Research - (2022) Volume 10, Issue 2
Exploration and Understanding of Lifestyle Modification with Conservative Treatment in Polycystic Ovarian Syndrome among Females Seeking Management for Primary Infertility
Sana Tariq1*, Lubna Razzak2, Najia Bhatti3, Basma Zia Isran3, Syeda Sarah Batool4, Sarah Siddiqui5, Syeda Alisha Johar6 and Saadia Siddiqui7
*Correspondence: Sana Tariq, Public Health Scientist, Pakistan, Email:
Abstract
Introduction: PCOS is a major endocrinological syndrome that affects females and impairs hormonal stability thus having an impact on the normal functioning of some body systems. This has affected 6-20% of the female population min reproductive age and hence its diagnosis is important. Methods: This is a prospective cohort study. A total of 151 females were enrolled, asked about menstruation history, signs and symptoms of polycystic ovarian disease, and reproductive health. Educated about weight loss, lifestyle modifications, and initiated consulted first-line conservative treatment, all the aspects were reevaluated after 4 months for results. The data was analyzed in the statistical package of social sciences (SPSS) version 2021. Result: Lifestyle preferences indicated low to none physical activity and increased basal metabolic index in 85.4% of study participants, 60.9% were facing irregular periods, heavy bleeding was experienced by 16.6% participants.. 41.7% knew that lifestyle modification can help reduce adverse effects of the syndrome. After lifestyle modification, 68.9% indicated menstruation regularity, and 64.9% conceived without any medical intervention. Overall 79.5% of improvement in symptoms was recorded after the intervention, a total of 23.7% were taking medicines for insulin resistance, and 53.5% had a positive family history of diabetes and obesity. Conclusion: Lifestyle choices adopted by childbearing-aged females of Pakistan may predispose them to disorders including PCOS and infertility, early detection, proper management, and lifestyle modification including weight reduction, lower stress, and healthy diet improved menstruation regularity, and participants conceived without medical intervention.
Keywords
Lifestyle Modification, Polycystic ovarian syndrome
Introduction
Polycystic ovarian syndrome is an endocrinological impairment that affects 6-20% of women of Reproductive age ranging from 15 years to 49 years, making it the most debatable gynaecological disorder in the developing world [1]. In this syndrome, the usual levels and functions of hormones are constantly impaired which affect ovaries and maintenance of regular menstrual cycles [2]. Polycystic ovarian syndrome (PCOS) is widespread globally; In Pakistan, the prevalence rate has been recorded as 52%, the reason behind higher incidence rates are late detection of disease, rare medical follow-up and decreased knowledge of lifestyle modification impact. the prevalence of PCOS in western countries are notably low, 20-25% in the United Kingdom and 4-12% in the united states [3], The awareness of PCOS and its associated risk factors are low, in the US 7 million women with PCOS only half of them is mindful that they have this syndrome. Insufficient knowledge leads to the progression of disease and late diagnosis, the young Pakistani female population has little awareness regarding this syndrome, 22% rise in incidences has been recorded in the past 05 years [4]. Hereditary factors, environmental factors, and consanguineous marriage can be the reason behind the escalating occurrence of PCOS [5]. The ultimate reason behind infertility is raised androgen and luteinizing hormone levels and PCOS is currently the leading cause of infertility in women. It is further characterized by irregular menstrual cycles, hirsutism, acne & seborrhea [6,7] PCOS is related remarkably with BMI indicating obesity, paired with dysglycemia, DM type 2, and metabolic syndrome still it is not diagnosed thus restricting the chances of precautionary majors and its management [8-10]. 30% to 40% of women who are suffering from PCOS have glucose intolerance and are unresponsive to the insulin that causes hyperinsulinaemia via feedback mechanism as body’s response to regulate blood glucose levels and approximately 10% are prone to have insulinindependent diabetes in their 40s [11]. It is commonly observed as being the potent instigator of impaired glucose tolerance, elevated insulin levels, heart disease, and high blood pressure. The occurrence of surplus weight in PCOS lies in the span of 30-75% and fattening up has detrimental effects on individuals and their symptoms are exacerbated [12] also expected to increase the possibility of cardio metabolic disorders, as significant half of the population of females with PCOS are obese. Hormonal imbalance in PCOS lays its effects on the psychological wellbeing of a person and thus affects the quality of life. Psychological impairment manifests as depression, anxiety, stress, low self-esteem, negative body image & psychosexual dysfunction. The occurrence of endometrial cancer increases three folds in individuals with PCOS [13]. Wide range of treatment options has been evaluated for PCOS, including lifestyle modification [14], weight reduction [15] to conservative management with decreasing symptoms of PCOS, metformin for insulin resistance and folic acid, inositol intake for better ovum quality [16]. Ovulation induction for ovulatory patients with clomiphene citrate and letrozole are popular too. Invasive treatment options range from cyst excision to enhance ovulation chances and intrauterine insemination (IUI), to in-vitro fertilization (IVF) [17].
