Research - (2021) Volume 9, Issue 4
Functional Outcome and Rotational Alignment of Femoral Component in Unnavigated Total Knee Arthroplasty
*Correspondence: Madhukar, Department of Orthopaedics, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, India, Email:
Abstract
Total Knee Arthroplasty helps the patient have a pain free mobile joint, as reflected by the improvement in the post - op Knee Clinical Score and Knee Functional Score. It is possible to achieve the rotational alignment of the components correctly in navigated Total Knee Replacement with appropriate surgical techniques, so that the complications due to misalignment of the components can be avoided. Our study shows that there is significant improvement in the lifestyle of the patients following TKR. Our study shows that there is significant improvement in the lifestyle of the patients following TKR. The aim of this prospective study is to analyze the “functional outcome and rotational alignment of the femoral component in conventional Total Knee Arthroplasty.
Keywords
Total knee arthroplasty, Osteoarthritis, Femoral and tibial, Prosthesis, Intra-medullary, TKR, Patella
Introduction
Arthritis is a joint disease of painful inflammation resulting in stiffness. This is frequently associated with arthralgia. Arthritis may result as a result of abnormal metabolism (such as in Gout and Pseudogout), infection (such as in Lyme disease). Arthritis is the most common disabling disease that affects millions of people in our country. The common causes of knee arthritis include Osteoarthritis (OA), Rheumatoid Arthritis (RA), Juvenile Rheumatoid Arthritis, Post traumatic Arthritis, Secondary Osteoarthritis, and other types of inflammatory arthritis. The incidence of osteoarthritis is increasing with increase in ageing population.
Osteoarthritis is a chronic and painful disease without a known medical cure. Osteoarthritis causes pain and loss of movement in the knee that lead to difficulty in performing daily activities. Medicines can relieve the pain, but they cannot cure the underlying pathology. In most arthritic knees, some degree of instability, deformity, contracture, or a combination of these elements, can be found [1-3]. The concept of improving the knee function by modifying the articular surface has received the attention since the 19th century. Though there are many advances in biomedical technology in last 20 years, persons with destructed joints by osteoarthritis find renewed hope in Total Knee Arthroplasty.
The goals of Total Knee Arthroplasty include:
✓ Pain relief.
✓ Restoration of normal limb alignment.
✓ Restoration of the functional range of movement.
A successful outcome needs precise surgical technique, sound implant design and kinematics with appropriate materials and compliance of patient in rehabilitation. The use of accurate instrumentation and an understanding of the basic principles inherent to the instruments are necessary to implant reproducibly well-aligned prostheses. Computer-assisted navigation is being used by some surgeons to try to improve the reproducibility of component alignment [4]. While performing the Total Knee Arthroplasty, the rotational alignment of femoral and tibial components play a crucial role in determining the functional outcome and polyethylene wear [5]. Range of motion and stability are the two key factors in the success of total knee arthroplasty. Both features relate intimately to the kinematics of the knee joint [6,7].
Primary misalignment and inappropriate positioning of the femoral component, in particular may lead to [8]:
✓ Patellarmal tracking.
✓ Anterior knee pain.
✓ Knee flexion instability.
The rotational alignment of the femoral component can be measured post- operatively by
✓ Conventional radiographs.
✓ Axial two-dimensional (2D) CT scan.
✓ Axial three-dimensional (3D) reconstructed CT scan.
It is measured post-operatively by the angle between transepicondylar axis of femur and posterior condylar line of the prosthesis (Figure 1) [9].
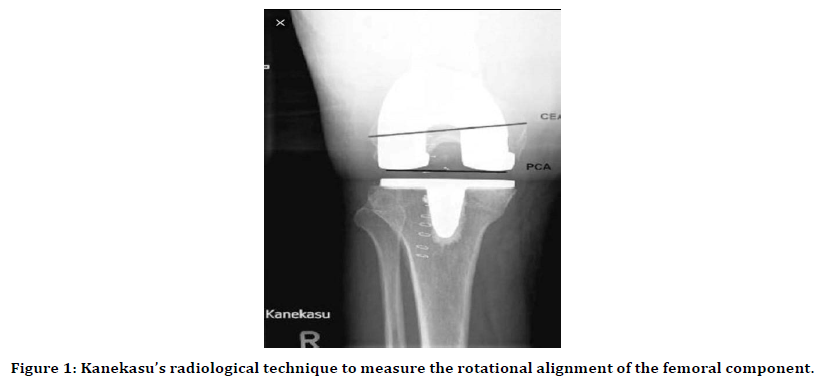
Figure 1. Kanekasu’s radiological technique to measure the rotational alignment of the femoral component.
