possible.
Generic information (setting, time, technique) and a comprehensive itemized list of what is up items utilized throughout the course of entire patient-centered clinical procedures were gathered. The total mass of what is up utilized and discarded throughout the operation was calculated by collecting and weighing samples of each what is up item. Over the course of four months, from October 1st2021, to January 30th, 2022, investigators conducted their investigations in four separate cities. Each of the three dental offices and the dental teaching hospital's restorative dentistry department performed 147 observations altogether (Table 1 and Figure 1). As a result of the COVID-19 pandemic, more PPE was employed to provide aerosol generating procedures (AGPs) to health workers.
| Procedure | Number of observations per procedure |
|---|---|
| Dental examinations | 79 |
| Periodontal treatment | 24 |
| Endodontic treatment | 7 |
| Direct placement restorations | 31 |
| Prosthodontic (Fixed &removable) | 7 |
| Oral surgery treatment | 9 |
| Total | 147 |
Table 1: Number of observations conducted per dental procedure.
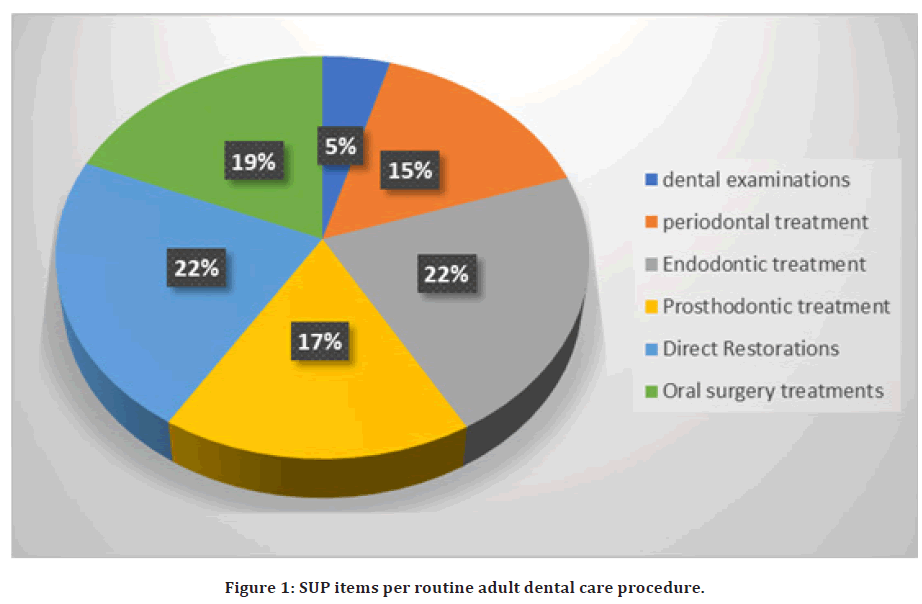
Figure 1. SUP items per routine adult dental care procedure.
Results
We collected and examined the data for each location in turn, both individually and collectively as necessary. As a result of the data showing similarities across the four locations, an extensive data set was created for further investigation. The one exemption was the use of nitrile gloves, which were permitted. Undergraduate restorative dentistry students at the teaching hospital used significantly fewer gloves than practicing dentists in their clinical rotations. Restorative dentistry clinical education involves the application of cross-infection control techniques relevant to clinical governance for usage in open, multi-user clinical settings. There are a lot more pairs of gloves needed for these tasks since they need to examine patient data, use the chair-side computer or get equipment from the dispensary while wearing gloves. “Data on the usage of nitrile gloves by dental students and dentists has been separated to prevent any misunderstandings. Dental offices and a teaching hospital's Oral Surgery Department were included in this research, however student data was not included in the normalization of data for personal protective equipment and cleaning supplies.”
Suppression of the use of single-use plastics in medical procedures reduces the amount of plastic trash produced by generic products (used in normal operation set-up). The average number of what is up items used in a regular adult primary care dental surgery was found to be twenty-one (n =21), with a mass of 354 g on average (including set up and clean up). According to our findings, the following is the sequence in which what is up items are most likely to be utilized during an adult care procedure: Periodontal care is the last step in the process of providing direct placement restorations, root canal therapy and oral surgery for minor surgical operations. During the pandemic, the number of PPE items used rose from 14 (pre-COVID 19) to 19.
There was a roughly 50/50 split between SUPs built from a single plastic and those made from a composite structure composed of numerous plastics (heteropolymers) in the construction of their composition.
Discussion
For this study, the researchers set out to determine the prevalence of SUPs in adult oral health care operations, as well as to count and weigh them in order to get a sense of just how widespread the problem is and what steps should be taken to address it.