This study aims to assess the effect of lifestyle modification, weight reduction, stress reduction, and healthy diet along with first-line conservative management in diagnosed polycystic ovarian syndrome patients, upon polycystic ovarian syndrome symptoms, infertility, and quality of life.
Method
This is a cross-sectional, cohort study; the survey continued for 3 months ranging from August2021 till October 2021, 151 females diagnosed with polycystic ovarian syndrome and seeking treatment for primary infertility were enrolled in the study. After signing informed consent, demographic data was gathered by a prestructured validated questionnaire, The questionnaire contains two different sections, section A has Demographic questions including Age, weight, basal metabolic index, duration of PCOS diagnosis, duration of infertility, medical history, and lifestyle pattern, while Section B contains questions about details of the menstrual history and PCOS symptoms and perceived stress access to evaluate stress severity of study participants. Upon consultation with a consultant gynaecologist, patients were prescribed first-line conservative treatment, nutritionist counselled for healthy diet pattern and primary investigator educated the participants about lifestyle modification, stress reduction, and weight reduction. After 3 months of consecutive communication, patients were asked to visit outpatient department again, results were compared after three months. Successful weight reduction, declining of symptoms, improvement in menstrual regularity, and conception was analyzed. The data were analyzed in a statistical package of social sciences (SPSS) version 2021.Demographic detail such as age weight height and BMI are analyzed as descriptive variables and interpreted in mean and standard deviation methods. Independent variables were analyzed in frequencies and percentages. To compare the pre-intervention and postintervention paired sample t-test and multivariate regression was performed, the significance of data was analyzed with chi-square test, p-value<0.05 considered significant.
Results
The mean age value of the participants is 22.2 ± 1.9 years. Upon enrolment, the medical history including age at menarche, and duration of infertility explained as the duration of trying to conceive or having unprotected sex was asked and meantime was 2.5 ± 0.8 years and mean age at menarche was 11.5 ± 4.8 years, while the duration of PCOS diagnosis was 1.2 ± 0.4 years. After diagnosis, consultant health care provider prescribed conservative first-line treatment, every patient was recommended to take 400μcg of folic acid once a day, only134 (88.7%) were prescribed to take metformin (1000-1500mg /day), Inositol was prescribed to 71 (47%) participants while only 48 (31.7%) females were requested to take Progesterone to get menstrual cycle after 3 months of absence. Other than medical advice, a few recommendations were to reduce weight, enhance physical activity with mild exercise and improve diet patterns and food choices to participants after detailed consultation. A psychological assessment for stress was taken, perceived stress scale was used to assess the severity of stress in study participants, 73 (48.3%) indicated mild stress, while 41 (27.1%) showed signs of moderate stress, only 7 (4.6%) showed severe stress symptoms and referred to a psychologist for consultation. Mild and moderate stress indicated participants were educated for stress management and perception management for better-coping skills (Table1).
| Variables | Mean SD/n(%) | |
|---|---|---|
| Descriptives and Diagnosis | Age (years) | 22.2 ± 1.9 |
| Menarche age (years) | 11.5 ± 4.8 | |
| Duration of infertility (years) | 1.5 ± 0.8 | |
| Duration of PCOS diagnosis (years) | 1.2 ± 0.4 | |
| Medication | Folic acid | 151 (100%) |
| Metformin | 134 (88.7%) | |
| Inositol | 71 (47%) | |
| Progestrone | 48(31.7%) | |
| Recommendation | Weight reduction | 92 (60.9%) |
| Exercise (Mild) | 127 (84.1%) | |
| Diet improvement | 142 (94%) | |
| Stress evaluation | Mild stress | 73 (48.03%) |
| Moderate stress | 41 (27.1%) | |
| Severe stress | 7 (4.6%) | |
Table 1: Descriptive details of study participants.