Materials and Methods
This prospective study was carried out at Sree Balaji Medical College and Hospital, Chrompet from March 2017 to October 2018.The recruitment of patient was for 12 months till January 2018; so that there would be a minimum follow-up period of 9 months (range:9 to 20 months).
Inclusion criteria
Our patients were selected based upon following criteria.
✓ Both male and female in the age group of 51 to 70 years were included.
✓ Patients with Grade III and IV osteoarthritis.
✓ Rheumatoid Arthritis.
✓ Post-Traumatic Arthritis.
Exclusion criteria
✓ Patients with Grade I and II osteoarthritis.
✓ Post-septic arthritis sequelae.
✓ Any co-morbidity that prevents the patient from early mobilization.
Pre-operative evaluation
All our patients were evaluated with detailed history and clinical examination. The preoperative medical evaluation was done for all to prevent complications. Perioperative guidelines have not been well- established for the use of DMARDs in rheumatoid arthritis. The current British Society for Rheumatology guidelines suggest that TNF-α inhibitor therapy should be withheld for 2 to 4 weeks prior to any major surgical procedure. Prospective randomized controlled trial suggested that there was no increased risk of infection or other postoperative complications in patients with rheumatoid arthritis who continued MTX.
In the clinical examination, we looked for varus, valgus and fixed flexion deformities. The extensor mechanism was assessed for any quadriceps contracture. We also assessed for any ligmentous instability and laxity. Any limb length discrepancies were noted. The knee function was assessed pre - operatively by using knee society score.
Routine pre-operative laboratory evaluations including complete blood cell count, electrolytes, urine analysis, blood grouping, ECG, chest roentgenogram and coagulation studies were done. We obtained opinions from otorhinolaryngology, dermatology, dental surgery, and carried out appropriate investigations to rule out the septic foci elsewhere in the body.
Radiological evaluation
Standard guidelines were utilized to get knee radiographs weight bearing antero-posterior view, lateral view. The patellar tracking was assessed with tangential patellar view. The mechanical axis and the alignments of both lower limbs were studied by taking the X-rays including the hip, knee and ankle. Angle between mechanical axis of femur and tibia determines the valgus or varus deformity. Any collateral ligament laxity, subluxation of tibia, presence of osteophytes, any bone defects and the quality of bone is assessed. Sizing of the femoral and tibial components was done.
The goal of preoperative radiological evaluation is to
✓ Confirm the diagnosis for surgical intervention.
✓ To determine the anatomical relationship of the femur and tibia, and
✓ To restore the joint anatomy and biomechanics during the surgery.
Surgical procedure position
The patient is placed in supine position on the operating table. Two stoppers were kept on the operating table with one in 300 of knee flexion and another one at full available flexion. With strict aseptic precautions, painting and draping of the lower limb was done. Pre operative antibiotics were given just before the skin incision. All cases were done under tourniquet control.
Approach
We used anterior midline approach for the skin. 10 cm incision was made centering the patella and extending up to the tibial tuberosity. Medial parapatellar arthrotomy was done to expose the knee joint. The advantage of using the medial para-patellar approach was to prevent the fibrosis on the lateral retinaculum, which may predispose to the dislocation of the patella. Post operative arthrofibrosis can be prevented by excising the retro-patellar fat pad.
The knee is extended and the patella is everted along with their lease of the lateral patella femoralplica. The anterior cruciate ligament Is divided along with the anterior horn of the lateral meniscus to facilitate the eversion of the patella. In knees with varus deformity there is sequential release of superficial collateral ligament, deep collateral ligament, pes tendons and semi-membranous muscle from the posteromedial corner of tibia (Figure 2).
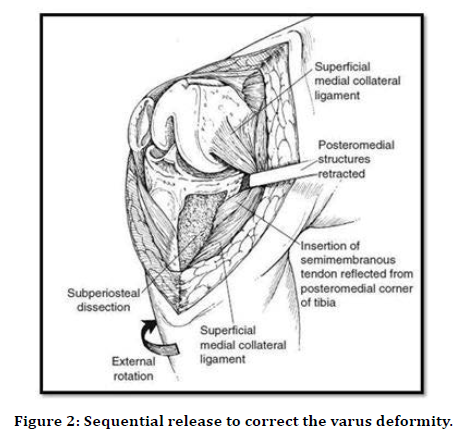
Figure 2. Sequential release to correct the varus deformity.
In knees with valgus deformity, lateral release begins with transverse cutting of the postero-lateral structures (arcuate ligament, posterolateral capsule and reinforcing ligaments) just below the popliteus tendon from the posterolateral corner of the cut surface of the tibia. In severe cases piecrust” release of the iliotibial tract and LCL is performed with a 15 blade by making multiple horizontal incisions in the iliotibial tract (Figure 3).
