Research - (2021) Volume 9, Issue 3
Guillain-BarrE Syndrome Following COVID-19: A Case Report
Aqeel Almutairi*, Sarah Bin Abdulqader, Majed Alhameed, Sajjad Ali, Bandar Alosaimi and Rakan Alotaibi
*Correspondence: Aqeel Almutairi, National Neuroscience Institute, King Fahad Medical City, Riyadh, Saudi Arabia, Email:
Abstract
Introduction: Guillain-Barre syndrome (GBS) is an immune mediated disease that often manifests clinically after an infectious process. Patients with GBS classically present with progressive, ascending symmetrical flaccid paralysis with diminished or lost deep tendon reflexes. Case report: we report a case of 36-year-old healthy male who developed bilateral progressive distal extremity numbness, change in speech and bilateral facial weakness within 3 weeks of SARS-CoV-2 infection. The patient was diagnosed with GBS and treated with Intravenous immune globulin with significant improvement in his complaints. Discussion: The exact mechanism of GBS formation in patients with COVID-19 is yet to be determined. However, prevailing theories suggested that inflammatory cells are stimulated by COVID-19 leading to production of inflammatory cytokines which therefore creates an immune mediated process. Conclusion: proper neurologic assessment is recommended whenever there is a suspicion of GBS following GI and/or respiratory infection.
Keywords
COVID-19, Guillain-barre syndrome, SARS-CoV-2, Respiratory infection, Paralysis
Introduction
Guillain-Barre syndrome (GBS) is an immune mediated disease that often manifests clinically after an infectious process. Patients with GBS classically present with progressive, ascending symmetrical flaccid paralysis with diminished or lost deep tendon reflexes. Cranial nerves paresis may also be observed [1]. In December 2019, the novel coronavirus disease 2019 (COVID-19) was detected in Wuhan City in China [2]. COVID-19 commonly leads to respiratory complications with symptoms similar to the severe acute respiratory syndrome coronavirus-1 (SARSCoV- 1) and Middle East Respiratory Syndrome Coronavirus (MERS-CoV). These symptoms include fever, cough, headaches, dyspnea, myalgia and diarrhea [3]. Other complications such as gastrointestinal complications, cardiac and renal failure were also reported in patients with COVID-19 [4,5]. Moreover, the neurological manifestations of COVID-19 are increasingly reported which include dizziness, headaches, loss of taste and smell, muscle involvement as well as ischemic and hemorrhagic stroke [6]. Interestingly, few papers have recently discussed the incidence of GBS after COVID-19 infection. In this report, we describe a case of GBS that occurred within 3 weeks of COVID-19 infection.
Case Report
On 26th of June 2020, a previously healthy 36-year-old male presented to a primary health care center complaining of cough and diarrhea. COVID-19 was suspected and PCR results confirmed that the patient is positive for SARSCoV- 2. At that time, the patient was on supportive care and quarantine for a total of 14 days without requiring medication or admission. Two weeks later (11th of July), the patient woke up with bilateral progressive distal extremity numbness and within 4 days the patient developed speech impairments and bilateral facial weakness. Bowl and bladder incontinent, fatigue and respiratory symptoms were not observed. In the emergency department of a privet hospital, he was diagnosed with Bell's palsy and started treatment on prednisolone. Two days later, the patient felt that his bilateral distal extremity numbness improved but still had no change on his bilateral facial weakness. After 5 days of steroid, the patient was referred to King Fahd Medical City a specialized tertiary hospital in the field of neurology and neurosciences.
On examination, he was conscious, alert, oriented to time place and person. Cranial nerves examination was normal except for bilateral lower motor neuron facial weakness, more to the left with mild dysarthria. Motor examination revealed no muscles wasting and normal tone. The patient scored 5 in the Medical Research Council (MRC) scale for muscle strength and his upper and lower limbs contracted normally against full resistance. Coordination was grossly normal. However, the patient presented diminished triceps reflexes and did not show knee and ankle bilateral reflexes, bicep and supinator. Sensory examination revealed decreased sensation on bilateral feet and hand with normal temperature, proprioception and vibration. Gait exam was unremarkable. Lumbar puncture was performed but failed due to vasovagal symptoms. The patient was informed about his progressive sensory and motor polyneuropathy and agreed to start on IVIG 0.4 mg/kg for 5 days with physical therapy.
Further examinations using Fluoroscopic guided lumbar puncture revealed CSF WBC count of 1 (0-5 ), Glu count of 4.3 mmol/L (2.22 - 3.89 mmol/L), Protein count of 1.93 (0.15 - 0.4 g/L), and negative PCR findings for HSV 1&2, entoervirus, MTB DNA complex, VZV, CMV and brucella. Serological investigations found low Vitamin D (33), normal Vitamin B12 (351) and normal thyroid function test.
