Case Report - (2019) Volume 7, Issue 3
Gastric Perforation in a Neonate with Trachea-esophageal Fistula
Lawan Musa Tahir1*, Lokman Cam1, Goksel Bahadir2, Pascal Anyawu3, Ummi Sani Dambatta4 and Senol Dane5
*Correspondence: Lawan Musa Tahir, Department of Pediatrics, Nizamiye Hospital, Nigeria, Email:
Abstract
The purpose of this study was to present a case with the gastric perforation and pneumoperitoneum due to the mechanic ventilation in a female neonate with congenital esophageal atresia and distal trachea-esophageal. The subject of the present study was one female late preterm neonate with very low birth weight (1.48 Kg). She needed mechanical ventilation because her low oxygen saturation. Gastric perforation and pneumoperitoneum occurred secondary to mechanic ventilation. She had an abdominal paracentesis and an emergency laparotomy. The gastric perforation was repaired, banding of the fistula was applied and gastrotomy tube was inserted. She was stabilized post-operatively but unfortunately died a week after from sepsis and heart failure.
Keywords
Trachea-esophageal fistula, Mechanical ventilation, Gastric perforation, Pneumoperitoneum
Introduction
Trachea-esophageal fistulae are often associated with life threatening complications. They are usually diagnosed in the neonatal period. Esophageal atresia with distal trachea-esophageal fistula accounts for more than 80% of all trachea-esophageal fistulae [1]. An infant with this type of trachea-esophageal fistulae is intubated and commenced on ventilator assistance; the air with increased pressure in the airways is transmitted through the fistula to the gastrointestinal tract. The continuous positive pressure breathing in a child with tracheaesophageal fistulae may result in gastric perforation with resultant pneumoperitoneum as a complication and is associated with high mortality [2,3].
Spontaneous gastric perforation, although rare, has been reported in newborn babies and the commonly associated prenatal and perinatal risk factors as reported in order of frequency are prematurity, respiratory distress syndrome, birth asphyxia and resuscitation, premature rupture of membranes, breech delivery, caesarian delivery and twin delivery [4].
The purpose of this study was to cause awareness about complications of the mechanic ventilation with positive pressure such as gastric perforation and pneumoperitoneum in a female neonate with congenital esophageal atresia and distal trachea-esophageal.
Case Study
This case deals with a female, late preterm neonate with very low birth weight (1.48 Kg). She was delivered at gestational age of 36 weeks by emergency caesarean section because her mother had uterine rupture. The mother was primiparous and had no antenatal clinic visit. When the baby was born, she was flaccid and her APGAR scores were 2 and 5 at 1st and 5th minutes, respectively. She was actively resuscitated; airway suctioning, intubation and bag and mask ventilation as well as cardiac massage were done in the theater (Figure 1). Baby was transferred to neonatal intensive care unit where she was commenced on mechanical ventilation.
Figure 1. Assisted ventilation
She had multiple congenital abnormalities; small face with cleft lip & palate, VSD & ASD, esophageal atresia (EA) with distal trachea-esophageal fistula and bilateral talipes deformity. She was treated with surfactant and commenced on antibiotics and 5% Dextrose infusions immediately.
It has been noticed that she has a sudden onset of abdominal distention with deteriorating respiratory function on the second day of life. Oxygen saturation dropped to 84% at SPO2 of 90% and she had respiratory acidosis (pH=7.271, PCO2=48.8). Pneumoperitoneum was suspected and radiological confirmed (Figures 2 and 3).
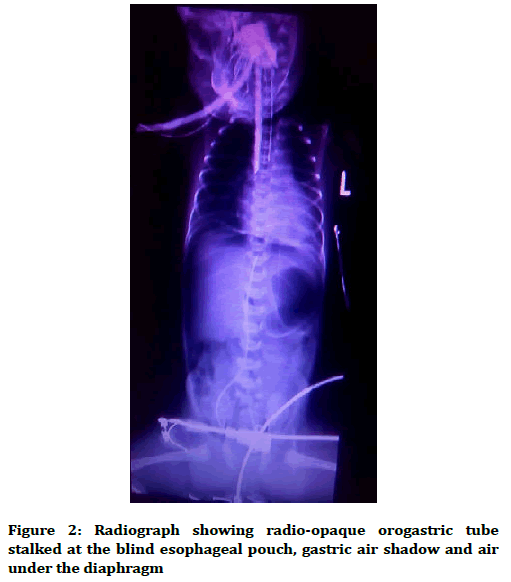
Figure 2. Radiograph showing radio-opaque orogastric tube stalked at the blind esophageal pouch, gastric air shadow and air under the diaphragm
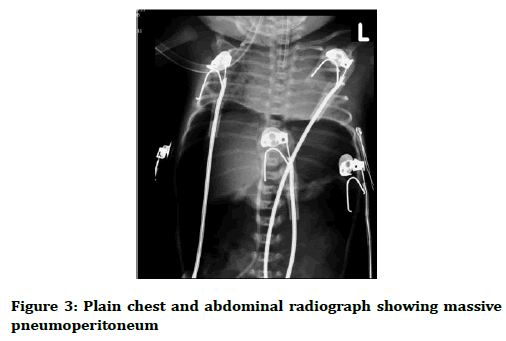
Figure 3. Plain chest and abdominal radiograph showing massive pneumoperitoneum
A needle paracentesis was done while planning for an urgent laparotomy. At the laparotomy, the gastric perforation was repaired, banding of the fistula was applied and gastrotomy tube was inserted (Figures 4 and 5). She was treated with total parenteral nutrition and the feeding through gastrotomy tube was commenced by second day post-op. She became stable and by 5th day post-op attempt was being made to wean off mechanical ventilator. On the 7th day post-op both respiratory and cardiac functions began to deteriorate. She unfortunately died of sepsis and heart failure at 12 days old.