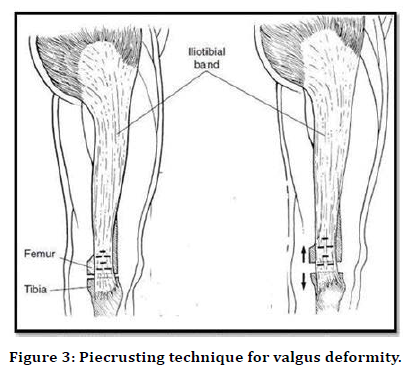
Figure 3. Piecrusting technique for valgus deformity.
The knee is again flexed, the marginal osteophytes removed completely along with the removal of anterior horns of both medial and lateral meniscus. The tibia can now be subluxated anteriorly and externally rotated. The patellar fat pad is partially excised and the everted extensor mechanism is retracted with a levering-type of retractor to expose the lateral tibial plateau.
Femoral preparation
Femoral preparation is done using intramedullary alignment jig. The Whiteside line and Trans-epicondylar line was made over the femoral condyles after exposing the condyles. The vertical line cutting through the middle of distal femoral sulcusis the white sideline. The horizontal line linking the medial and lateral epicondyleis the Trans epicondylarline. At the intersection between these two lines, the starter hole is created. With the help of 9.5mm diameter drill bit, medullary canal was opened.
Component implantation
The trial prosthesis for tibia and femur is fixed with the articular insert, the ligamentous balancing and patellar tracking is assessed. The trial components are removed and bony ends are cleaned with saline. The femoral component is cemented in a similar fashion with a few additional considerations. Usually, all components are cemented simultaneously with one batch (40 g) of cement. The press fit articular insert is then fixed to the tibial tray.
Post-operative protocol
In the immediate post-operative period compression bandage was applied. Intravenous antibiotics were given for 48 to 72 hours. Epidural analgesia is continued for 48 hours post operatively. Subcutaneous low molecular weight heparin was given as DVT prophylaxis. On day of surgery, patient was started on CPM in the recovery room for at least 4 hours. A towel roll is placed under the ankle once the CPM is stopped.
Observation And Results
Age and sex distribution
Our patients were in the age group of51 to 70 years with an average of 61.6years. Most of our patients were between 61 to 65 years (Table 1).
| Age in years | Male | Female | Patients’ “n” |
|---|---|---|---|
| 51-55 | 1 | 2 | 3 |
| 56-60 | 2 | 3 | 5 |
| 61-65 | 3 | 5 | 8 |
| 66-70 | 2 | 2 | 4 |
| TOTAL | 8 | 12 | 20 |
Table 1: Age and sex distribution.
Side distribution
In our series left side was more commonly operated upon. Left to Right ratio was 3:2 (Table 2 and Figure 4).
| Side | Frequency |
|---|---|
| Right | 8(40%) |
| Left | 12(60%) |
| Total | 20(100%) |
Table 2: Side distribution.
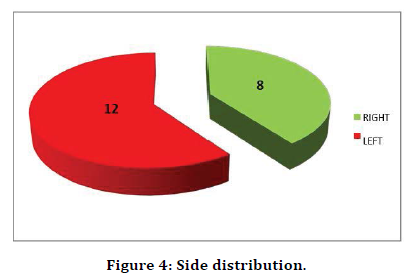
Figure 4. Side distribution.
Deformity
In our study 80% of cases had varus deformity, 20% had valgus deformity and 20% had fixed flexion deformity (Table 3 and Figure 5).
| Deformity of knee | Frequency ‘n’(%age) |
|---|---|
| Varus knee | 16 (80%) |
| valgus knee | 4 (20%) |
| Fixed flexion deformity | 4 (20%) |
Table 3: Deformity.
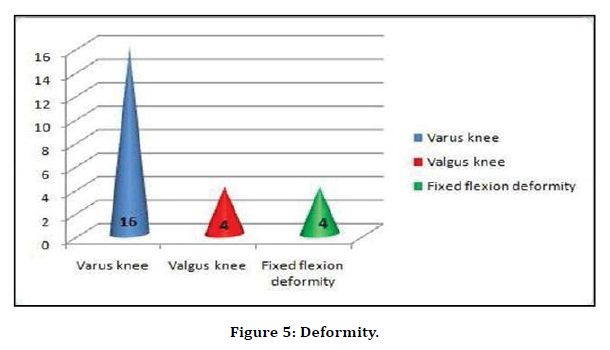
Figure 5. Deformity.
Indications
Osteoarthritis was the most common indication in our series, followed by Rheumatoid arthritis and post- traumatic arthritis (Table 4 and Figure 6).
| Indication for TKR | No of patient’s “n” | %age |
|---|---|---|
| Osteoarthritis | 15 | 75 |
| Rheumatoid arthritis | 4 | 20 |
| post traumatic arthritis | 1 | 5 |
Table 4: Indications.
