Research Article - (2020) Volume 8, Issue 4
Evaluation of Tracheal Index in Obstructive Airway Disease Using High Resolution Computed Tomography (HRCT)
Omair Ashraf Shah*, Iqbal Javaid, Manzoor Aaqib, Gojwari Tariq, Shera Tehleel and Shera Faiz
*Correspondence: Omair Ashraf Shah, Department of Radiology, SKIIMS SOURA, Jammu and Kashmir, India, Email:
Abstract
Purpose: To assess the change in Tracheal index in patients of COPD as a function of severity and its correlation with PFT parameters.
Methods: HRCT scans of 48 patients were done and correlated with Pulmonary Function Tests taken within 2 weeks of the study. We obtained TI by dividing the coronal diameter of the trachea by sagittal diameter and multiplying it by 100 at a level 2 cm above the aortic arch. These values were then correlated with COPD severity based on PFT results.
Results: The mean tracheal index in our study was 0.672 ± 0.10. The mean tracheal index in mild emphysema group was 0.73 ± 0.07 and in the moderate to severe group 0.61 ± 0.08. A significant correlation was found between tracheal index and PFT parameters signifying COPD severity i.e. FEV1, FEV1/FVC, RV/TLC and Pef 25%-75%.
Conclusion: Tracheal index is a marker of severity of COPD and it has significant association with the PFT parameters in these patients. Large airway changes in COPD patients can predict lung function and small airway changes.
Keywords
Tracheal index, Forced expiratory volume in 1 sec, High resolution computed tomography, PEF25-75% Peak expiratory flow (25–75%), Pulmonary function testIntroduction
Obstructive airway diseases are respiratory diseases characterized by airway obstruction. Although COPD shares similar characteristics with other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms and reversibility of airway obstruction [1]. Diagnosis of obstructive airway diseases requires several factors depending on the exact disease being diagnosed. However, one common criterion is a FEV1/FVC ratio less than 0.7. COPD includes emphysema and chronic bronchitis which usually overlap in each patient [2].
Smoking is a common patho-etiogenic factor in COPD. COPD has been classified based on PFT parameters into 4 grades: Mild-FEV1/FVC <0.70, FEV1 ≥ 80% predicted; Moderate- FEV1/FVC <0.70, FEV1 50-80% predicted; Severe- FEV1/FVC <0.70, FEV1 30-50% predicted; Very Severe- FEV1/FVC <0.70, FEV1 <30% predicted or FEV1 <50% predicted plus chronic respiratory failure [3]. Inspiratory HRCT helps in evaluation of morphology of interstitium and lung parenchyma [4]. In patients of small airway disease, an expiratory scan may provide additional information including functional assessment of airway obstruction [5]. Expiratory scans can be useful in assessing air trapping in patients with normal or mildly deranged PFT. This is because PFT provides a global overview and may be normal until large areas of both lungs are involved [6].
Many studies have been carried out to correlate radiological parameters obtained on HRCT with lung morphological changes and lung functional changes in patients of COPD. Air trapping, mean lung HU and tracheal collapse area are some of these parameters that have been assessed by various researchers in COPD. These parameters are also significantly correlated with lung function parameters, even in mild COPD [7–10].
Tracheal index is one parameter that assesses the large airway change in patients with COPD. This index is calculated on axial HRCT scans by dividing the maximum coronal diameter by maximum sagittal diameter. The level of measurement has varied among various studies but 2 cm above the aortic arch appears to be the best level for measurement. Saber-sheath trachea, a common feature seen in COPD patients has been defined as a tracheal index (TI) of less than 2/3 or 0.67 [11].
Our study was aimed to find out the large airway changes in the patients of COPD and to assess whether the large airway changes can predict the severity of COPD associated PFT changes. The association of degree of emphysema with large airway abnormalities in the form of tracheal index was also sought in our study.
Methods
The study was an observational prospective study and was conducted in Department of Radio diagnosis and Imaging SKIMS Srinagar from October 2016 to June 2018. The patients included in our study were referred from the Department of Pulmonology as cases of obstructive airway disease. Pregnant patients, those with lung mass/consolidation and those with pleural effusions were excluded from the study.
