Research - (2021) Volume 9, Issue 8
Evaluation Pathogenesis Outcomes of Knee and Hip in Patients with Osteoarthritis Based on: Histopathological, Hematological, and Indicators of Inflammation
Dina AA Abdullah1, Sahar AH Al-Sharqi2*, Hazima mossa ALabassi1, Mahmood SWahab3 and Mohammad Saeed Almishhadany3
*Correspondence: Sahar AH Al-Sharqi, Department of Biology, College of Sciences, Mustansiriyah University, Iraq, Email:
Abstract
Introduction: Osteoarthritis (OA) is a biomechanical process in which the joints respond pathologically to mechanical stress, leading to articular cartilage damage and changes in other tissue. The present study focuses on some hematological and inflammatory indicators in both patients and control and histopathological change in the knee and hip of OA patients. Methods: Tissue samples were obtained from 50 OA patients (25 knee and 25 hip) during knee and hip replacement for histopathological study and 25 as control group for hematological and immune factors analysis. The tissue and blood samples were collected during the period October 2019 to April 2020. Results: the Histological study of knee and hip OA tissues (Femoral bone tissue and bone marrow tissue) expressed many histopathological changes such as fibrin deposition, congestion of blood vessels, and infiltration of inflammatory cells. There was no significant difference in concentration of Lymphocytes, Monocytes, and Neutrophils between control and tested groups as well there is no significant difference between tested groups in the patients group. Our results showed significant elevation in erythrocyte sedimentation rate (ESR) there was a significant difference in concentration of (ESR) between control and tested groups while there is no significant difference between tested groups in the patients group. While, there was a significant difference in concentration of C- reactive protein (CRP) between control and tested groups while there is no significant difference between tested groups in patients group. Conclusions: Histopathological, Hematological, and Immune factors are all associated with the progression of OA disease.
Keywords
Osteoarthritis, Femoral bone, Bone marrow, Knee, Hip
Introduction
The knee joint is the largest and most heavily charged human body joint. The knee joint interacts with bone, cartilage, meniscus, joint capsule, ligaments, muscles, and tendons in a special way to provide stability and mobility [1].The hip joint is the joint between the hemispheric head of the femur and the cup-shaped acetabula of the hip bone. It is a strong, stable multi-axial ball-and socket type of synovial joint. The hip joint is built for flexibility over a wide variety of movements [2].
Osteoarthritis (OA) is the most widespread degenerative joint condition characterized by gradual damage to the articular cartilage, osteophyte formation and alterations of the subchondral bone [3]. OA is characterized by degradation of articular cartilage, bone hypertrophy at the margins, subchondral sclerosis [4]. Pathological alterations in the late stage of OA include softening, ulceration and focal disintegration of the joint cartilage [5]. Typical clinical symptoms include discomfort, particularly after sustained exercise and weight loss, whereas stiffness is experienced after inactivity [6]. The current study investigates histopathological, hematological, and immunological factors changes in knee and hip OA patients.
Materials and Methods
Study has been designed upon Iraqi patients with OA in the Nursing home hospital and Ghazy Al-hariri hospital for surgical specialties/Medical city during the period from October 2019 to April 2020. Subjects involved in this study include 50 patients, which diagnosed as OA, and 25 as control.
Collection of blood samples
From each 50 patients and 25 control, 7 ml of venous blood was collected from a suitable vein. 3 ml of the blood was transferred to sterile Ethylene diaminetetra acetic acid (EDTA) tubes, 4 ml of blood was used to remove serum, which was insulated by centrifugation at 3000 rpm for 5 minutes, and then collected at -20°C until the period of using it.
Tissue collection
Tissue specimens were obtained during operation involving total replace knee and hip in 50 patients with OA (25 knee and 25 hip) diagnosed by a professional doctor. OA patient’s age ranged 35-90 year. The tissue specimens collected were conserved in the fixative solution (formalin10%) for histopathological study which are routinely stained with Hematoxylin and Eosin [7]. Histopathological study was conducted at Mustansiriyah University in the laboratories of Biology department.