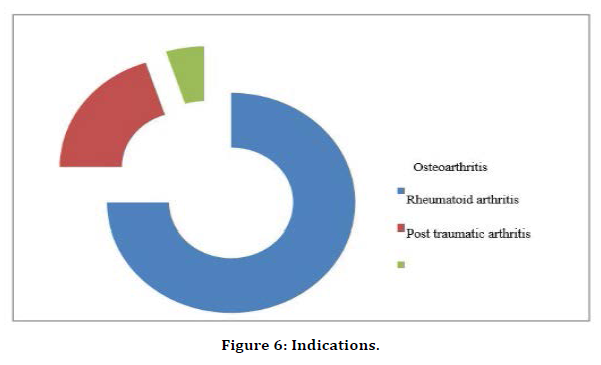
Figure 6. Indications.
Types of prosthesis
Cruciate retaining prosthesis were more commonly used than cruciate substituting prosthesis (Table 5 and Figure 7).
| Type of TKR prosthesis used | No of patient’s “n” | %age |
|---|---|---|
| Cruciate retaining | 16 | 80 |
| Cruciate substituting | 4 | 20 |
Table 5: Types of prosthesis.
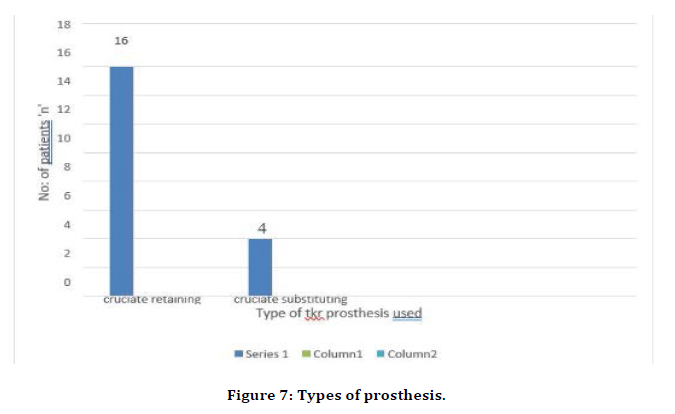
Figure 7. Types of prosthesis.
Rotational alignment of the femoral component (Table 6 and Figure 8).
| Rotational alignment of the femoral component in external rotation | Frequency “n” | % age |
|---|---|---|
| 4-7 degrees | 12 | 60 |
| 7.1-10 degrees | 6 | 30 |
| 10.1-13degrees | 2 | 10 |
Table 6: Rotational alignment of the femoral component.
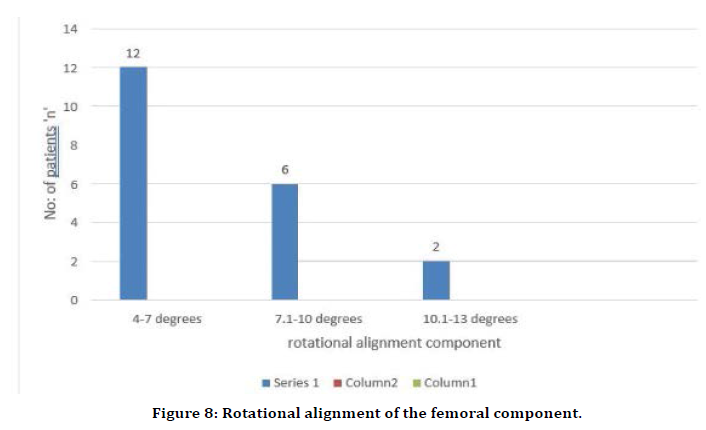
Figure 8. Rotational alignment of the femoral component.
Complications
In our study knee pain was encountered in 30 % of cases (n=6), superficial infection in 10 % of cases (n=2) and notching of anterior femoral cortex in 5 % ofcases (n=1) (Table 7 and Figure 9).
| Complications | Frequency “n” | % age |
|---|---|---|
| Anterior knee pain | 6 | 30 |
| Superficial infection | 2 | 10 |
| Notching of anterior femoral cortex | 1 | 5 |
Table 7: Complications.