All the information presented shows that SUPs are often used for routine treatments in primary care dentistry. Dentist and nurse personal protective equipment (PPE) like as gloves and a mask, as well as particular items for setup and cleaning (wipes, sterilizing sleeves, and tray liners) are the most regularly used supplies. Exam gloves are the most often used what is up item, with most patients requiring many pairs. The COVID-19 epidemic has also led to an increase in the usage of Personal Protective Equipment (PPE), according to this data.
“With the utilization of the information from this exploration, it is doable to gather with a serious level of certainty the cross country utilization of SUPs in dentistry practice. During the COVID-19 pandemic, this number moved to around 2.4 billion (27 tons). A safe approximation of 352 million nitrile gloves is involved each year in typical grown-up essential consideration clinical methods in India [28-30].
Dentists have utilized observational auditing methods to determine the volume and type of trash generated by their operations [26,31]. These methodologies are applied in this research, which focuses on the connection between dental operations and the plastic items used and disposed of as a consequence of the delivery of this patient-centered process. As a result, no consideration is given to the extra plastic trash that is generated farther upstream in the supply chain. This should be noted when doing this kind of study elsewhere.
When it comes to providing people with routine primary oral healthcare, our research on the usage of SUPs has produced a mixed picture. PPE is required at every step of the procedure, but that does not mean it is not necessary (before and during the COVID-19 pandemic).A significant percentage of what is up waste was derived from the use of PPE, which was repeatedly worn and doff throughout specific patient-based procedures. In contrast, a large range of specialized what is up plastic goods with a complicated assembly nature are available, constructed from highly cross-linked polymers and treated in such a way that they cannot be readily broken down into the component raw ingredients or derivatives. For complicated polymer-based devices that have been constructed in numerous layers and welded together, disassembly is very difficult or impossible. PVC, for example, when heated emits HCl and organic Cl-containing byproducts, making it a difficult polymer to work with if you want to do any chemical processing at all. “To avoid contamination and to make cleaning, disinfecting, and sterilizing polymer devices in the clinical context easier, these devices have been designed with a single-use design in mind. [23]”
A substantial amount of additional what is up data might be gathered by including sterilizing packing and pouches in this analysis. Due to pre-opened or multiple-packaged products, the packaging was an issue throughout the event. “In the dentistry sector, packaging is generally acknowledged as the single greatest contributor to plastic trash, as it goes down the supply chain to the dental surgery and end user, with most (>90 percent) ending up as garbage for incineration or landfill.”
In order to provide an accurate picture of the cumulative effect of SUPs for each operation, it is necessary to consider the frequency with which it is performed. This analysis is made possible by publicly available data on the amount of activity for various treatments performed by dental facilities in India [32-35]. Direct-placement restorations accounting for 12.5% of all treatments in 2021/22 (amalgam, resin-based composite, and glass ionomers together accounted for the remainder). Approximately 41.5 percent of the year's activities was dedicated to dental examination. As Borglin, et al. [36] noted out, dental examination create more than three times Sups as any other kind of dental procedure. This is instantly obvious. Manufacturers and clinical care providers may work together to find methods to reduce the usage of these plastics and recycle them (mechanically or chemically) for use in low-value goods like building bricks, fences, park benches, etc. or as a feedstock for new polymers [37].
The management of clinical waste and its primary and secondary packing is becoming a serious problem because of the threat of an infectious disease pandemic, as well as laws and public pressure to improve patient safety. “The level of safety required for clinical treatment and the accompanying usage of personal protective equipment (PPE) has been enhanced as a result of the COVID-19 pandemic. In the previous section of this essay, we said that this is a one-way road with rising levels of security. This pandemic has shifted the attention away from the environment and will need a shift in viewpoint. PPE in oral health care has to be standardized so that it may be used by people of various economic and development levels across the world. Ecologically sustainable PPE must be collected and recycled to ensure that it provides the necessary protection for people and the environment, as well as ensuring that PPE can be collected and repurposed."