Polycystic ovarian syndrome has specific symptoms, including irregular menstrual cycle, excessive bleeding during menstruation, patches of dark skin, acne, and excessive body hair growth, these symptoms have been indicated by our study participants as 98 (64.9%), 38 (25.1%), 42(27.8%), 48(31.7%) and 72(47.6%) respectively. While after intervention the follow up results showed significant decline in symptoms with 21 (13.9%), 17 (11.2%), 33 (21.8%), 29(19.2%) and 56 (37%) of frequency respectively (Figure 1). Overall, 132(56%) of reduction in PCOS symptoms have been recorded with 104 (44%) menstrual regularity after the intervention (Figure 2). Details of pre-intervention and post-intervention differences are significant, weight reduction showed a mean value of 32.3kgs loss with a positive association with symptoms of the polycystic ovarian syndrome, mean basal metabolic index difference was 4.4, while stress difference was remarkable after the intervention, indicating 24 participants from mild stress, 20 participants from moderate stress and 5 from severe stress with the association of all variables were positive. Upon intervention with conservative management including metformin, ovulation induction and weight reduction, successful conception was recorded in 98 (64.9%) of study participants (Table 2 and Figure 3).
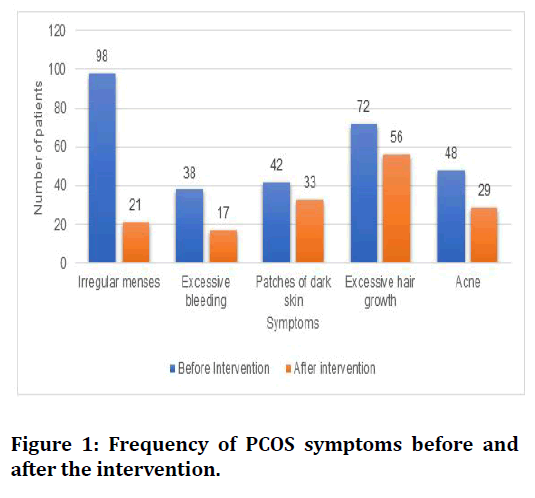
Figure 1. Frequency of PCOS symptoms before and after the intervention.
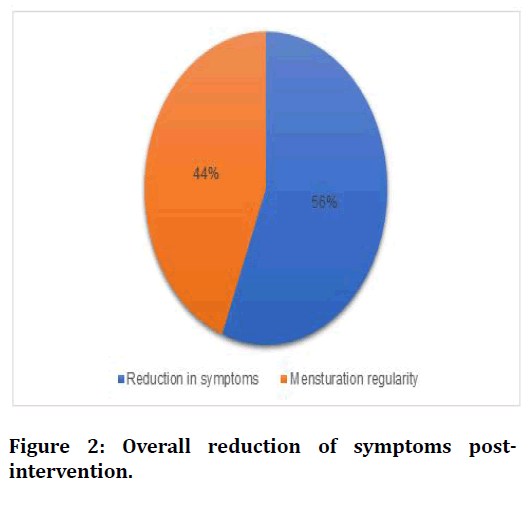
Figure 2. Overall reduction of symptoms postintervention.
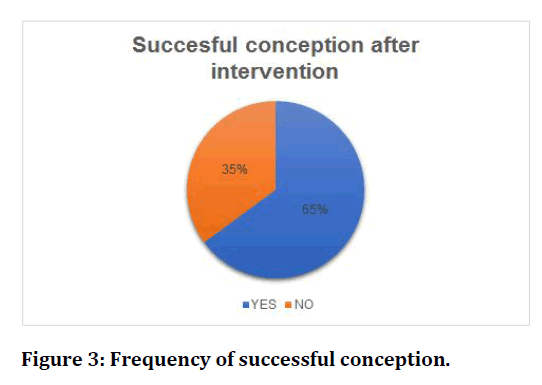
Figure 3. Frequency of successful conception.
