Research - (2021) Volume 9, Issue 6
Haematological Abnormalities in Decompensated Chronic Liver Disease
E Halleys Kumar and A Radhakrishnan*
*Correspondence: A Radhakrishnan, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
To assess the haematological abnormalities a decompensated chronic liver disease this study. was conducted in sree balaji medical college and hospital. About 100 patients were admitted as inpatients and out patients were taken up to assess the haematological profile. First all the patients were evaluated for the diagnosis of cirrhosis. Once the patient has been diagnosed, patients underwent haematological profile. Investigations such as ultrasound abdomen, UGI scopy were done to confirm the diagnosis. Then blood investigations such as RBC, WBC, platelets, reticulocyte count, peripheral smear were done to find out the type of anaemia, nature of anaemia, type of RBCS, WBC count and defects in platelets. All the investigations were done and results are obtained. According to the study the type of anaemia which is more prevalent in cirrhosis is normocytic normochromic anaemia. Microcytic and macrocytic anaemia is more common m males in my study. Macrocytosis is more common in alcoholics. Leucocytosis occurs in patients due to repeated paracentesis and bacterial peritonitis and leucopenia occurs in only smaller number of patients. Eosinophilia is due to parasitic infections. Thrombocytopenia is present in cirrhotic patients.
Keywords
Cirrhosis, Anaemia, Microcytic, Macrocytic, Carcinoma
Introduction
Liver is the largest organ of the body, weighing 1-1.5kg and representing 1.5-2.5 percentage of the lean body mass. The liver is located in the right upper quadrant of the abdomen under the right lower rib cage against the diaphragm and projects for a variable extent into the left upper quadrant. The liver is held in place by ligamentous attachments to the diaphragm, peritoneal, great vessels and upper gastrointestinal organs. It receives a dual blood supply 20 percent of the blood flow is oxygen rich blood from hepatic artery and 80 percent is nutrient rich blood from portal vein arising from the stomach, intestines, pancreas and spleen. The majority of cells in the liver are hepatocytes, which constitute 213rd of the mass of the liver. Remaining cell types are kupffer cells, stellate cells, endothelial cells and blood vessels, bile ductular cells and supporting structures.
Liver performs numerous and vital roles in maintaining homeostasis and health. It plays a major role in carbohydrate, lipid and protein metabolism. Liver is the major storage site for iron, vitamin b12 and folic acid. The liver is involved in or is responsible for various haematologica abnormalities due to its uruque portal circulation and its synthetic (clotting factors, thrombopoietin) and immune functions. Primary liver problems like cirrhosis can lead to haematological abnormalities and primary haematological diseases can in turn affect the liver and its functioning Cirrhosis is a condition that is defined histopathological and has a variety of clinical manifestations and complications, some of which can be life threatening. Abnormalities in haematological indices are frequently encountered in cirrhosis. Multiple causes contribute to the occurrence of hematological abnormalities. Recent studies suggest that the presence of hematological cytopenias is associated with a poor prognosis in cirrhosis. The study was conducted to assess the hematological abnormalities and the nature of hematological abnormalities, so that treatment can be initiated towards reducing the morbidity.
Cirrhosis is a condition that is defined histopathological and has a variety of clinical manifestations and complications, some of which can be life-threatening. In the past, it has been thought that cirrhosis was never reversible; however, it has become apparent that when the underlying insult that has caused the cirrhosis has been removed, there can be reversal of fibrosis. This is most apparent with the successful treatment of chronic hepatitis C; however, reversal of fibrosis is also seen in patients with hemochromatosis who have been successfully treated and in patients with alcoholic liver disease who have discontinued alcohol use. Regardless of the cause of cirrhosis, the pathologic features consist of the development of fibrosis to the point that there is architectural distortion with the formation of regenerative nodules. This results in a decrease in hepatocellular mass, and thus function, and an alteration of blood flow. Clinical features of cirrhosis are the result of pathologic changes and mirror the severity of the liver disease.
The grading and staging schemes vary between disease states and have been developed for most conditions, including chronic viral hepatitis, non-alcoholic fatty liver disease, and primary biliary cirrhosis. Advanced fibrosis usually includes bridging fibrosis with nodularity designated as stage 3 and cirrhosis designated as stage 4. Early and well-compensated cirrhosis can manifest as anorexia and weight loss, weakness, fatigue, and even osteoporosis as a result of vitamin D malabsorption and subsequent calcium deficiency. Decompensated disease can result in complications such as ascites, spontaneous bacterial peritonitis, hepatic encephalopathy, and variceal bleeding from portal hypertension Patients who have developed complications of their liver disease and have become decompensated should be considered for liver transplantation. Many of the complications of cirrhosis will require specific therapy. Portal hypertension is a significant complicating feature of decompensated cirrhosis and is responsible for the development of ascites and bleeding from esophagogastric varies, two complications that signify decompensated cirrhosis [1-21].