SUPs' negative environmental impact may be minimized by recycling and decreasing rubbish at its source, according to a United Nations inverted pyramid for managing waste [38,39]. "Reduction and recycling are the primary motivators for the oral health supply chain from this standpoint. "— (pre- and post-clinical contamination). For SUPs coming from packaging or clinical waste, reuse is not possible. With rethinking (the fourth R in the Reduce Reuse Recycle and Rethink acronym), we are challenged to think about how we might engage in reduction and recycling to tackle the inherent problems this presents to our industry," he writes. The most practical and easily implemented remediation technique is to concentrate on reducing and recycling. Dentists should concentrate on preventative measures and provide lasting treatments that will endure for a longer period of time or need fewer adjustments to maintain excellent oral health. This method tries to eliminate the need for dental products and visits to the dentist. To decrease packaging waste farther up the supply chain, numerous methods may be used, such as undertaking a systematic review of packaging requirements and removing unneeded packaging that travels down the supply chain [40-43]. Recover the value of discarded plastic packaging by cooperating with all parties in the supply chain. Waste management partnerships with end users and waste management businesses to sort, collect and recycle clinical SUPS as a valuable commodity; (iii) single-plastic products that can be recycled easily." To restate, dental plastics are an essential material that delivers safe, effective, and efficient patient-centered treatment. One of the most pressing issues of our day is that plastic must be moved from its existing linear life cycle of production from fossil-based resources and trash disposal to a circular economy. Renewable and/or bio based component materials are used in circular economies to generate end goods, which are subsequently recovered and recycled to create new polymers as valuable feedstock. When reducing capacity on a local and supply chain level, packaging should also be taken into account.
We can reduce the amount of plastic we use by encouraging high standards of oral health care that emphasize disease prevention. Excellent oral health results in less surgery, which minimizes the carbon footprint and environmental impact. A greater emphasis on recycling should be placed on healthcare SUPs (including PPE) and package management in order to reduce waste (mechanical and chemical). For a more environmentally friendly strategy that uses less plastic, best practices in technology, logistics management, and environmental constraints must be used.
Conclusion
Dental professionals utilize a large amount of singleuse plastics at the point of service, which generates significant clinical waste. Ideally, some energy may be recovered from the waste before it is sent to a landfill or incinerator for disposal. In order to reduce the negative environmental consequences of these items, it is essential to rethink their usage in order to preserve their material features.
References
- Jambeck JR, Geyer R, Wilcox C, et al. Marine pollution. Plastic waste inputs from land into the ocean. Science 2015; 347:768–71.
- Eriksen M, Lebreton LC, Carson HS, et al. Plastic pollution in the world's oceans: More than 5 trillion plastic pieces weighing over 250,000 tons afloat at sea. PloS One 2014; 9:e111913.
- Bamai YA, Miyashita C, Araki A, et al. Effects of prenatal di (2-ethylhexyl) phthalate exposure on childhood allergies and infectious diseases: The hokkaido study on environment and children's health. Sci Total Environ 2018; 618:1408-1415.
- Gao X, Wang HS. Impact of bisphenol A on the cardiovascular system—Epidemiological and experimental evidence and molecular mechanisms. Int J Environ Res Public Health 2014; 11:8399-8413.
- Erler C, Novak J. Bisphenol a exposure: Human risk and health policy. J Pediatr Nurs 2010; 25:400-407.
- Minatoya M, Sasaki S, Araki A, et al. Effects of prenatal phthalate exposure on thyroid hormone levels, mental and psychomotor development of infants: The Hokkaido study on environment and children's health. Sci Total Environ 2016; 565:1037-1043.
- Peretz J, Vrooman L, Ricke WA, et al. Bisphenol A and reproductive health: Update of experimental and human evidence, 2007–2013. Environ Health Perspective 2014; 122:775-786.
- Duane B, Ramasubbu D, Harford S, et al. Environmental sustainability and waste within the dental practice. Br Dent J 2019; 226:611-618.
- Leonard A, Dunn H, Wilson N. The ‘gloves are off’–can we reduce inappropriate glove usage through an educational based intervention and risk assessment. Arch Dis Child 2018; 103.
- https://www.gov.uk/government/collections/chief-medical-officer-annual- reports
- https://noharm-global.org/documents/health-care-climate-footprint-report
- Hodges S. Hospitals as factories of medical garbage. Anthropol Med 2017; 24:319-333.
- https://www.england.nhs.uk/wp-content/uploads/2021/05/HTM_01-05_2013.pdf
- Farmer GM, Stankiewicz N, Michael B, et al. Audit of waste collected over one week from ten dental practices. A pilot study. Aust Dent J 1997; 42:114-117.
- http://mercuryconvention.org/
- Mulligan S, Kakonyi G, Moharamzadeh K, et al. The environmental impact of dental amalgam and resin-based composite materials. Br Dent J 2018; 224:542-548.
- Polydorou O, König A, Hellwig E, et al. Long‐term release of monomers from modern dental‐composite materials. Eur J Oral Sci 2009; 117:68-75.
- Polydorou O, Schmidt OC, Spraul M, et al. Detection of Bisphenol A in dental wastewater after grinding of dental resin composites. Dent Mater 2020; 36:1009-10018.
- Reidelbach C, Garcia-Käufer M, Wingert N, et al. Cytotoxicity and estrogenicity in simulated dental wastewater after grinding of resin-based materials. Dent Mater 2021; 37:1486-1497.