CT scanning protocol
All CT scans were done in the Department of Radio-diagnosis & Imaging SKIMS, Soura using CT SOMATOM SENSATION 64 with the following parameters:
120 kV voltage, 150 mA tube current, 5 mm section thickness, 0.5–0.6 s tube rotation, and 1.25 mm detector collimation. Inspiratory scans were obtained at the end of full inspiration. Images were reconstructed with a slice thickness of 1 mm and a reconstruction interval of 0.5 mm using B-70 sharp kernel.
Interpretation of CT scans
The HRCT scans were assessed by a radiologist with 5 years’ experience in thoracic imaging. The morphology and degree of emphysema in all patients was assessed. The patients were divided into two groups according to Inspiratory Reserve Volume <-950 value i.e. the volume of lung between -950 HU and -1024 HU. Mild emphysema group (IRV <-950 <15%) and moderate to severe emphysema group (IRV<- 950 >15 %,). -950 HU has been validated by many previous studies as being the threshold for emphysema. The large airway changes were noted, and tracheal index calculated by dividing the maximum coronal diameter by maximum sagittal diameter. The measurements were obtained at a level 2 cm above the aortic arch on axial plane. Three measurements were obtained by a single observer and a mean of these three measurements was taken as the final value.
Pulmonary function tests
PFTs were performed within 2 weeks of obtaining CT scans using PC BASED MEDIKRO WINDOWS SPIROMETER WITH SOFTWARE VERSION 1.8 manufactured by MEDIKRO OY Finland. The spirometric parameters were recorded in accordance with the American Thoracic Society Guidelines 2005. The tracheal index values were then correlated with PFT parameters to look for any significant relation.
The values were expressed as mean ± SD. We segregated our patients into mild and moderatesevere emphysema groups based on values of inspiratory relative volume <–950. Comparisons of tracheal index between the moderate to severe emphysema group and mild emphysema group were done using the two sample Independent t-test, one-way analysis of variance and Pearson's correlation coefficient. Tracheal index values were also correlated with PFT parameters. p -value less than 0.05 was statistically significant.
Results
Patient profile
We conducted HRCT scans of 48 COPD patients and correlated them with PFT results. Of the 48 patients in our study, 20(42%) were females and 28(58%) were males. The mean age of patients in our study was 52.27 ± 13.30 yrs. The age range was 40–80yrs.
Smoking history
Among the 48 patients in our study, 43(90%) were smokers and 5(10%) were nonsmokers. A significant difference in PFT parameters and tracheal index between smokers and nonsmokers was found in our study (p<0.005).
Inspiratory relative volume -950--1024 HU (IRV <-950)
The mean value of IRV <-950 in our patients was 14.26% ± 6.22%. The patients were divided into two groups according to IRV <-950 values: Mild emphysema group (IRV <-950 <15%, mean value=8.79% ± 3.21%, mean age=50.12 ± 13.3) and moderate to severe emphysema group (IRV<-950 >15%, mean value=19.72% ± 2.58%, mean age=54.44 ± 13.20) (Table 1).
| Group | N | Mean IRV |
|---|---|---|
| Mild emphysema | 24 | 8.79% ± 3.21% |
| Moderate-severe emphysema | 24 | 19.72% ± 2.58% |
| Total | 48 | 14.26 % ± 6.22% |
Table 1: Mean IRV and division of patients into two groups: mild emphysema group and moderate-severe emphysema group.
Tracheal index
The tracheal index was calculated by the formula: Coronal tracheal diameter/ Sagittal tracheal diameter.