Materials and Methods
Study population
To asses the hematological abnormalities m decompensated chronic liver disease, the prevalence study was conducted in sree balaji medical college and hospital from 2011 to 2013.
About hundred patients were selected in random for this study , from patients coming to department of general medicine opd and ward patients.
Inclusion criteria
All liver disease patients whose symptoms and signs persists more than six months.
Alcoholic, post infective, metabolic causes of liver diseases are taken for study.
Exclusion criteria
Patients with known primary hepatocellular carcinoma or GI malignancies.
Acute liver cell failure.
Description of study
• Blood investigations such as complete blood count, liver function test, UGI scopy and ultrasound abdomen were done for all the patients. ONCE the patients were confirmed as a case of decompensated chronic liver disease then the patients were said to undergo other tests such as RBC, Hb, WBC, platelets ,reticulocyte count and peripheral smear.
• Peripheral smear was done to find the type of anaemia.
• Oral and written consent of the patients got for the clinical examination and for the lab investigations.
• A detailed history and blood investigations like complete blood count, liver function test, UGI scopy, ultrasound abdomen would be done.
• Presenting complaints of the patients were taken in detail such as abdominal pain, abdominal distension, and decreased urine output, yellowish discolouration of urine and eyes, loss of appetite, loss of weight, early satiety and fever.
• Past history regarding the presence of diabetes mellitus, systemic hypertension, ischemic heart disease, tuberculosis were all got from the patient.
• Personal history such as alcohol intake (amount and years) , smoking ( pack per day/ yrs), betel nut chewing were got from the patient.
• Family history of any liver disease was also noted.
• Patients were taken a detailed general and systemic examination.
Ultrasonography
Abdominal ultrasonography with Doppler is a noninvasive, widely available modality that provides valuable information regarding the gross appearance of the liver and blood flow in the portal and hepatic veins in patients suspected to have cirrhosis.
Ultrasonography should be the first radiographic study performed in the evaluation of cirrhosis because it is the least expensive and does not pose a radiation exposure risk or involve intravenous contrast with the potential for nephrotoxicity as does computed tomography (CT). Nodularity, irregularity, increased echogenicity, and atrophy are ultrasonography hallmarks of cirrhosis. In advanced disease, the gross liver appears small and multinodular, ascites may be detected, and Doppler flow can be significantly decreased in the portal circulation. The discovery of hepatic nodules via ultrasonography warrants further evaluation because benign and malignant nodules can have similar ultrasonography appearances [22].
A study using high-resolution ultrasonography in patients with cirrhosis confirmed with biopsy or laparoscopy found a sensitivity and specificity for cirrhosis of 91.1 and 93.5 percent, respectively, and positive and negative predictive values of 93.2 and 91.5 percent, respectively [23].
After establishing the diagnosis patients were evaluated for hematological abnormalities .
All complete blood investigations were done in pathology laboratory in sree balaji medical college and hospital.
RBC count
RBC count was done in neubauers chamber using hayems fluid or auto analyser. normal value: 4.5 to 5.5 millon per cu mm.
Haemoglobin estimation
Done by sahlis method, based on the conversion of haemoglobin to acid hematin or acid analyser. normal values : male 14 to 18 gm/dl female 12 to 16 gm/dl.
Packed cell volume
Done by auto analyser or microhematocrit capillary method normal value: male 42 to 52 percent female 37 to 47 percent.
Peripheral smear for blood picture
Low power field examination.
High power field examination.
Oil immersion examination.
WBC abnormality
Done by QBC method or using neubauers chamber with turks fluid. normal value: 4000 to 11,000 cells per cu mm.
Upper GI endoscopy
UGI scopy was done at the medical gastroenterology department. Patient was explained about the procedure and side effects. Results were correlated for establishing the diagnosis.
Results
Figure 1 show about 100 patients were taken for the study and about 70 males and 30 females. Out of this 8 males ( 11.4 percent) and 4 females (13.3 percent belong to younger age group, about 55 males and 20 females in the middle age group, about 7 males and 6 females in the elderly age group.
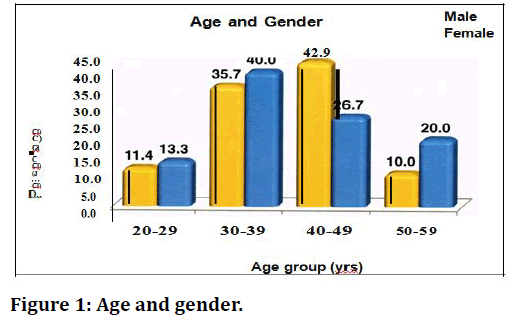
Figure 1. Age and gender.