The statistical analysis
The data collected were subjected to a one-way variance analysis (ANOVA) test to compare different groups with each other, and values of p>0.05 were considered statically non- significant while p<0.05, <0.01and <0.001 were considered significantly different and highly significantly different. The statistical analysis was carried out by SPSS (V.20).
Results
Histopathological study
Knee tissues
Femoral bone tissue
The results of the histological examination of the sections stained with hematoxylin-eosin stain of the femoral bone tissue in the knee in OA patients indicated that several changes occurred, showed osteocytes death in many areas and abnormal controlling and proliferation of osteocytes (Figure 1A) dilated vascular sinuses with congestion of blood vessels (Figure1B) and necrotic bone cells and empty osteocytic lacunae (Figure 1C).
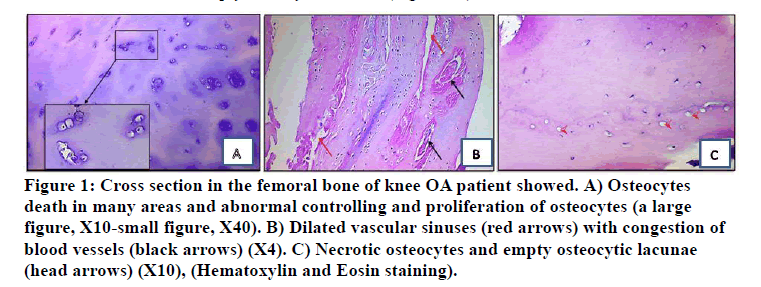
Figure 1: Cross section in the femoral bone of knee OA patient showed. A) Osteocytes death in many areas and abnormal controlling and proliferation of osteocytes (a large figure, X10-small figure, X40). B) Dilated vascular sinuses (red arrows) with congestion of blood vessels (black arrows) (X4). C) Necrotic osteocytes and empty osteocytic lacunae (head arrows) (X10), (Hematoxylin and Eosin staining).
Bone marrow tissue
Histological sections of f bone marrow tissue in osteoarthritis patients showed in the knee stained with the hematoxylin-eosin stain displayed a number of noncharacteristic abnormalities including (Figure 2A) increase in adipose tissue in the bone marrow and decreased cellular portion (Figure 2B) and increase in granulocytes and decrease in erythroid cells.
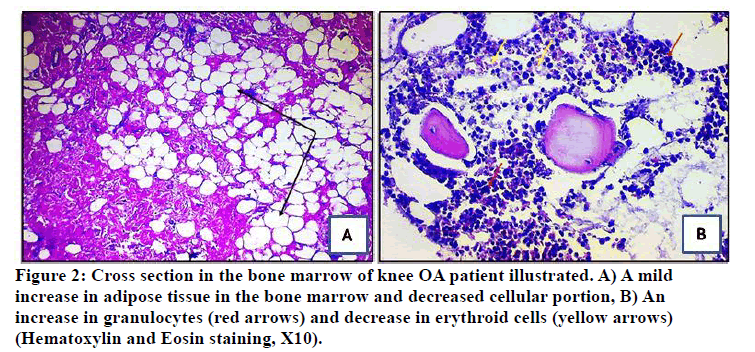
Figure 2: Cross section in the bone marrow of knee OA patient illustrated. A) A mild increase in adipose tissue in the bone marrow and decreased cellular portion, B) An increase in granulocytes (red arrows) and decrease in erythroid cells (yellow arrows) (Hematoxylin and Eosin staining, X10).
Hip tissues
Femoral bone tis sue
The results of the histological examination of the sections stained with hematoxylin-eosin stain of the femoral bone tissue in the hip in osteoarthritis patients indicated that several changes occurred, including showed apoptotic osteocytes with condensed nuclei and fragmented chromatin osteocytes (Figure 3A), death in many areas and abnormal controlling and proliferation of osteocytes (Figure 3B). Also, lacunae housing the shrunken remains of osteocytes with increased fibrocytes in outer layers and osteogenic cells in inner layers of Periosteum (Figure 3C).