| Variables | Pre-intervention | Post-intervention | P-Value | Odds Ratio (95% CI) |
|---|---|---|---|---|
| Weight (kg) | 124.4 ± 9.0 | 92.1 ± 8.6 | 0.02 | 4.1 (2.5-12.9) |
| BMI | 28.9 ± 4.8 | 24.5 ± 1.8 | 0.05 | 2.3 (1.8-5.4) |
| Mild stress | 73 (48.03%) | 49 (32.4%) | 0.04 | 1.3 (0.4-3.4) |
| Moderate stress | 41 (27.1%) | 21 (13.9%) | 0.09 | 1.7 (0.5-1.8) |
| Severe stress | 7 (4.6%) | 2 (1.9%) | 0.03 | 1.2 ( 0.7-2.1) |
Table 2: Difference between pre-intervention and post-intervention.
| Successful conception after conservative medication | |||
|---|---|---|---|
| Variables | Results n(%) | Odds Ratio (95% CI) | |
| Medication | Metformin | 42 (27.8%) | 3.4 (1.8-6.7) |
| Inositol | 8 (5.2%) | 0.9 (0.2-1.2) | |
| Recommendation | Weight reduction | 29 (19.2%) | 2.8 (0.9-4.2) |
| Exercise (Mild) | 9 (5.9%) | 1.1 (0.5-2.8) | |
| Diet improvement | 4 (2.6%) | 0.8 (0.1-1.7) | |
| Stress managemnt | 6 (3.9%) | 1.4 (0.8-3.4) | |
Table 3: Association of lifestyle modification along with conservative management on conception chances.
Association of recommended adaptations and conservative management with successful conception indicated that metformin increases the chances of conception by 3.4 folds, although inositol doesn’t have a positive association. Weight reduction also showed significant improvement in conception along with enhancing physical activities mildly, diet improvement doesn’t show a positive association (Table 3).
Discussion
Lifestyle modification reduces the polycystic ovarian symptoms including irregular menstruation, acne, and other related issues, and enhances the chances of conception, our study results showed significant improvement in symptoms including menstrual disturbances by 44%, while excessive blood flow during menstruation was reduced by 21, another study with similar progressive results indicated that overall lifestyle modification has a positive impact on polycystic ovarian syndrome symptoms [18-20]. Metformin increases the chances of fertility by 3.4% in study participants diagnosed with PCOS along with insulin resistance, these results have been evaluated before and indicated a positive impact of metformin as the drug of choice in many PCOS patients, metformin is known to reduce weight and regulate menstruation by managing blood glucose level [21,22]. Although the effect of inositol on the fertility of PCOS patients is still not completely evaluated, a few studies supported the treatment [23] our study results indicated a negative association of inositol treatment on fertility, the reason could be the severity of symptoms of PCOS and/or stress levels. The impact of perceived stress upon PCOS symptoms, Quality of life, and fertility have been explained in many studies, the fact that managing stress enhances the chances of fertility in females diagnosed with PCOS is known and present in literature [24], our study participants were evaluated for stress and counselled to manage stress and work on their coping skill, the fertility was enhanced in 3.9% of participants by managing stress only. Mild physical activities including exercise and weight reduction have a significant effect on fertility of PCOS patients and reduction in symptoms, importance, and methods of weight reduction were counselled to study participants and results indicated significant improvement in fertility with 19.2% inspection overall. The body fat and increased basal metabolic index is known risk factors to reduce fertility and disturb menstruation in females not diagnosed with PCOS, with PCOS diagnosis the risk enhances by2 folds [25-27]. Diet improvement has no positive effect on the fertility of study participants, the reason could be financial difficulties. A significant difference was noted after intervention in weight, BMI, and stress severity of study participants, indicating adaptation of females towards a better lifestyle and accepting the effect of lifestyle modification upon PCOS and fertility issues, the improvement after counselling has been noted after three months and indicated positive results specifically insight reduction and stress management, although diet pattern was not been followed by many participants. Previous studies have been evaluated the improvement after intervention on weight reduction and stress levels separately [28,29]. For male infertility the importance of weight management and stress management has also been evaluated and results described the vital part of stress management upon sperm quality, for females stress is known to reduce ovulation and fertilization. 98(64.9%) out of 151 study participants showed positive conception after the intervention, the results are similar to other studies conducted in other regions with 60%, 71%, and 81% of positive conception without any invasive intervention [30-32]. Limitations of the study are small sample size, with only three months of follow up, also patients were from middle socioeconomic class, studies with randomization of lifestyle modification and conservative management with metformin and ovulation induction in large sample size involving more than two socio-economic classes is recommended.