Table 1 shows hemoglobin abnormalities in decompensated chronic liver disease patients. (70 males and 30 females).
| Haemoglobin ( gm/dl) | Gender | Total | ||||
|---|---|---|---|---|---|---|
| Male | Female | |||||
| N | % | N | % | N | % | |
| SEVERE (<6gm/dl) | 10 | 14.3 | 6 | 20 | 16 | 16 |
| MODERATE ( 6 TO 8.9/dl) | 30 | 42.9 | 12 | 40 | 42 | 42 |
| MILD ( 9 TO 12.9gm/dl) | 20 | 28.6 | 8 | 26.7 | 28 | 28 |
| NORMAL | 10 | 14.3 | 4 | 13.3 | 14 | 14 |
| Total | 70 | 100 | 30 | 100 | 100 | 100 |
Table 1: Haemoglobin (Anaemia in chronic liver disease patients).
• In this study we found that 10 males(14.3 percent), 6(20 percent) of the patients had severe anemia
• 30 males (42.9 percent), 12 females (40.0 percent) had moderate anaemia and 20 males (28.6percent), 8 females (26.7 percent) had mild anaemia.
• About 10 males and 4 females had normal haemoglobin levels. iv) Female patients had a greater proportion of severe anaemia in other studies contrary to our study in which male patients has severe anaemia compared to females.
• Female patients had a greater proportion of severe anaemia in other studies contrary to our study in which male patients has severe anaemia compared to females.
Macrocytic anaemia is more common among alcoholics. About 18 males(30 percent) and 6 females (23 percent) had microcytic hypochromic anaemia about 11 m£ \les(l8.3 percent) and 4 females(l5.4 percent) had macrocytic anaemia. All males gave history of alcoholism. 1 male (l.7 percent) and 1 female (3.8 percent) had dimorphic anaemia. About 10 males and 4 females had normal haemoglobin level (14 patients) Table 2).
| Type of RBCS | Patients with anaemia | Total | ||||
|---|---|---|---|---|---|---|
| Male | Female | |||||
| N | % | N | % | N | % | |
| Normocytic | 30 | 50 | 15 | 57.7 | 45 | 16 |
| Microcytic | 18 | 30 | 6 | 23.1 | 24 | 42 |
| Macrocytic | 11 | 18.3 | 4 | 15.4 | 15 | 28 |
| Dimorphic | 1 | 1.7 | 1 | 3.8 | 2 | 14 |
| Total | 60 | 100 | 26 | 100 | 86 | 100 |
Table 2: Type of anaemia in chronic liver disease patients.
Table 3 showing WBC count in decompensated chronic liver disease patients. About 24 males (34.3 percent) and 12 females (40 percent) had leucocytosis. Only 3 males (4.3 percent) and 1 females (3.3 percent) had leucopenia. Leucocytosis is more prevalent than leucopenia in decompensated chronic liver disease patients in my study of about 100 patients. about 36 patients had leucocytosis and is due to Infection (community acquired infection, nosocomial infection, spontaneous bacterial peritonitis and secondary peritonitis due to repeated peritoneal paracentesis. about 30 to 40 percent of the patients with leucocytosis had high grade fever and showed increase in polymorphs in ascetic fluid. 4 patients had leucopenia and may be due to hypersplenism. Chronic inflammatory cytokines which has a suppresor effect on bone marrow. Direct action of alcohol on bone marrow infection.
| Total Count ( IN CU.MM) | Gender | Total | ||||
|---|---|---|---|---|---|---|
| Male | Female | |||||
| N | % | N | % | N | % | |
| <4000 | 3 | 4.3 | 1 | 3.3 | 4 | 4 |
| 4000-5999 | 10 | 14.3 | 6 | 20 | 16 | 16 |
| 6000-7999 | 15 | 21.4 | 5 | 16.7 | 20 | 20 |
| 8000-11000 | 18 | 25.7 | 6 | 20 | 24 | 24 |
| >11,000 | 24 | 34.3 | 12 | 40 | 36 | 36 |
| Total | 70 | 100 | 30 | 100 | 100 | 100 |
Table 3: WBC count in decompensated chronic liver disease patients.
Table 3 shows platelet count in decompensated chronic liver disease patients.
• In my study, thrombocytopenia is seen in 38 males and 18 females with (22.9 percent) of the males and (22 percent) of the females has thrombocytopenia.
• Severe thrombocytopenia is seen in 16 males and 6 females.
• 22 males and 12 females had mild to moderate thrombocytopenia
• There were no patients with thrombocytosis.
• Remaining patients had normal platelet count.