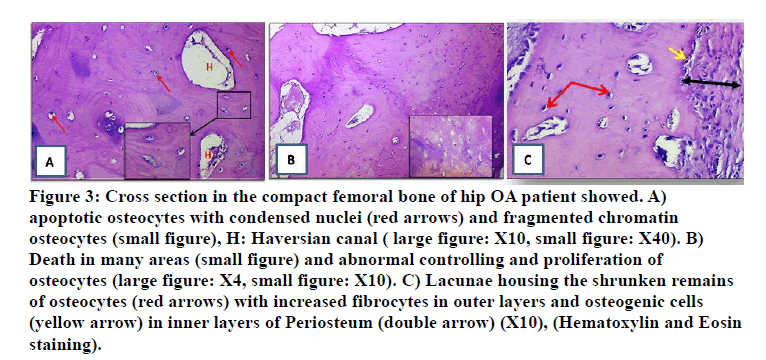
Figure 3: Cross section in the compact femoral bone of hip OA patient showed. A) apoptotic osteocytes with condensed nuclei (red arrows) and fragmented chromatin osteocytes (small figure), H: Haversian canal ( large figure: X10, small figure: X40). B) Death in many areas (small figure) and abnormal controlling and proliferation of osteocytes (large figure: X4, small figure: X10). C) Lacunae housing the shrunken remains of osteocytes (red arrows) with increased fibrocytes in outer layers and osteogenic cells (yellow arrow) in inner layers of Periosteum (double arrow) (X10), (Hematoxylin and Eosin staining).
Bone marrow tissue
The results of the histological examination of the sections stained with hematoxylin-eosin stain of the bone marrow in the hip in OA patients indicated that several changes occurred, including increased formation of erythroid and granulocytes (Figure 4A), hypo cellular areas contain increased reticular strom (Figure 4B) and an increase in the number of megakaryocytes with a mild decrease in bone marrow hematopoietic cellular density (Figure 4C).
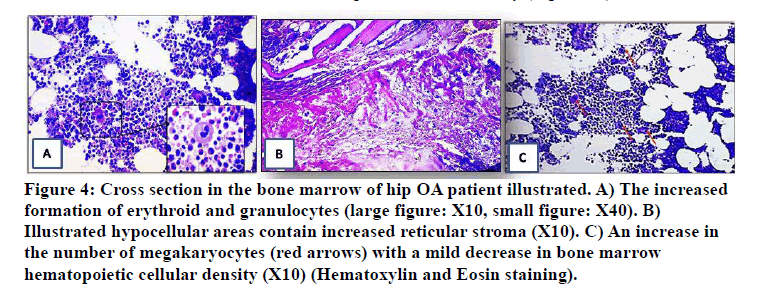
Figure 4: Cross section in the bone marrow of hip OA patient illustrated. A) The increased formation of erythroid and granulocytes (large figure: X10, small figure: X40). B) Illustrated hypocellular areas contain increased reticular stroma (X10). C) An increase in the number of megakaryocytes (red arrows) with a mild decrease in bone marrow hematopoietic cellular density (X10) (Hematoxylin and Eosin staining).
Blood cells count
The result of present study of count blood cells showed in Table 1. The lymphocytes count in knee and hip OA patients were 2.60 ± 1.00 103/ μl) and 2.31 ± 1.15 10³/ μl),respectively as compared with control group was 2.12 ± 0.61 10³/ μl).Our result of lymphocyte level was nonsignificant difference (p > 0.05) in knee and hip OA patients when compared with control group, while no significant difference (p >0.05) between knee and hip OA patients. While monocytes in knee and hip OA patients were 0.41 ± 0.20 10³/ μl and 0.48 ± 0.31 10³/ μl respectively as compared with control group was 0.70 ± 0.18 10³/ μl. Our result of monocytes level were nonsignificant difference (p > 0.05) in knee and hip OA patients when compared with control group, while no significant difference (p>0.05) between knee and hip OA patients.