Conclusion
In our study, we concluded that weight reduction and stress management has a positive effect on PCOS symptoms management and increase the chances of conception. Conservative management of PCOS with metformin and ovulation induction can be a burden financially and emotionally for many females, lifestyle modification should be the first-line option to manage PCOS and fertility along with stress severity identification and management.
Conflict of Interest
The authors declare no conflict of interest.
References
- Dargham SR, Ahmed L, Kilpatrick ES, et al. The prevalence and metabolic characteristics of polycystic ovary syndrome in the Qatari population. PloS one 2017; 12:e0181467.
- Ajmal N, Khan SZ, Shaikh R. Polycystic ovary syndrome (PCOS) and genetic predisposition: A review article. Eur J Obstetr Gynaecol Reprod Biol 2019; 3:100060.
- Wolf WM, Wattick RA, Kinkade ON, et al. Geographical prevalence of polycystic ovary syndrome as determined by region and race/ethnicity. Int J Environ Res Public Health 2018; 15:2589.
- Sidra S, Tariq MH, Farrukh MJ, et al. Evaluation of clinical manifestations, health risks, and quality of life among women with polycystic ovary syndrome. PloS One 2019; 14:e0223329.
- Haq N, Khan Z, Riaz S, et al. Prevalence and knowledge of polycystic ovary syndrome (PCOS) among female science students of different public Universities of Quetta, Pakistan. Imperial J Interd Res 2017; 35:385-392.
- Chadha C, Kataria J, Chugh P, et al. Quality of life in young adult females with PCOS. Indian J Physiother Occup Ther 2019; 1:40-2.
- Norman RJ, Dewailly D, Legro RS, et al. Polycystic ovary syndrome. Lancet 2007; 370:685-697.
- Arif N, Khawaja S, Iqbal Q. Awareness of polycystic ovarian disease: Knowledge and presence of presenting symptoms. Pak J Med Health Sci 2020; 14:627-630.
- Khomami MB, Tehrani FR, Hashemi S, et al. Of PCOS symptoms, hirsutism has the most significant impact on the quality of life of Iranian women. PLoS One 2015; 10e0123608
- http://scientificresearchjournal.com/wp-content/uploads/2019/02/Social-Science-6_A-154-159-Full-Paper.pdf
- Khan MJ, Ullah A, Basit S. Genetic basis of polycystic ovary syndrome (PCOS): Current perspectives. Application Clin Genet 2019; 12:249.
- AlSinan A, Shaman AA. A study to measure the health awareness of polycystic ovarian syndrome in Saudi Arabia. Global J Health Sci 2017; 9:210-219
- Krul-Poel YH, Koenders PP, Steegers-Theunissen RP, et al. Vitamin D and metabolic disturbances in polycystic ovary syndrome (PCOS): A cross-sectional study. PloS One 2018; 13:e0204748.
- Kim CH, Chon SJ, Lee SH. Effects of lifestyle modification in polycystic ovary syndrome compared to metformin only or metformin addition: A systematic review and meta-analysis. Sci Rep 2020; 10:1-3.
- Calcaterra V, Verduci E, Cena H, et al. Polycystic ovary syndrome in insulin-resistant adolescents with obesity: The role of nutrition therapy and food supplements as a strategy to protect fertility. Nutrients 2021; 13:1848.
- Laganà AS, Garzon S, Casarin J, et al. Inositol in polycystic ovary syndrome: Restoring fertility through a pathophysiology-based approach. Trends Endocrinol Metabol 2018; 29:768-780.
- Sawant S, Bhide P. Fertility treatment options for women with polycystic ovary syndrome. Clin Med Insights Rep Health 2019; 13:1179558119890867.
- Park YJ, Shin H, Jeon S, et al. Development and effects of college-based lifestyle modification program for menstrual health of young adult women with irregular menses: a randomized controlled trial. Int J Environ Res Public Health 2021; 18:233.