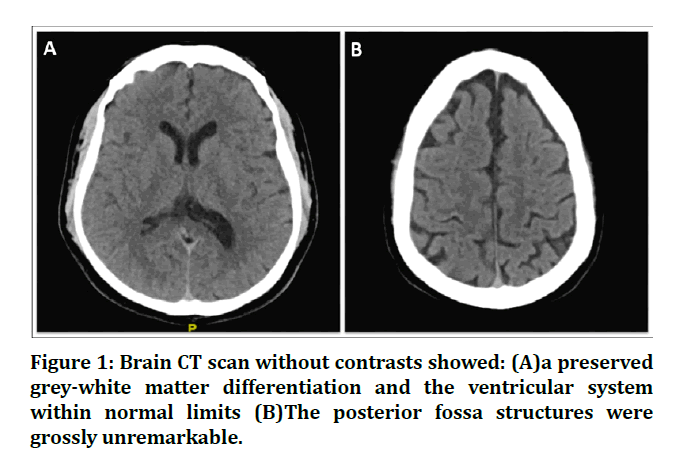
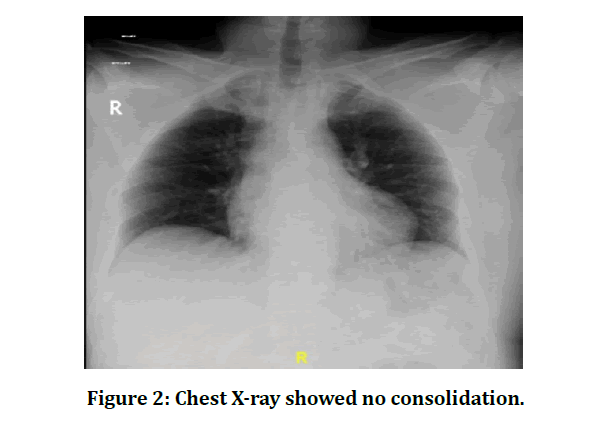
Nerve conduction studies were performed at day 20 of the onset of neurological symptoms. Sensory nerve conduction studies showed absent sensory nerve action potentials (SNAPs) from the median and superficial peroneal nerves with preserved sural SNAPs. Motor conduction studies showed significantly delayed distal motor latency (DML), respectively) in demyelinating range (>130% ULL) in the right median (10.9 ms) and left peroneal (12.0 ms) nerves with borderline low compound muscle action potentials (CMAPs) in the right median (3.6 mV) and preserved CMAP in the left peroneal (3.0 mV) with slow conduction velocities. There was no evidence of conduction block or temporal dispersion. Right peroneal CMAPs were absent. Tibial and ulnar motor nerves showed slow conduction velocities bilaterally. Minimum F-wave latencies were prolonged in the right median and left peroneal nerves (Figures 1 and 2).
Figure 1: Brain CT scan without contrasts showed: (A)a preserved grey-white matter differentiation and the ventricular system within normal limits (B)The posterior fossa structures were grossly unremarkable.
Figure 2: Chest X-ray showed no consolidation.
On day 5 of admission, patient bilateral lower motor neuro facial weakness was improved and controlled with IVIG. The patient was able to close his eyes with minimal weakness and Bilateral numbness of distal extremities was improving. The patient was then prescribed Gabapentin due to complaining of neuropathic pain in the hands and feet. He was then discharge with outpatient appointment in general neurology clinic. Further repeat of nerve conduction studies after 3 weeks, showed remarkable improvement in all parameters. Right median and peroneal DMLs improved to 6.9 ms and 6.1 ms respectively with normalization of CMAPs and conduction velocities. Right median and left peroneal SNAPs were recordable. A month later, the patient presented to the clinic without showing any sensory symptoms but there was still mild residual for the bilateral lower motor neuro facial weakness. The patient was advised to continue physical therapy.
Discussion
GBS is an autoimmune disorder characterized by rapidly progressive limb weakness accompanied by cranial nerves or sensory deficits. This syndrome typically occurs after respiratory tract or gastrointestinal infection, mostly six weeks after infection [7]. COVID-19 clinical manifestations resemble those of SARS- 1 and MERS with a number of neurological manifestations being reported [6,8]. The first report that discussed an association of COVID-19 and GBS was published by Zhao and colleagues [9]. This case presented initially with GBS symptoms followed by symptoms of SARS-CoV-2 eight days from initial presentation. Sedaghat and Karimi reported a case of GBS that was diagnosed two weeks after COVID-19 infection in a 65-year-old gentleman confirmed by electrophysiological examinations [10]. A recent systematic review on GBS after COVID-19 identified a total of 18 cases [11]. Most cases were from Europe with only 2 cases reported from the Middle East. All patients were symptomatic for SARS-CoV-2 and all had classical clinical presentation of GBS except for two who had bilateral facial palsy, two with paraparetic type, and one with a pure motor GBS. Cranial nerve involvement was evident in 61% of patients. In cases where electrophysiological studies were performed, acute inflammatory demyelinating polyneuropathy (AIDP), acute motor and sensory axonal neuropathy (AMSAN) and acute motor axonal neuropathy (AMAN) were the most commonly reported subtypes in descending order. Cerebrospinal fluid (CSF) examination determined increased protein level and albuminocytological dissociation with normal cell count in 61% of patients. In addition, all patients who were tested for antigangliosides antibodies showed negative results. The mean time from onset of symptoms of COVID-19 and the first symptoms of GBS was 9 days which is similar to the interval of GBS seen during or after other infections [1,12].