Table 1: Distribution the level of blood cell distributed in knee and hip OA patients and control group.
| Parameters 10³/ µl | Mean ± SE |
|---|---|
| Lymphocytes knee | 2.60 ± 1.00 |
| Lymphocytes Hip | 2.31 ± 1.15 |
| Control | 2.12 ± 0.61 |
| P value between control and tested groups | NS |
| P value between tested groups | NS |
| Monocytes Knee | 0.41 ± 0.20 |
| Monocytes Hip | 0.48 ± 0.31 |
| Control | 0.70 ± 0.18 |
| P value between control and tested groups | NS |
| P value between tested groups | NS |
| Neutrophils Knee | 4.32 ± 0.34 |
| Neutrophils Hip | 4.13 ± 0.91 |
| Control | 4.10 ± 0.6 |
| P value between control and tested groups | NS |
| P value between tested groups | NS |
SE=Standard Error, NS=No Significant , OA=Osteoarthritis
Normal value Lymphocyte, 1.5-3.5 10³/ µl
Normal value Monocyte, 0.5-1 10³/ µl), Normal value Neutrophil, 2.5-7.5 10³/ µl
In addition, the count of the Neutrophils in knee and hip OA patients were 4.32 ± 0.34 10³/ μl and 4.13 ± 0.91 10³/ μl respectively as compared with control group was 4.10± 0.6 10³/ μl. Our result of Neutrophil level was nonsignificant difference (p > 0.05) in knee and hip OA patients when compared with control group, while no significant difference (p >0.05) between knee and hip OA patients.
CRP test
The level of CRP in serum showed an increase in knee and hip OA patients when compared with control group (Table 2). As the mean value of CRP in knee and hip OA patients were found to be 17.16 ± 2.7mg\l and 16.41 ± 2.3mg\l respectively, and in control group was 0.00 ± 0.0mg\l. Statistically a highly significant (p<0.05) increased was found in level of CRP between knee and hip OA as compared with control, while no significant difference (p 0.05) in level of CRP of Knee OA as compared with hip OA patients group.
Table 2: Distribution of sample studies according to CRP result of knee and hip OA patients and control group.
| Study groups (mg/l) | Mean ± SE |
|---|---|
| CRP Knee OA | 17.16 ± 2.7 |
| CRP Hip OA | 16.41 ± 2.3 |
| Control | 0.00 ± 0.00 |
| P value between control and tested groups | 0.001 |
| P value between tested groups | NS |
SE=Standard Error, NS=No Significant , OA=Osteoarthritis
CRP=C-reactive protein, Normal value of CRP = 5 <mg/l
ESR test
The result of present study showed a highly significant elevation level of the ESR in knee and hip OA patients was 47.12 ± 5.9 mm\h and 44.68 ± 4.2 mm\h respectively as compared with control group was 11.04 ± 0.49 mm\h. Our result of ESR level was with a significant difference (p<0.05) in knee and hip OA patients when compared with control group, while no significant difference (p>0.05) between knee and hip OA patients (Table 3).
Table 3: Distribution of sample studies according to ESR in knee and hip OA patients and control group.
| Study groups (mm\h) | Mean ± SE |
|---|---|
| ESR Knee OA | 47.12 ± 5.9 |
| ESR Hip OA | 44.68 ± 4.2 |
| Control | 11.04 ± 0.49 |
| P value between control and tested groups | 0.001 |
| P value between tested groups | NS |
SE=Standard Error, NS=No Significant , OA=Osteoarthritis
ESR=Erythrocyte sedimentation rate
Normal value of ESR=(1 -15 mm\h)
Discussion
Histopathological Study
Knee tissues
Femoral bone tissue
The phenotypes can changes s in bone cells (osteoblasts, osteocytes and osteoclasts) with the progression of OA. Aberrant intercellular communications among bone cellbone cell and bone cell-chondrocyte are of great importance and might be the factors promoting OA development meanwhile the death of osteocytes is recorded increases in cases of OA increase in immature osteocytes, specifically in regions of active bone formation and MSC accumulation in OA bone [8]. The importance of osteocytes is in the regulation of bone remodelling, osteocytes regulate bone turnover by acting on bone-forming osteoblasts and bone-resorbing osteoclasts. In addition, osteocytes directly participate in osteolysis, control phosphate homeostasis, and functionally act on the neighboring skeletal muscle and distant organs, the functional and morphological properties of osteocytes appear to be hampered in patients with OA, Indicates that these cells may play an important pathological role in subchondral osteosclerosis [9-11]. Osteocytes die as a result of micro damage or a lack of mechanical stimulus as a result of disuse or weightlessness, which stimulates the recruitment and/or differentiation of osteoclast precursors to the sites of osteocyte apoptosis [12]. On the other hand, a progressive alteration in the subchondral bone is a characteristic of advanced OA, where bone formation leads to the development of osteophytes [13]. Osteophyte formation is significantly correlated with disease progression, and increased local joint space narrowing is associated with increased osteophyte size [14].