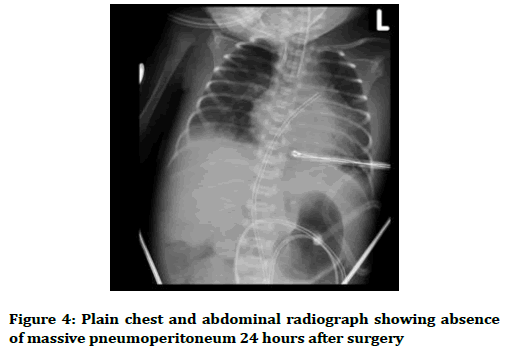
Figure 4. Plain chest and abdominal radiograph showing absence of massive pneumoperitoneum 24 hours after surgery
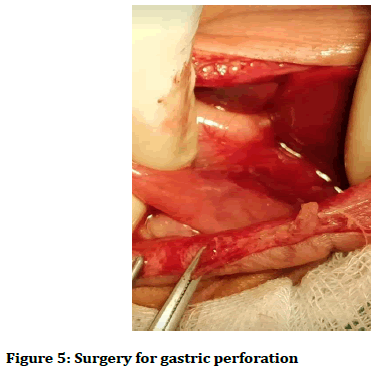
Figure 5. Surgery for gastric perforation
Discussion
Gastric perforation is a well-known complication of esophageal atresia with distal tracheo-oesophageal fistula, and is usually associated with extreme prematurity, hyaline membrane disease in which all the neonate requires for assisted ventilation [5-7]. The presentation is sudden, and leads to further deterioration in respiratory function because of increasing abdominal distension from pneumoperitoneum and splinting of the diaphragm. Unrelieved, the infant becomes increasingly hypoxic and may die [1,7,8].
Our patient was a late preterm (36 weeks gestational age) with very low birth weight (birth weight of 1.48 Kg). She had esophageal atresia with distal tracheaesophageal fistula as well as additional multiple congenital abnormalities (small face with cleft lip & palate, VSD & ASD and bilateral talipes deformity). She also had perinatal asphyxia and required intubation and respiratory support, thus was at a high risk of gastric perforation. Her clinical state was noticed to have suddenly deteriorated and remarkably improved following abdominal paracentesis, typical of presentation of massive pneumoperitoneum. Other co-morbidities contributed significantly to the poor outcome in our patient.
Conclusion
To conclude, in the present case, other co-morbidities contributed significantly to the poor outcome in our patient. The gastric perforation was repaired, banding of the fistula was applied and gastrotomy tube was inserted. She was stabilized post-operatively but unfortunately died a week after from sepsis and heart failure. Gastric perforation and pneumoperitoneum due to mechanical ventilator with positive pressure should be taken into account in a neonate with trachea-esophageal fistula at all times.
References
- Kumar PD, Rainey J, Kotton B. Tracheoesophageal fistula and massive pneumoperitoneum after prolonged mechanical ventilation. South Med J 2001; 94:1027-9.
- Parker JJ, Mikity VG, Jacobson G. Traumatic pneumoperitoneum in the newborn. AJR 1965; 95:203-7.
- Kaufman RA, Kuhns UR, Poznanski AK, et al. Gastrointestinal perforations without intraperitoneal air-fluid level in neonatal pneumoperitoneum. AJR 1976; 127:915-21.
- Behera MK, Harikrishnan KM, Sunil J. Spontaneous gastric perforation in newborn, case report. Med J Armed Forces India 1991; 54:353-4.
- Leonidas J, Berdon WE, Baker DH, et al. Perforations of the gastrointestinal tract and pneumoperitoneum in newborns treated with continues lung distending pressures. PediatrRadiol 1974; 2:241-6.
- Kirkpatrick BV, Felman AH, Eitzman DV. Complications of ventilator therapy in respiratory distress syndrome. Am J Dis Child 1974; 128:496-502.
- Maoate K, Myers NA, Beasley SW. Gastric perforation in infants with oesophageal atresia and distal trachea-oesophageal fistula. PediatrSurg Int 1999; 15:24-7.
- Byun J, Kim HY, Noh SY, et al. Neonatal gastric perforation: A single center experience. World J Gastrointest Surg 2014; 6:151-5.
Author Info
Lawan Musa Tahir1*, Lokman Cam1, Goksel Bahadir2, Pascal Anyawu3, Ummi Sani Dambatta4 and Senol Dane5
1Department of Pediatrics, Nizamiye Hospital, Abuja, Nigeria2Department of Anaesthesia, Nizamiye Hospital, Abuja, Nigeria
3Department of Surgery, National Hospital, Abuja, Nigeria
4College of Health Sciences, Nile University of Nigeria, Abuja, Nigeria
5Department of Physiology, College of Health Sciences, Nile University of Nigeria, Abuja, Nigeria
Citation: Lawan Musa Tahir, Lokman Cam, Goksel Bahadir, Pascal Anyawu, Ummi Sani Dambatta, Senol Dane, Gastric Perforation in a Neonate with Trachea-esophageal Fistula, J Res Med Dent Sci, 2019, 7(3): 46-48.
Received: 11-Apr-2019 Accepted: 01-May-2019