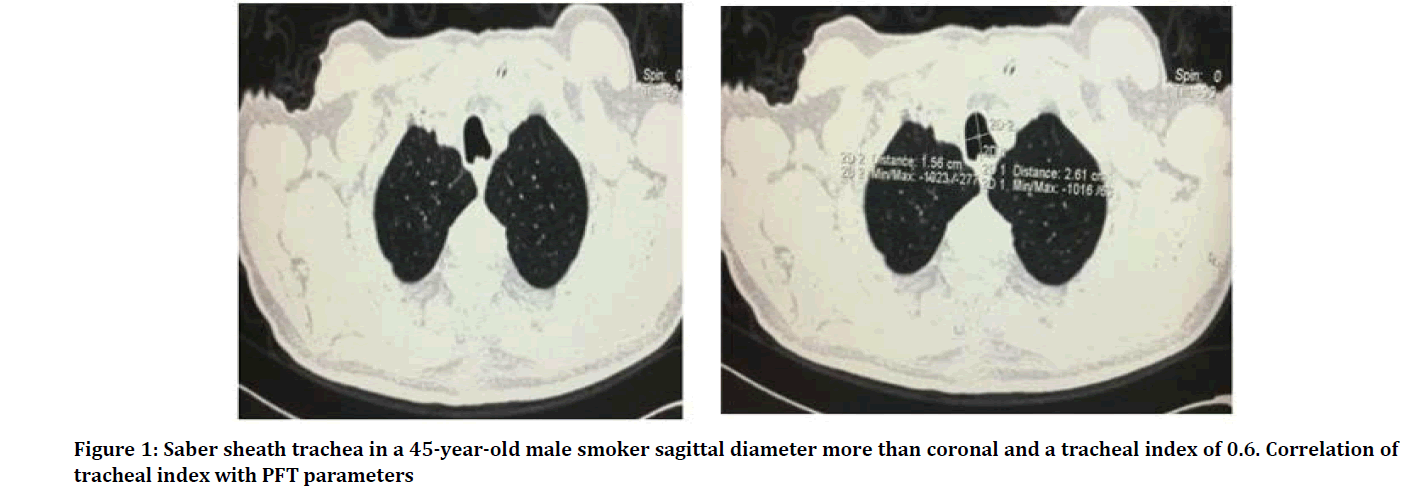
The measurements were taken 2cm above aortic arch in axial planes. The mean tracheal index in our study was 0.672 ± 0.10. The mean tracheal index in mild emphysema group was 0.73 ± 0.07 and in the moderate to severe group 0.61 ± 0.08 (Figure 1).
Figure 1: Saber sheath trachea in a 45-year-old male smoker sagittal diameter more than coronal and a tracheal index of 0.6. Correlation of tracheal index with PFT parameters
Correlation of tracheal index with PFT parameters
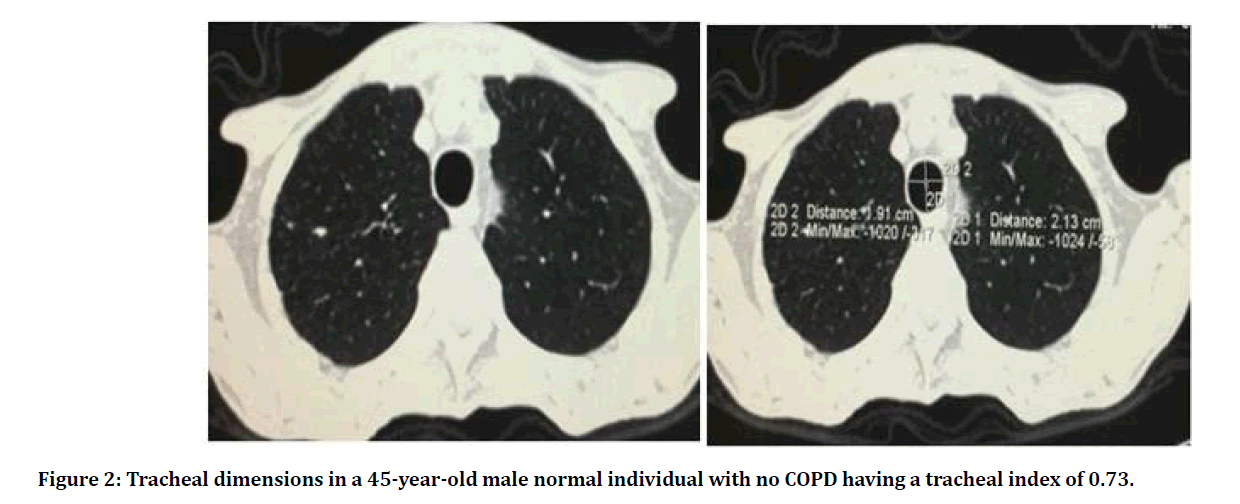
We correlated the tracheal index in our patients with the PFT parameters obtained within 2 weeks of the HRCT scan. We found a significant correlation between the PFT parameters signifying airway dysfunction i.e. FEV1 (p value .003), FEV1/FVC (p value <0.0001), RV/TLC (p value <0.0001), Pef 25% -75 % ( p value 0.047) and tracheal index (Table 2 and Figure 2).