Bone marrow tissue
One of the key changes in bone marrow in patients with knee osteoarthritis is bone marrow fibrosis and necrosis, trabecular bone abnormalities and increased inflammatory cells in sclerotic subchondral bone close to areas of severe cartilage loss, which are known to contain abundant bone marrow, consequently, bone marrow can be regarded as resulting from increased remodelling of subchondral bone and bone marrow [15]. On the other hand, an increase in lesion size strongly associates with progressive cartilage loss and development of OA .Conversely, absence or regression over time of bone marrow is associated with a reduced risk of cartilage loss [16]. There were several fat vacuoles and small blood vessels (sinusoids and venules) often showed erythrocyte aggregation and agglutination. The bone marrow was replaced by fibrous tissue in large areas, The vessels in the Haversian canals were usually open, but areas of erythrocyte agglutination and fibrin thrombi of different ages were not uncommon. Generally, the differences observed in in rheumatoid bone marrow resembled those found in arthritis, except for large aggregations of mononuclear inflammatory cells, sometimes adjacent to vessels clogged [17,18].
Hip tissues
Femoral bone tissue
Osteocyte death occurs as a result of ageing, after the menopause, reduced bone loading and the death of osteocytes is strongly associated with bone resorption, On the other hand, lack of Mechanical loading to apoptosis of osteocytes by oxygen deprivation. It appears that mechanical stimulation provides essential oxygen levels to keep osteocytes viable [19]. Apoptosis of mature osteoblasts is influenced by cytokines such as IL-6 and TGF-β1 , but survival and differentiation of osteoblast into osteocyte was dependent on (matrix metalloproteinase) activity [20]. On the other hand, the current result suggest that the fibrin deposition usually need for mechanical assistance by an increase of osteoclast activity in the in outer circumferential bone lamella in order to causes interruptions in the tidemark with the presence of bony channels carrying inflammatory cells and blood vessels and deposition of blood content involve fibrin this suggestion was explored [21].
Bone marrow tissue
Bone marrow is a source of osteoprogenitor cells, which are key elements in bone formation and fracture healing [22]. An early explanation for the development of Bone marrow considered increased flow and vascular congestion in the setting of capillary wall changes or increased intravascular pressure. It was thought that these factors and the resulting vascular leakage would lead to Bone marrow development [23]. In addition, bone marrow lesion has reliably been shown to correlate with bone marrow necrosis and fibrosis in OA human knees and hips [24]. This result revealed many of changes that associated with OA, such changes are recorded [25] who mentioned that the bone marrow fibrosis, necrosis, swollen/dying adipocytes, and alterations in trabecular bone structure. Our result contrary to studies of [26] that revealed that the changes of fluid dynamics at subchondral bone represents a part of the mechanism the fluid flow lead to OA and bone marrow.
Blood cells count
The results obtained in the present study showed that there is no effect of OA disease on lymphocytes count, because there is no change in lymphocyte count in that blood. Study of [27] showed that, in the severe knee OA, blood neutrophil, lymphocytes ratio levels found to be elevated when compared to mild to moderate knee OA. The study of [28] reported that, the infiltration into the synovium activation T and B cells and the increased expression of pro inflammatory mediator in both early and late stage of OA which consistent with the current histopathological study [29]. Showed that, T cell may play an important role in the pathogenesis and progression of OA [30] reported the recruited of lymphocyte to the site of inflammation at the late stages of chronic inflammation.