- Afefy NA, Abd Elrehim AE. Comparing the effectiveness of herbal remedies and lifestyle modification on minimizing polycystic ovarian syndrome symptoms. Int J Dev Res 2019; 9:25965-25973.
- Hussein OS, Abd Elfattah H, Sayed EM, et al. Effect of lifestyle modifications on reliving menstrual dysfunction among women suffered from polycystic ovarian syndrome. Int J Novel Res healthcare Nurs 2021; 8:78-88.
- Guan Y, Wang D, Bu H, et al. The effect of metformin on polycystic ovary syndrome in overweight women: a systematic review and meta-analysis of randomized controlled trials. Int J Endocrinol 2020; 2020.
- Kim CH, Chon SJ, Lee SH. Effects of lifestyle modification in polycystic ovary syndrome compared to metformin only or metformin addition: A systematic review and meta-analysis. Sci Rep 2020; 10:1-3.
- Monastra G, Vucenik I, Harrath AH, et al. PCOS and inositols: Controversial results and necessary clarifications. basic differences between D-chiro and myo-inositol. Front Endocrinol 2021; 12:269.
- Damone AL, Joham AE, Loxton D, et al. Depression, anxiety and perceived stress in women with and without PCOS: A community-based study. Psychol Med 2019; 49:1510-20.
- Cena H, Chiovato L, Nappi RE. Obesity, polycystic ovary syndrome, and infertility: A new avenue for GLP-1 receptor agonists. J Clin Endocrinol Metabol 2020; 105:e2695-709.
- Albezrah NK, Arein FR. Knowledge, attitude, and practice toward weight reduction among polycystic ovary syndrome women at Taif city. Saudi J Health Sci 2019; 8:112.
- Jiskoot G, Timman R, Beerthuizen A, et al. Weight reduction through a cognitive behavioral therapy lifestyle intervention in PCOS: The primary outcome of a randomized controlled trial. Obesity 2020; 28:2134-41.
- Leisegang K, Dutta S. Do lifestyle practices impede male fertility?. Andrologia 2021; 53:e13595.
- Bana RS, Sepat SE, Rana KS, et al. Moisture-stress management under limited and assured irrigation regimes in wheat (Triticum aestivum): Effects on crop productivity, water use efficiency, grain quality, nutrient acquisition and soil fertility. Indian J Agricul Sci 2018; 88:1606-2.
- Raffone A, Travaglino A, Flacco ME, et al. Clinical predictive factors of response to treatment in patients undergoing conservative management of atypical endometrial hyperplasia and early endometrial cancer. J Adolescent Young Adult Oncol 2021; 10:193-201.
- Mohammed ZI, Qasim MT. Correlation of AMH and LH Levels in PCOS patients with pregnancy rate. Annals Romanian Society Cell Biol 2021; 945-951.
- Artini PG, Obino ME, Sergiampietri C, et al. PCOS and pregnancy: A review of available therapies to improve the outcome of pregnancy in women with polycystic ovary syndrome. Exp Rev Endocrinol Metabol 2018; 13:87-98.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Sana Tariq1*, Lubna Razzak2, Najia Bhatti3, Basma Zia Isran3, Syeda Sarah Batool4, Sarah Siddiqui5, Syeda Alisha Johar6 and Saadia Siddiqui7
1Public Health Scientist, SZABIST, Karachi, Pakistan2Department of Urogyneacologist, Tabba Kidney Institute, Karachi, Pakistan
3Assistant Professor (Obs/Gyn), Shaheed Mohtarma Benazir Bhutto Medical University, Pakistan
4Department of Urology, Tabba Kidney Institute, Karachi, Pakistan
5Karachi Medical and Dental College, Pakistan
6Medical officer, Dow Medical College, Pakistan
7Department of Medicine Jinnah Sindh Medical University, Pakistan
Received: 03-Feb-2022, Manuscript No. JRMDS-22-53674; , Pre QC No. JRMDS-22-53674 (PQ); Editor assigned: 04-Feb-2022, Pre QC No. JRMDS-22-53674 (PQ); Reviewed: 18-Feb-2022, QC No. JRMDS-22-53674; Revised: 21-Feb-2022, Manuscript No. JRMDS-22-53674 (R); Published: 28-Feb-2022