The exact mechanism of GBS formation in patients with COVID-19 is yet to be determined. However, prevailing theories suggested that inflammatory cells are stimulated by COVID-19 leading to production of inflammatory cytokines which therefore creates an immune mediated process. This can possibly induce the formation of antibodies against specific gangliosides that may appear with certain types of GBS [3,10,13]. Dysregulation of the autoimmune system secondary to COVID-19 has also been proposed [14,15]. In addition, Alberti and colleagues suggested that peripheral nerve involvements in patients with COVID-19 can manifest clinically even before the resolution of pneumonia [16].
Conclusion
Detailed history taking with proper neurologic examination followed by laboratory and radiology investigation are highly recommended whenever there is a suspicion of GBS following GI and/or respiratory infection.
Study Funding
No targeted funding reported. The article processing charge was funded by the authors.
Acknowledgements
The authors would like to thank the National Neuroscience Institute and the Research Center at King Fahd Medical City, Riyadh, for their valuable help and support.
Decleration of Interests
Authors have nothing to declare with respect to the research, authorship, and/or publication of this article.
References
- Sejvar JJ, Baughman AL, Wise M, et al. Population incidence of Guillain-Barré syndrome: A systematic review and meta-analysis. Neuroepidemiol 2011; 36:123-133.
- Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J Med Virol 2020; 92:401-402.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395:497-506.
- Chen L, Liu H, Liu W, et al. Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia. Chinese J Tuberculosis Respir Dise 2020; 43:e005.
- Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020; 323:1406-1407.
- Mao L, Wang M, Chen S, et al. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: A retrospective case series study. MedRxiv 2020.
- Webb S, Wallace VC, Martin-Lopez D, et al. Guillain-Barré syndrome following COVID-19: A newly emerging post-infectious complication. BMJ Case Reports 2020; 13:e236182.
- Sahin AR, Erdogan A, Agaoglu PM, et al. 2019 novel coronavirus (COVID-19) outbreak: A review of the current literature. EJMO 2020; 4:1-7.
- Zhao H, Shen D, Zhou H, et al. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol 2020; 19:383-384.
- Sedaghat Z, Karimi N. Guillain Barre syndrome associated with COVID-19 infection: A case report. J Clin Neurosci 2020; 76:233-235.
- De Sanctis P, Doneddu PE, Viganò L, et al. Guillain Barré syndrome associated with SARSâ?CoVâ?2 infection. A systematic review. Eur J Neurol 2020; 27:2631-2370.
- Toscano G, Palmerini F, Ravaglia S, et al. Guillain–Barré syndrome associated with SARS-CoV-2. New England J Med 2020; 382:2574-2576.
- Jacobs B, Rothbarth P, Van der Meché F, et al. The spectrum of antecedent infections in Guillain-Barré syndrome: A case-control study. Neurology 1998; 51:1110-1115.
- McGonagle D, Sharif K, O'Regan A, et al. Interleukin-6 use in COVID-19 pneumonia related macrophage activation syndrome. Autoimmunity Reviews 2020; 102537.
- Qin C, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infectious Diseases 2020; 71:762-768.
- Alberti P, Beretta S, Piatti M, et al. Guillain-Barré syndrome related to COVID-19 infection. Neurol Neuroimmunol Neuroinflammation 2020; 7.
Author Info
Aqeel Almutairi*, Sarah Bin Abdulqader, Majed Alhameed, Sajjad Ali, Bandar Alosaimi and Rakan Alotaibi
1National Neuroscience Institute, King Fahad Medical City, Riyadh, Saudi Arabia2Research Center, King Fahad Medical City, Riyadh, Saudi Arabia
3King Abdulaziz University, KSA, Saudi Arabia
Citation: Aqeel Almutairi, Sarah Bin Abdulqader, Majed Alhameed, Sajjad Ali, Bandar Alosaimi, Guillain-BarrE Syndrome Following COVID-19: A Case Report, J Res Med Dent Sci, 2021, 9 (3): 7-10.
Received: 07-Jan-2021 Accepted: 08-Mar-2021 Published: 15-Mar-2021