The Monocytes contribute to pathogenesis in OA Lowgrade inflammation occurs in OA and correlates with disease severity and progression [31]. A high count of monocyte can be result of several causes, and one of them is acute inflammation, when monocyte increases it indicate that, the body is trying to fight certain diseases [32,33] reported the increase of monocyte, macrophage cells in 24 to 48 hours in most form of acute inflammation, also the chronic inflammation primarily mediated by monocyte and macrophage. It is assumed that the circulating of high numbers of monocyte was occur as a migration of large number of cells into damaged tissues in response to inflammatory signal [34]. When monocytes migrate out of the blood and into peripheral tissue, they immediately undergo to a phenotypic change to aid with the inflammatory response [35].
The neutrophil ratio level as inflammatory marker for indicating the severity of OA [36]. Neutrophils rapidly respond to chemokine’s, predominate in the inflammatory infiltrate during 6 to 24 hours [33]. Also it possibly mediates monocyte/macrophage function [37]. After the injury neutrophils, mast cell and macrophages recruited to involved area and can produce variety of pro inflammatory cytokines [38].
CRP test
In this study, all of newly diagnosed OA patients were positive for CRP, this result showed association between CRP and OA were in agreement with the study of [39], CRP is an acute phase protein in synthesized by hepatocytes that stimulates the tumor necrosis factor TNF-a and fibrinogen that leads to high erythrocytes and stimulates the production of (IL-1),which increases the production of white blood cells and stimulates T cells, and it consider as an e evidence of the severity of the inflammation [40].
ESR test
The ESR is the most commonly used laboratory tests for detecting the acute inflammation [41] and thus diagnosis and monitoring of inflammatory conditions. This study demonstrated the increased ESR levels in OA patients compared to controls, suggesting the presence of an inflammatory response by the immune system against OA [42]. Previous finding demonstrated higher ESR levels in OA patients compared to controls. The failure of various treatments to reverse normalize ESR value is suggestive of presence other mechanisms responsible for the pathogenesis of OA [27].
Conclusion
Histopathological changes in Femoral bone and Bone marrow in knee and hip OA patients occurred with the progression of OA disease. The histopathological changes showed the functional and morphological properties of osteocytes appear to be hampered in patients with OA, indicates that these cells may play an important pathological role in OA. Also, the aggregation of inflammatory cells in tissues, thus reflect the role of these cells in inflammatory response. In addition, increase fibrin deposition in much area of tissues. On the other hand, an increase in ESR in OA patients which reflect the present of chronic inflammation in the pathology of OA. While increased CRP in OA patients might be related to present of inflammatory response.
References
- Gao S, Hao B, Yang XF, et al. Decreased CD200R expression on monocyte-derived macrophages correlates with Th17/Treg imbalance and disease activity in rheumatoid arthritis patients. Inflammation Res 2014; 63:441-50.
- Attum B, Varacallo M. Anatomy, bony pelvis and lower limb, thigh muscles. StatPearls Publishing 2018.
- Moore KL, Dalley AF, Agur AM. Clinically oriented anatomy. Lippincott Williams & Wilkins 2013.
- Chen DI, Shen J, Zhao W, et al. Osteoarthritis: Toward a comprehensive understanding of pathological mechanism. Bone Res 2017; 5:1-3.
- Pain SW. Targeting pain or osteoarthritis? Implications for optimal management of osteoarthritis pain. Pain 2016.
- Giri P. The effect of mulligan technique in comparison with maitland mobilization and kinesio taping in patients with Osteoarthritis of knee joint. J Physio 2019; 1:42-60.
- Suvaran SK, Layton C, Bancroft JD. Bancroft's theory and practice of histological techniques. Eight edition, Churchill livingstone Elsevier 2019.
- Rabelo GD, Vom Scheidt A, Klebig F, et al. Multiscale bone quality analysis in osteoarthritic knee joints reveal a role of the mechanosensory osteocyte network in osteophytes. Scientific Reports 2020; 10:1-2.