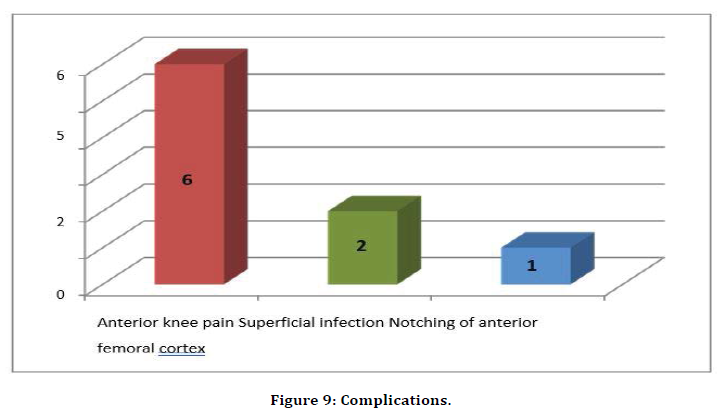
Figure 9. Complications.
Knee clinical score
The average pre-operative Knee Clinical Score was 27.15 in our study, which improved to an average post-op score of 91.6 (Table 8 and Figure 10).
| Status | ‘n’ | Mean | Median | Mode | Standard deviation | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| Pre-op | 20 | 27.15 | 28 | 28 | 7.45 | 14 | 38 |
| Post-op | 20 | 91.6 | 92 | 98 | 7.34 | 75 | 99 |
Table 8: Knee clinical score.
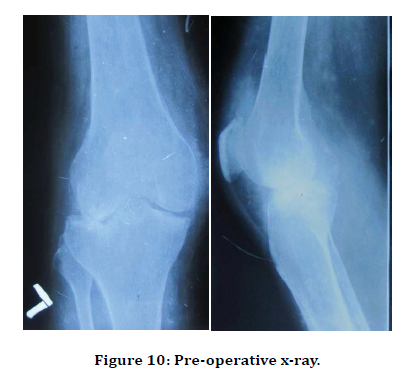
Figure 10. Pre-operative x-ray.
Grading of knee clinical score
According to the Knee Society Clinical scoring system out of 20 patients, 75% patients (n=15) had excellent results,20%patients (n=4) had good results and 5%patient (n=1) had fair results (Table 9).
| Frequency | Percent | |
|---|---|---|
| Excellent | 15 | 75 |
| Good | 4 | 20 |
| Fair | 1 | 5 |
| Total | 20 | 100 |
Table 9: Grading of knee clinical score.
Case Illustrations
Case illustrations I to III are described as follows.
Case illustration-I (Figure 10-13).
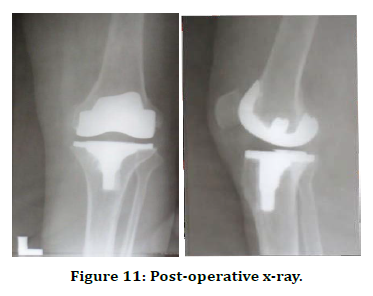
Figure 11. Post-operative x-ray.
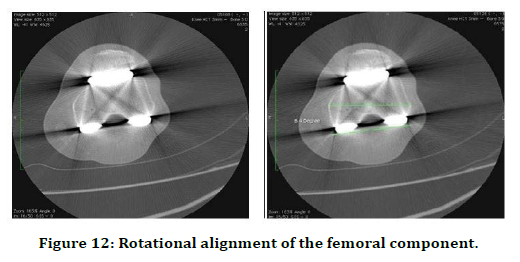
Figure 12. Rotational alignment of the femoral component.
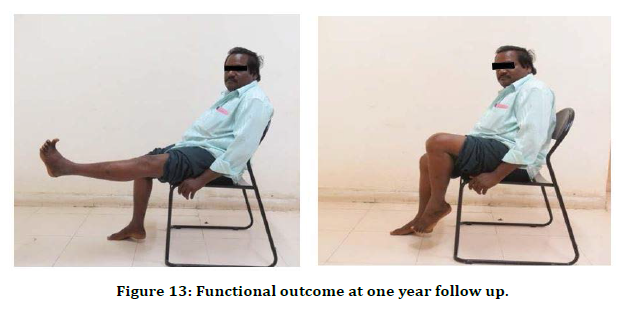
Figure 13. Functional outcome at one year follow up.
Case illustration-III (Figures 18-21)

Figure 14. Pre-operative x-ray.

Figure 15. Post-operative x-ray.
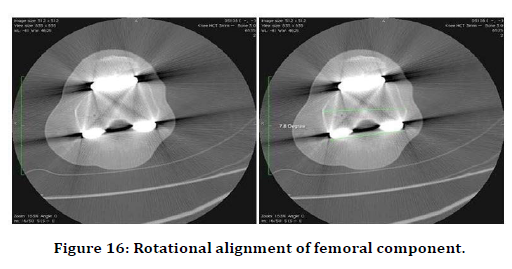
Figure 16. Rotational alignment of femoral component.
