Research - (2022) Volume 10, Issue 3
Giant Epididymal Cyst with Absent Tunica Vaginalis
Narendran Govindarajan*, Raghupathy Thirunavukkarasu and Magesh Chandran
*Correspondence: Narendran Govindarajan, Department of General Surgery, Sree Balaji Medical College and Hospital, Bharath university, India, Email:
Abstract
We present a case of 82 yr. old male who came to hospital was planned for eversion of sac for hydrocele. During surgery testis was found to be devoid of tunica vaginalis and a giant cyst was present over the epididymis. The cyst was excised and was sent for histopathological examination and found to be epididymal cyst. This is a rare case presentation as it is not reported anywhere.
Keywords
Epididymal cyst, Surgery, Ultrasound
Introduction
Epididymal cysts are multilocular cystic fluid collections in a single sac. They are usually solitary; however they can often be seen in groups. These cysts are completely harmless [1]. The initial clinical sign may be a scrotal enlargement that grows in size and is described by the patient as a third testicle. The second symptom is testicular discomfort. Accidental physical examination is the third method of epididymal cyst discovery. The fourth presentation is the most prevalent, and it is discovered during a scrotum ultrasound [2]. In the juvenile age group, clinical examination of the scrotal can be difficult to determine a diagnosis, especially if there is discomfort. Ultrasound can make a good anatomical and pathological diagnosis [3].
Epididymal cysts have an unknown prevalence, but they are more common in teenagers. A 14.4% incidence of epididymal cyst was discovered in a systematic assessment of paediatric scrotal ultrasounds. In patients above the age of 15, the prevalence of epididymal cysts increased to 35.5 percent. Regardless of age group, patients with epididymal cysts had bigger testes [4]. The fluid in these epididymal cysts is clear and wonderfully translucent.
Cystic fibrosis, polycystic kidney disease, and Von Hippel-Lindau disease have all been linked to epididymal cysts in children exposed to diethylstilbestrol in utero [5-7]. For epididymal cyst diagnosis, ultrasonography of the scrotum is the most accurate imaging method [8]. Conservative treatment, cyst aspiration, and cyst excision are the options for treating epididymal cysts [9].
Case Report
An 82yr old male came with complaints of swelling in right scrotum for 10 yrs duration. Gradual in onset, progressive in nature, not associated with pain. Patient had no other specific complaints. On examination, the right side of scrotum shows a swelling of 15x10 cm size which is confined to scrotum (can get above the swelling). The surface of swelling is smooth and well defined. No warmth, non-tender. The swelling is fluctuant and transilluminant. The right testis is not separately felt. Skin over swelling normal. Contralateral testis and genitalia normal. A diagnosis of right hydrocele was made. The rest of the examination was unremarkable.
Investigations
Biochemical & hematological investigations were within normal limits. Urine routine was normal.
Treatment
The patient was operated as an elective case done under spinal anesthesia. Right vertical incision was made parallel to median raphe. Through an incision right testis was seen anteriorly and a giant cyst was seen posteriorly. Right cyst was excised in toto. Dartos was closed with 2-0 chromic catgut. Skin closed with 2-0 chromic catgut. Procedure was uneventful. Scrotal bandage applied (Figure 1).
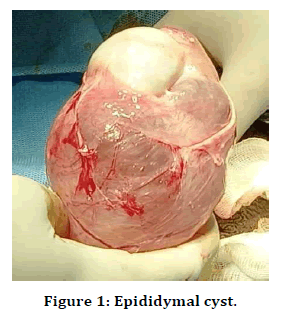
Figure 1. Epididymal cyst.
Outcome
Post op period was uneventful. Patient improved symptomatically and was discharged.
Discussion
Epididymal cysts are prevalent in teens and young adults. Epididymal cysts are uncommon in children under the age of 12. True epididymal cysts are uncommon in individuals over the age of 40 as they are mainly spermatocele. In our case, the patient was 82 years old having a epididymal cyst which occur less commonly in this age group. Secondly in these cases they are linked to epididymo-orchitis. Because of the numerous brilliant translucency and finely boss elated surface give an appearance of “Chinese lantern”.
Epididymal cysts are unilocular or multilocular collections of fluid in the epididymis caused by tubular blockage causing dilatation of efferent epididymal tubules [10]. A research discovered that cyst development is caused by local production of proinflammatory cytokines, as shown by increased levels of interleukin 8 (IL8) and interleukin 6 (IL6) in epididymal cysts [9]. Epididymal cysts are extra testicular lumps that are generally smooth, spherical, and found within the epididymis in clinical practice. Our patient had no symptoms at all, and the sole complaint was discomfort that led to an ultrasound examination confirming the diagnosis [7].
Conclusion
The cyst in the epididymis can be found with an ultrasound examination. The epididymis head is the most typical place but it can also occur in the body and tail very rarely. But in our case it involved all 3 parts of epididymis which is another rare instance. The appearance of an epididymal cyst on ultrasonography is similar to that of cystic tumours such as epididymal adenomatoid tumour and mesodermal tumour of the testis. They should also be taken into account while making a differential diagnosis.
References
- Gerscovich EO. High resolution ultrasonography in the diagnosis of scrotal pathology: Normal scrotum and benign disease. J Clin Ultrasound 1993; 21:355-373.
- Singh AK. Clinico pathological study of cystic swellings of scrotum. Asian J Biomed Pharamceutical Sci 2016; 6:42-44.
- Delaney LR, Karmazyn B. Ultrasound of the pediatric scrotum. Semin Ultrasound CT MR 2013; 34:248-56.
- Posey ZQ, Ahn HJ, Junewick J, et al. Rate and associations of epididymal cysts on pediatric scrotal ultrasound. J Urol 2010; 184:1739-42.
- Arora BK, Arora R, Arora A. A randomised study of management modalities in epididymal cyst. Int Surg J 2019; 6:340‐344.
- Fernández‐Ibieta M, Villalon‐Ferrero F, Ramos‐García JL. Benign scrotal tumor in a pediatric patient: epididymal cyst. Case Rep Urol. 2018;2018:1‐3.
- Posey ZQ, Ahn HJ, Junewick J, et ak. Rate and associations of epididymal cysts on pediatric scrotal ultrasound. J Urol 2010; 184:1739‐1742.
- Kocak I, Dündar M, Yenisey C, et al. Pro‐inflammatory cytokine response of the fluid contents of spermatoceles and epididymal cysts. Andrologia 2002; 34:112‐115.
- Bleve C, Conighi ML, Bucci V, et al. Torsion of huge epididymal cyst in a 16‐year‐old boy: Case report and review of the literature. Pediatr Med Chir 2018; 40.
- Kocak I, Dündar M, Yenisey C, et al. Pro‐inflammatory cytokine response of the fluid contents of spermatoceles and epididymal cysts. Andrologia 2002; 34:112-115.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Narendran Govindarajan*, Raghupathy Thirunavukkarasu and Magesh Chandran
Department of General Surgery, Sree Balaji Medical College and Hospital, Bharath university, Chrompet, Chennai, IndiaReceived: 28-Feb-2022, Manuscript No. JRMDS-22-52878; , Pre QC No. JRMDS-22-52878 (PQ); Editor assigned: 02-Mar-2022, Pre QC No. JRMDS-22-52878 (PQ); Reviewed: 16-Mar-2022, QC No. JRMDS-22-52878; Revised: 23-Mar-2022, Manuscript No. JRMDS-22-52878 (R); Published: 30-Mar-2022