- Prasadam I, Farnaghi S, Feng JQ, et al. Impact of extracellular matrix derived from osteoarthritis subchondral bone osteoblasts on osteocytes: role of integrinβ1 and focal adhesion kinase signaling cues. Arthritis Res Therapy 2013; 15:1-4.
- Klaewklad A, Nakkanong K, Nathaworn CD, et al. Rubber elongation factor (REF) and small rubber particle protein (SRPP) gene expression responses to variation of seasonal change in four selected rubber clones. Pakistan J Biotechnol 2017; 14:115-20.
- Rabelo GD, Vom Scheidt A, Klebig F, et al. Multiscale bone quality analysis in osteoarthritic knee joints reveal a role of the mechanosensory osteocyte network in osteophytes. Scientific Reports 2020; 10:1-2.
- Intemann J, De Gorter DJ, Naylor AJ, et al. Importance of osteocyte-mediated regulation of bone remodelling in inflammatory bone disease. Swiss Med Weekly 2020; 150.
- Lories RJ, Luyten FP. The bone–cartilage unit in osteoarthritis. Nature Reviews Rheumatol 2011; 7:43-49.
- Murata K, Kokubun T, Onitsuka K, et al. Controlling joint instability after anterior cruciate ligament transection inhibits transforming growth factor-beta-mediated osteophyte formation. Osteoarthritis Cartilage 2019; 27:1185-96.
- Hügle T, Geurts J. What drives osteoarthritis?—synovial versus subchondral bone pathology. Rheumatol 2017; 56:1461-71.
- Perry TA, Parkes MJ, Hodgson RJ, et al. Association between Bone marrow lesions & synovitis and symptoms in symptomatic knee osteoarthritis. Osteoarthritis Cartilage 2020; 28:316-23.
- Scher C, Craig J, Nelson F. Bone marrow edema in the knee in osteoarthrosis and association with total knee arthroplasty within a three-year follow-up. Skeletal Radiol 2008; 37:609-17.
- Muratovic D, Cicuttini F, Wluka A, et al. Bone marrow lesions detected by specific combination of MRI sequences are associated with severity of osteochondral degeneration. Arthritis Res Therapy 2016; 18:1-1.
- Doolittle ML. Dissecting the genetic influences on osteoporosis reveals Zbtb40 as a novel regulator of osteoblast function. Doctoral dissertation, University of Rochester 2020.
- Ali AA, Al-Attar AS, Refat NA, et al. Synergistic effect of nanocurcumin and platelet rich plasma on resolving experimentally induced osteoarthritis in albino rats. Adv Anim Vet Sci 2021; 9:26-34.
- Mapp PI, Walsh DA. Mechanisms and targets of angiogenesis and nerve growth in osteoarthritis. Nature Rev Rheumatol 2012; 8:390-8.
- Tomaru Y, Yoshioka T, Sugaya H, et al. Hip preserving surgery with concentrated autologous bone marrow aspirate transplantation for the treatment of asymptomatic osteonecrosis of the femoral head: retrospective review of clinical and radiological outcomes at 6 years postoperatively. BMC Musculoskeletal Disorders 2017; 18:1-8.
- Starr AM, Wessely MA, Albastaki U, et al. Bone marrow edema: Pathophysiology, differential diagnosis, and imaging. Acta Radiol 2008; 49:771-86.
- Campbell TM, Churchman SM, Gomez A, et al. Mesenchymal stem cell alterations in bone marrow lesions in patients with hip osteoarthritis. Arthritis Rheumatol 2016; 68:1648-59.
- Zanetti M, Bruder E, Romero J, et al. Bone marrow edema pattern in osteoarthritic knees: correlation between MR imaging and histologic findings. Radiology 2000; 215:835-40.
- Aaron RK, Dyke JP, Ciombor DM, et al. Perfusion abnormalities in subchondral bone associated with marrow edema, osteoarthritis, and avascular necrosis. Annals New York Academy Sciences 2007; 1117:124-37.