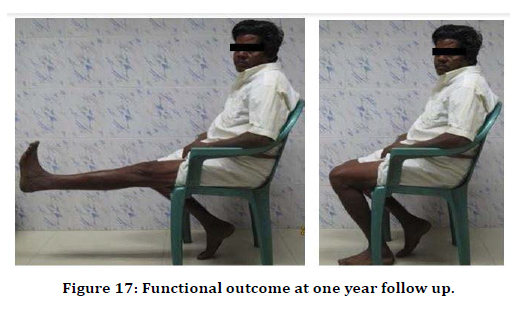
Figure 17. Functional outcome at one year follow up.
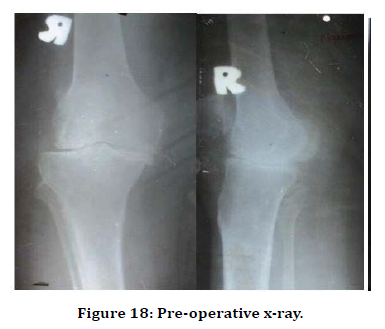
Figure 18. Pre-operative x-ray.
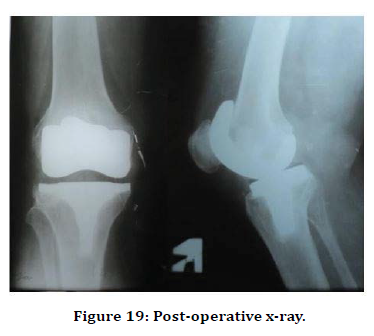
Figure 19. Post-operative x-ray.
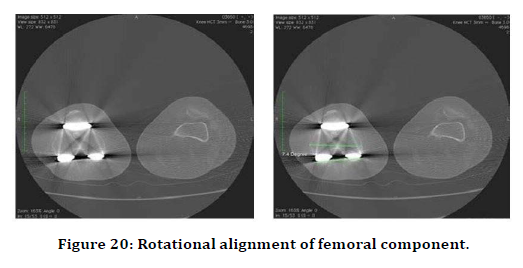
Figure 20. Rotational alignment of femoral component.
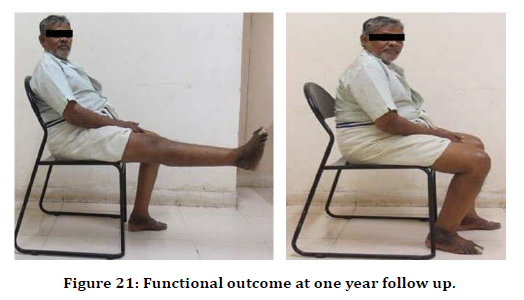
Figure 21. Functional outcome at one year follow up.
Discussion
Total Knee Arthroplasty done for patients suffering with arthritic knee provides the patient with considerable medium to long term benefits in terms of the quality of life (QOL), pain relief and function. The common causes of arthritis of the knee include osteoarthritis (OA), rheumatoid arthritis (RA), juvenile rheumatoid arthritis (JRA), post traumatic arthritis or secondary osteoarthritis and other types of inflammatory arthritis. Osteoarthritis (OA) is a chronic degenerative joint disease and a major cause of disability in the elderly people.
Significant advances have occurred in the type and quality of the metals, polyethylene, and more recently in the ceramics used in the prosthesis manufacturing process, leading to improved prosthesis longevity. As with most techniques in modern medicine, more and more patients are receiving the benefits of total knee arthroplasty (TKA) [10-25]. These advances in the knee implant design and the surgical techniques for total knee replacement achieved successful results in reducing the pain and providing with a stable joint.
Certainly, total knee replacement (TKR) is recommended for people with osteoarthritis for whom less invasive treatments (such as physiotherapy, analgesics, anti- inflammatory drugs, intra-articular steroids, hyaluronic acids, and arthroscopic surgery) have failed.
The selection of prosthesis for each patient depends on the anatomical status of the knee joint. The functional outcome following Total knee Arthroplasty depends upon various parameters including the surgical technique, soft tissue balancing, near anatomical rotational alignment of the femoral and tibial components, and cementation of the prosthesis. Incorrect femoral rotations can result in a trapezoidal flexion gap, which can lead to patello-femoral tracking problems [23] instability, dysfunctional overall biomechanics [26-28] and anterior knee pain [23]. To achieve correct femoral rotation, two methods have been devised [22]. The first relies on the tibial cut being performed prior to the femoral cut. This method, termed the “classic method,” relies on a tensedknee in flexion postligament balancing in extension, followed by an anteroposterior (AP) cut of the femur parallel to the cut surface of the tibia [25,27]. This method is especially useful for more severely malaligned knees as it adjusts for changes in laxity that occur post-ligament balancing and compensates for unexpected bone loss [27]. In a number of studies, it has been shown to be a highly accurate method of determining rotation and producing a rectangular flexionextension gap [22,23].