Figure 2: Tracheal dimensions in a 45-year-old male normal individual with no COPD having a tracheal index of 0.73.
| fev1 | fev1_fvc | Pef 25%-75% | rv_tlc | ||
|---|---|---|---|---|---|
| Tracheal index | Pearson Correlation | 0.419** | 0.552** | 0.277 | -0.530** |
| p-value | 0.003 | <0.0001 | 0.047 | <0.0001 | |
| N | 48 | 48 | 48 | 48 |
Table 2: Correlation of tracheal index with PFT parameters signifying airway dysfunction in patients of COPD.
Discussion
This study was conducted over a period of 2 years in our center and included 48 patients with a mean age of 52.27 ± 13.30 yrs. (40 –80yrs). The male to female ratio in our study was 28(58%): 20 (42%). These are concordant with the numbers in the studies done by Trigaux et al. [12] and Muro et al. [13]. Among the 48 patients in our study 43(90%) were smokers and 5(10%) were smokers.
We conducted inspiratory HRCT scans in all our patients and obtained the tracheal measurements after transferring the images to a dedicated workstation. After obtaining the scans we divided our patients into two groups according to the degree of emphysema. This was done based on the quantitative measurement of IRV <-950 values: mild emphysema group (IRV <-950 <15%, mean value=8.79% ± 3.21%, mean age=50.12 ± 13.3) and moderate to severe emphysema group (IRV<-950 >15%, mean value=19.72% ± 2.58%, mean age= 54.44 ± 13.20).
The large airway changes in patients of COPD were assessed in our study in the form of Tracheal Index. The measurements were taken 2cm above aortic arch in axial planes. The mean tracheal index in our study was 0.672 ± 0.10. The mean tracheal index in mild emphysema group was 0.73 ± 0.07 and in the moderate to severe group 0.61 ± 0.08. This difference was statistically significant. We also found a significant difference in the tracheal index values between smokers and nonsmokers (p value <0.005). Thus, it can be concluded that large airway changes are a guide to the degree of emphysema in patients of COPD and may indicate COPD severity. This is further proved by the fact that tracheal index had a significant correlation with PFT parameters that determine COPD severity in our study: FVC (p value .003), FEV1/FVC (p value <0.0001), RV/ TLC (p value <0.0001), Pef 25%-75 % (p value .047) (Table 2). We can therefore conclude that large airway changes in COPD are intricately linked to the small airway modifications and that the large airway changes increase in severity with increasing COPD severity. Thus, large airway change in the form of tracheal index can serve as a morphological marker of COPD severity and can measured easily on inspiratory HRCT scans and is quite an accurate and reproducible measurement. The results of our study correlating tracheal index and COPD severity has also been found by Trigaux et al. [12], Gupta et al. [14], Leader et al. [15] and Lee et al. [16] in their studies. All these researchers found a significant correlation of decreased tracheal index with lung hyperinflation and functional obstruction parameters (PFT).
Limitations of our study included limited number of patients; however, the number of patients were like previous studies. Also, the measurements made in our study was at a single level (2 cm above the aortic arch) while tracheal changes may affect any part, however this level has been taken as the standard by many studies in the past. Also, we did not conduct dynamic evaluation the trachea on inspiratory and expiratory scans to assess for tracheal collapsibility as the paired scans can expose a person to significant radiation dose.