- Taşoğlu Ö, Şahin A, Karataş G, et al. Blood mean platelet volume and platelet lymphocyte ratio as new predictors of hip osteoarthritis severity. Medicine 2017; 96.
- Nanus DE, Badoume A, Wijesinghe SN, et al. Identification of synovial fibroblasts subsets associated with pain and progression of knee osteoarthritis by single cell sequencing. Osteoarthr Cartilage 2020; 28:S133.
- Könnecke I, Serra A, El Khassawna T, et al. T and B cells participate in bone repair by infiltrating the fracture callus in a two-wave fashion. Bone 2014; 64:155-65.
- Zhu W, Zhang X, Jiang Y, et al. Alterations in peripheral T cell and B cell subsets in patients with osteoarthritis. Clin Rheumatol 2020; 39:523-32.
- Loukov D, Karampatos S, Maly MR, et al. Monocyte activation is elevated in women with knee-osteoarthritis and associated with inflammation, BMI and pain. Osteoarthr Cartilage 2018; 26:255-63.
- Raghu H, Lepus CM, Wang Q, et al. CCL2/CCR2, but not CCL5/CCR5, mediates monocyte recruitment, inflammation and cartilage destruction in osteoarthritis. Annals Rheumatic Diseas 2017; 76:914-22.
- Finn A. Biochemical biomarkers at the site of inflammation and in peripheral blood. Physiol Pharmacol 2015.
- Varol C, Yona S, Jung S. Origins and tissue‐context‐dependent fates of blood monocytes. Immunol Cell Biol 2009; 87:30-8.
- Gregory C. Sent by the scent of death. Nature 2009; 461:181-2.
- Koca TT, Baykara M, Koçyiğit BF. Relation of complete blood count parameters and derivatives with radiologic staging of knee osteoarthritis. Cukurova Med J 2019; 44:1364-70.
- Soehnlein O, Lindbom L, Weber C. Mechanisms underlying neutrophil-mediated monocyte recruitment. Blood 2009; 114:4613-23.
- Marchand F, Perretti M, McMahon SB. Role of the immune system in chronic pain. Nature Reviews Neurosci 2005; 6:521-32.
- Xu C, Guo H, Qu P, et al. Preoperatively elevated serum inflammatory markers increase the risk of periprosthetic joint infection following total knee arthroplasty in patients with osteoarthritis. Therapeutic Clin Risk Management 2018; 14:1719.
- Shadyab AH, Terkeltaub R, Kooperberg C, et al. Prospective associations of C-reactive protein (CRP) levels and CRP genetic risk scores with risk of total knee and hip replacement for osteoarthritis in a diverse cohort. Osteoarthr Cartilage 2018; 26:1038-44.
- Lapić I, Padoan A, Bozzato D, et al. Erythrocyte sedimentation rate and C-reactive protein in acute inflammation: Meta-analysis of diagnostic accuracy studies. Am J Clin Pathol 2020; 153:14-29.
- Bray C, Bell LN, Liang H, et al. Erythrocyte sedimentation rate and C-reactive protein measurements and their relevance in clinical medicine. Wmj 2016; 115:317-21.
Author Info
Dina AA Abdullah1, Sahar AH Al-Sharqi2*, Hazima mossa ALabassi1, Mahmood SWahab3 and Mohammad Saeed Almishhadany3
1Department of Biology, College of Education Ibn Al-Haitham, Baghdad University, Baghdad, Iraq2Department of Biology, College of Sciences, Mustansiriyah University, Baghdad, Iraq
3Nursing Home Hospital, Medical City Complex, Ministry of Health, Baghdad, Iraq
Citation: Dina AA Abdullah, Sahar AH Al-Sharqi, Hazima mossa ALabassi, Mahmood SWahab, Mohammad Saeed Almishhadany,Evaluation Pathogenesis Outcomes of Knee and Hip in Patients with Osteoarthritis Based on: Histopathological, Hematological, and Indicators of Inflammation, J Res Med Dent Sci, 2021, 9(8): 178-184
Received: 16-Jul-2021 Accepted: 13-Aug-2021