The second method relies on osseous landmarks. This method has become popular as the majority of implant manufacturers base their AP cuts on these landmarks [27]. Three separate bony landmarks have been identified to aid with defining rotation. These include: The posterior condylar axis, using a neutral or three degrees of external rotation cut [23] Whiteside's line or the transverse axis of the femoral component, with the cut being made perpendicular to the line passing through the trochlear groove from the lateral edge of the PCL [21,25]. On comparing the similar studies that have been done to our study there were not much of a difference, but the purpose of the studies was different. In a study which was done to assess the Rotational Alignment of Femoral Component and Flexion Gap Balance in 46 Patients With Distal Femoral Torsional Deformity Using Navigation-assisted TKA, Preoperative distal femoral torsional angle and postoperative rotational deviation of the femoral component were measured using computed tomography.The mean distal femoral torsional angle was 8.3° (range, 7°-12°). The mean rotational deviation of the femoral component was 4.1° (range, 2°-6°) and 4.2° (range, 2°-6°) external rotation about the PCA. In our study the mean rotational deviation of the femoral component was 5.5 ° (range 4-13°).
This study showed that navigation-assisted gap technique provided balanced flexion gaps in most patients with distal femoral torsional deformity. The femoral component was not aligned with bony landmarks such astransepicondylar axis or Whiteside’s line in patients with distal femoral torsional angle >7°. The femoral component was a mean of 4.5° (range, 2° -6°) internally rotated with reference to TEA when balanced flexion gaps were achieved in this study. The determination of femoral component rotation using anatomic bony landmarks method alone can result in excessive external rotation of the femoral component and unbalanced flexion gaps in patients with distal femoral torsional deformity. The soft tissue balancing using a navigation-guided gap technique can be a reliable method for achieving symmetrical flexion gaps, especially in patients with distal femoral torsional deformity [29-31].
Based on another study which was done by Claudio Carlo Castelli, Daniele Antonio Falvo, Mario Luigi Iapicca, Valerio Gotti Department of Orthopaedics, Bergamo, Italy. They described various surgical options to obtain a correct rotational alignment of femoral component in total knee arthroplasty (TKA). The correct rotational alignment is the key point to obtain a rectangular balanced flexion gap as well to have a good patellar tracking. For that reason, rotation alignment largely affects postoperative kinematic results particularly during flexion [32]. It is therefore essential to know different techniques, the instruments and the use at least two references: a reliable bone landmark and soft tissue envelop balancing [33].
The purpose of our study was to compare the rotational alignment of the femoral component and the functional outcome. Lesser the external rotation of the femoral component, better the outcome of the surgery. Patients in whom the external rotation of the femoral component was less than 5 degree had excellent knee clinical score and the function score, so the outcome was better.
Conclusion
Rotational alignment is especially important in getting good flexion and extension gap and preventing problems of rotational malalignment. Good rotational alignment is associated with good clinical and functional outcome. The functional outcome of Total knee Arthroplasty can be assessed by using the Knee Society Score System. The Knee Society Scoring system is subdivided in to a knee score that rates only the knee joint itself and a functional score that rates the patient’s ability to walk and climb stairs. This dual rating system eliminates the problem of declining knee scores associated with patient infirmity. Rotational alignment of femoral component and the functional outcome has been assessed in this study.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Vali TP, Lang JE. Insall and Scott surgery of the knee.4thed. Philadelphia: Churchill Livingstone, Elsevier;2006. p. 1455 -1521.
- Insall J, Ranawat CS, Scott WN, Walker P. Total condylar knee replacement. Preliminary report. Clin Orthop Relat Res 1976;120:149 - 54.
- Kim RH, Scott WN. Operative techniques: total knee replacement. Philadelphia: Saunders-Elsevier; 2009. p. 91-103.
- Y.H. Kim, J.S. Kim, S.H. Yoon, from EwhaWomans University School of Medicine, Soeul, Korea, Alignment and Orientation of the Components in Total Knee Replacement with and without Navigation Support. J Bone Joint Surg [Br]Vol. 89 -B, No.4, April2007.
- Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin OrthopRelat Res2002;(404):7-13.
- Cloutier JM, Sabouret P, Deghrar A. Total knee arthroplasty with retention of both cruciate l igaments: a nine to eleven-year follow-up study. J Bone Joint Surg Am.1999;81:697–702.
- LaPrade RF, Ly TV, Wentorf FA et al: The posterolateral attachments of the knee: a qualitative and quantitative morphologic analysis of the bularcol later alligament, popliteus tendon and lateral gastrocnemius tendon. Am. J. Sports Med. 2003; 854 860.