- Putzeys E, De Nys S, Cokic SM, et al. Long-term elution of monomers from resin-based dental composites. Dent Mater 2019; 35:477-485.
- https://awsassets.panda.org/downloads/plastic_ingestion_press_singles.pdf
- Maye D, Kirwan J, Brunori G. Ethics and responsibilisation in agri-food governance: the single-use plastics debate and strategies to introduce reusable coffee cups in UK retail chains. Agric Human Values 2019; 36:301-312.
- Martin N, Mulligan S, Fuzesi P, et al. Waste plastics in clinical environments: a multi-disciplinary challenge, in: Creative circular economy approaches to eliminate plastics waste. Plastics Research and Innovation Fund Conference, University of Sheffield. UK Research and Innovation and UK Circular Plastics Network 2020; 86–91.
- https://www.gov.uk/government/ statistical-data-sets/env23-uk-waste-data-and-management
- https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/690846/CMO_Annual_Report_2017_Health_Impacts_of_All_Pollution_what_do_we_know.pdf
- Richardson J, Grose J, Manzi S, et al. What's in a bin: A case study of dental clinical waste composition and potential greenhouse gas emission savings. Br Dent J 2016; 220:61-66.
- https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/06/C0581-covid-19-urgent-dental-care-sop-update-16-june-20-.pdf
- https://www.gdc-uk.org/docs/default-source/registration-reports/gdc-registration-statistical-report-2020---final311fef86-9e9f-44bb-81d8-68b3a44cae39.pdf?sfvrsn=918f77ec_8
- Mulligan S, Smith L, Martin N. Sustainable oral healthcare and the environment: Challenges. Dent Update 2021; 48:493-501.
- Martin N, Smith L, Mulligan S. Sustainable oral healthcare and the environment: Mitigation strategies. Dent Update 2021; 48:524-531.
- Kizlary E, Iosifidis N, Voudrias E, et al. Composition and production rate of dental solid waste in Xanthi, Greece: Variability among dentist groups. Waste Manag 2005; 25:582-591.
- Rizan C, Mortimer F, Stancliffe R, et al. Plastics in healthcare: Time for a re-evaluation. J Royal Soc Med 2020; 113:49-53.
- https://wrap.org.uk/taking-action/plastic-packaging/the-uk-plastics-pact
- https://europeanplasticspact.org/.
- https://www.gov.uk/government/publications/carbon-modelling-within-dentistry-towards-a-sustainable-future
- Borglin L, Pekarski S, Saget S, et al. The life cycle analysis of a dental examination: Quantifying the environmental burden of an examination in a hypothetical dental practice. Community Dent Oral Epidemiol 2021; 49:581-593.
- Bin Jumah A, Anbumuthu V, Tedstone AA, et al. Catalyzing the hydrocracking of low density polyethylene. Ind Eng Chem Res 2019; 58:20601-20609.
- https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/06/C0575-dental-transition-to-recovery-SOP-4June.pdf
- https://cwm.unitar.org/national-profiles/publications/cw/wm/UNEP_UNITAR_NWMS_English.pdf
- Martin N, Mulligan S. Environmental sustainability through good-quality oral healthcare. Int Dent J 2022; 72:26.
- https://www.bpf.co.uk/article/new-flexible- packaging-industry-consortium-to-bring-circular-eco-1138.aspx
- Martin N, Sheppard M, Gorasia G, et al. Awareness and barriers to sustainability in dentistry: A scoping review. J Dent 2021; 112:103735.
- Martin N, Sheppard M, Gorasia G, et al. Drivers, opportunities and best practice for sustainability in dentistry: A scoping review. J Dent 2021; 112:103737.
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Indexed at, Google scholar, Cross Ref
Author Info
Ankita Bajaj1*, Aayushi Sangal2, Shivani Dadwal Salaria3, Sunny Tandon2, Rajeev Kumar Singh4 and Visuja Chaudhary5
1Oral and Maxillofacial Surgeon, HH Dental and Maxillofacial Centre, Bareilly, India2Noida International Institute of Medical Sciences, Greater, Noida, India
3Department of Periodontics, Santosh Dental College, Ghaziabad UP, India
4Pedodontics and Preventive Dentistry, K D Dental College and Hospital Mathura (UP), India
5ITS Dental College, Greater Noida, India
Received: 28-Nov-2022, Manuscript No. jrmds-22-78375; , Pre QC No. jrmds-22-78375(PQ); Editor assigned: 30-Nov-2022, Pre QC No. jrmds-22-78375(PQ); Reviewed: 15-Dec-2022, QC No. jrmds-22-78375(Q); Revised: 19-Dec-2022, Manuscript No. jrmds-22-78375(R); Published: 26-Dec-2022