Conclusion
Large airway morphological changes in COPD can predict the degree of emphysema and COPD severity. Tracheal index is a sensitive measure of large airway modification in COPD patients and is significantly lower in smokers and severe COPD patients. Tracheal index is significantly associated with the PFT parameters signifying airway dysfunction.
References
- National Asthma Education and Prevention Program. Clinical Practice Guidelines. Expert panel report 2. Guidelines for the diagnosis and management of asthma. Bethesda: National heart, lung, and blood institute, national institutes of health, US Department of Health and Human Services. NIH Publication 1997; 97-4051.
- Sheppard R, Vinay K, Abbas AK, et al. Robbins basic pathology. 8th Edn. Philadelphia: Saunders 2007; ISBN 1-4160-2973-7.
- https://goldcopd.org/
- Kazerooni EA. High-resolution CT of the lungs. Am J Roentgenol 2001; 177:501-519.
- Mavili E, Büyükoğlan H, Çomul NB, et al. Correlation with pulmonary function tests and value for discriminating lung diseases. Eur J Gen Med 2010; 7:56-62.
- Kauczor HU, Hast J, Heussel CP, et al. CT attenuation of paired HRCT scans obtained at full inspiratory/expiratory position: comparison with pulmonary function tests. Eur Radiol 2002; 12:2757-2763.
- Xie X, de Jong PA, Oudkerk M, et al. Morphological measurements inc omputed tomography correlate with airflow obstruction in chronic obstructive pulmonary disease: Systematic review and meta-analysis. Eur Radiol 2012; 22:2085–2093.
- Mohamed Hoesein FA, van Rikxoort E, van Ginneken B, et al. Computed tomography-quantified emphysema distribution is associated with lung function decline. Eur Respir J 2012; 40:844–850.
- Mohamed Hoesein FA, de Hoop B, Zanen P, et al. CT-quantified emphysema in male heavy smokers: Association with lung function decline. Thorax 2011; 66:782–787.
- Heussel CP, Herth FJ, Kappes J, et al. Fully automatic quantitative assessment of emphysema in computed tomography: Comparison with pulmonary function testing and normal values. Eur Radiol 2009; 19:2391–2402.
- Greene R. Saber-sheath trachea: relation to chronic obstructive pulmonary disease. Am J Roentgenol 1978; 130:441–445.
- Trigaux JP, Hermes G, Dubois P, et al. CT of saber-sheath trachea. Correlation with clinical, chest radiographic and functional findings. Acta Radiol 1994; 35:247-250.
- Muro S, Nakano Y, Sakai H, et al. Distorted trachea in patients with chronic obstructive pulmonary disease. Respiration 2000; 67:638-644.
- Gupta PP, Yadav R, Verma M, et al. Correlation between high-resolution computed tomography features and patients’ characteristics in chronic obstructive pulmonary disease. Ann Thorac Med 2008; 3:87-93.
- Leader JK, Rogers RM, Fuhrman CR, et al. Size and morphology of the trachea before and after lung volume reduction surgery. Am J Roentgenol 2004; 183:315-321.
- Lee HJ, Seo JB, Chae EJ, et al. Tracheal morphology, and collapse in COPD: Correlation with CT indices and pulmonary function test. Eur J Radiol 2011; 80:531-535.
Author Info
Omair Ashraf Shah*, Iqbal Javaid, Manzoor Aaqib, Gojwari Tariq, Shera Tehleel and Shera Faiz
1Department of Radiology, SKIIMS SOURA, Jammu and Kashmir, IndiaCitation: Omair Ashraf Shah, Iqbal Javaid, Manzoor Aaqib, Gojwari Tariq, Shera Tehleel, Shera Faiz, Evaluation of Tracheal Index in Obstructive Airway Disease Using High Resolution Computed Tomography (HRCT), J Res Med Dent Sci, 2020, 8 (4): 01-05.
Received: 01-Jun-2020 Accepted: 19-Jun-2020 Published: 26-Jun-2020