- Banks SA, Fregly BJ, Boniforti F, Reinschmidt C, Romagnoli S. Comparing in vivo kinematics of unicondylar and bi-unicondylar knee replacements. Knee Surg Sports TraumatolArthrosc. 2005;13: 551– 556.
- Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining The rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin OrthopRelat Res1993;286:40 -7.
- JohnNInsall, Lawrence D Dorr, RichardDScott, W.NormanScott. Rationale of The Knee Society Clinical Rating System. Clin Orthop 1989 Nov 14 -18.
- Kim RH, Scott WN. Operative techniques: total knee replacement. Philadelphia:Saunders-Elsevier; 2009. p. 91-103.
- Campbell WC. Interposition of vitallium plates in arthroplasty of the knee: preliminary report. Am J Surg1940;47:639.
- Walldius B. Arthroplasty of the knee joint using endoprosthesis. Acta OrthopScand1957;24:19.
- MacIntosh DL. Arthroplasty of the knee. J Bone Joint Surg 1966;48:179.
- Insall JN, Ranawat CS, Scott WN, Walker PS. Total condylar knee replacement: preliminary report. Clin Orthop1976;120:149 -54.
- Insall JN, Lachiewicz PF, Burstein AH. The posterior stabilized condylar prosthesis: a modification of total condylar design: two to four year clinical experience. J Bone Joint Surg1982;64:1317.
- Laskin RS, Maruyama Y, Villaneuva M. Deep-dish congruent tibial Component. Use in total knee arthroplasty: a randomized prospective study. Clin OrthopRelat Res2000;380:36.
- Marmor L. Unicompartmental arthroplasty of the knee with a minimum ten- Year follow-up period. Clin OrthopRelat Res 1988;228:171.
- Donaldson III WF, Sculco TP, Insall JN. Total condylar III knee prosthesis: Long term follow-up study. Clin OrthopRelat Res 1988;226:21.
- Goodfellow JW, O'Connor JJ, Murray DW. Principles of meniscal bearing arthroplasty for unicompartmental knee replacement. Paris: Expansion Scientifique Francaise;1 997.
- Buechel FF. New jersey low-contact-stress knee replacement system. Clin OrthopRelat Res 1991;264:211.
- Jordan LR, Olivo JL, Voorhorst PE. Survivorship analysis of cementless Meniscal bearing total knee arthroplasty. Clin OrthopRelat Res1997;338:119.
- Callaghan JJ, Squire MW, Goetz DD. Cemented rotating-platform total knee replacement: a nine to twelve-year follow-up study. J Bone Joint Surg2000;82:705.
- Marmor L. Unicompartmental arthroplasty of the knee with a minimum ten-Year follow-up period. Clin OrthopRelat Res 1988;228:171.
- Rand JA, Chao EY, Stauffer RN. Kinematic rotating- hinge total knee arthroplasty. J Bone Joint Surg1987;69:489.
- Andriacchi TP, Galante JO, Fermier RW. The influence of total knee Replacement design on walking and stair climbing. J Bone Joint Surg 1982;64:1328.
- Dennis DA, Clayton ML, O'Donnell S. Posterior cruciate condylar total Knee arthroplasty: average 11 -year follow-up examination. Clin OrthopRelat Res1992;281:168.
- Figgie HE, Goldberg VM, Figgie MP. The effect of alignment of the implant on fractures of the patella after condylar total knee arthroplasty. J Bone Joint Surg1989;71:1031.
- Hozack WJ, Rothman RH, Booth Jr RE. The patellar clunk syndrome: a complication of posterior stabilized total knee arthroplasty. Clin OrthopRelat Res1989;241:203.
- Maloney WJ, Schurman DJ. The effects of implant design on range of motion after total knee arthroplasty: total condylar versus posterior stabilized total condylar designs. Clin OrthopRelat Res1992;278:147.
- Laskin RS. The Genesis total knee prosthesis: a 10 -year follow up study. Clin OrthopRelat Res2001;388:95.
- Faris PM, Herbst SA, Ritter MA. The effect of preoperative knee deformity on the initial results of cruciate-retaining total knee arthroplasty. J Arthroplasty1992;7:527.
- Dennis DA, Komistek RD, Colwell Jr CE. In vivo anteroposterior Femorotibial translation of total kne e arthroplasty: a multicenter analysis. Clin OrthopRelat Res1998;356:47.
Author Info
Department of Orthopaedics, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Vignesh D, Madhukar, Functional Outcome and Rotational Alignment of Femoral Component in Unnavigated Total Knee Arthroplasty, J Res Med Dent Sci, 2021, 9 (4):476-487.
Received: 22-Mar-2021 Accepted: 23-Apr-2021