Discussion
Anaemia in cirrhosis is mostly due to haemodilution, decreased erythropoietin level as per study siciliano hepatol 1995 who showed decreased erythropoietin level in cirrhotic patients with anaemia. Cirrhosis without anaerrua is not associated with low erythropoietin levels where as Yang et al [24] investigated the significance of erythropoietin in 67 patients with varying severity of cirrhosis, and reported that plasma erythropoietin levels were significantly higher in cirrhotic patients than in controls. They also found levels to be higher in patients with anemia. Inflammatory cytokines suppressing the bone marrow (chronic inflammation) g) Folic acid and vitamin B12 deficiencies and iron deficiency develop frequently in patients with cirrhosis producing severe anaemia. Of diverse etiology occurs in about 75% of patients with chronic liver disease [25] according to sheila sherlock and oxford text book of hepatology. Most common anaemia seen in cirrhotic patients 1s normochromic and normocytic anaemia [26,27]. In a previous study it is reported 43 percent of macrocytosis supported by bingham et al. macrocytic Anemia in an alcoholic anse as a consequence of the direct toxic effects of alcohol on erythrocyte precursors in the bone marrow.
Folic acid and vitamin B12 deficiencies develop frequently in patients with cirrhosis. These deficiencies may be related to inadequate food intake or intestinal malabsorption. They are suspected when examination of a blood film reveals hyper segmented cells and oval macrocytes, m addition to round macrocytes characteristic of chronic liver disease. When anemia is caused by these deficiencies, the mean corpuscular volume 1s increased and bone marrow shows megaloblastic erythropoiesis. Consumption of alcohol appears to be associated with an approximately 40% reduction in the risk of development of iron deficiency anemia. Acute gastrointestinal haemorrhage 1s a common and potentially senous complication of portal hypertension [28-3l]. Acute haemorrhage may induce severe hypovolemia and subsequently secondary iron deficiency anemia. Esophageal and gastric vances and/or portal hypertensive gastropathy may be associated with slow chronic loss of blood into the gut and development of chronic iron deficiency anemia.The most important approach to management is prevention of variceal haemorrhage [28,30,31]. serum iron is bound to beta globulin transferrin and total iron binding capacity largely depends on transferrin concenteration. Acanthocytosis or spur cells can refer generally to the presence of this type of crenated red blood cell, such as may be found in severe cirrhosis or pancreatitis [32,33], they are a bad prgnostic indicator.these abnormal rbcs are not found in our study.
According to sheila sherlock leucopenia thrombocytopenia are commonly found in cirrhotics. Liangpunsakul et al [34] reported that the presence of severe hypersplenism independently predicted the development of variceal bleeding and death. eosinophilia is seen in association with parasitic diseases and also associated with hepatic vein thrombosis, hepatocellular carcinoma [35]. It is also seen in primary biliary cirrhosis. Disease of platelet number and function are well documented in patients with chronic disease contributing significantly to their hemostatic abnormalities [36]. Thrombocytopenia (platelet count < 150,000/L) 1s common in patients with chronic liver disease; it has been reported in as many as 76% of patients with cirrhosis [37,38]. The pathogenesis of the thrombocytopenia is complex; it includes splenic pooling, and increased destruction and impaired production of platelets. Impaired production of platelets is caused, at least in part, by low levels of thrombopoietin. Prolonged bleeding time, and impaired aggregation, reduced adhesiveness and abnormal ultrastructure of platelets reflect abnormal platelet function; these abnormalities have been attributed to an intrinsic platelet defect. Specific treatments to attempt to reverse the effects of this defect are not usually given, but platelet transfusions or platelet-stimulating agents have been administered in some cases. Felix et al [39] compared leukopenia and thrombocytopenia among patients treated with either a portocaval shunt or conventional medical therapy. Patients in the medical group did not receive beta blockers or nitrates. Thrombocytopenia improved in 43% of subjects in the surgical group compared with 0% in the medical group. Gschwantler et al [39,40] showed an, average increase of 19% in platelet count after the placement of TIPS compared with a 17% decrease in controls. In another previous study it is reported that a subgroup of patients that had TIPS placed for ascites in whom the platelet count increased by more than 25%.
Conclusion
This study was conducted for 100 patients coming to our hospital. 86 percentages of patients had anaemia in some form. Normocytic normochromic anaemia is most common type of anaemia present in our study in patients having cirrhosis. Microcytic anaeffila 1s more common m men than women in my study. Macrocytic anaemia patients gave history of alcoholism. Abnormal red cells such as microcytes, macrocytes, target cells, anisocytosis are found to be common in cirrhosis. As anaemia is prevalent in 86 percent of patients, it become essential that we screen all the patients with chronic liver disease for anaemia and treat accordingly to reduce morbidity and mortality. Leucocytosis 1s more common m patients with spontaneous bacterial peritonitis and secondary peritonitis. Hence a simple screening test like WBC count will help us to pick up infections like spontaneous bacterial peritonitis and secondary peritonitis and treat accordingly to reduce morbidity and mortality. Leucopenia is found to be rare in my study.
Thrombocytopenia is present in 48 percent of the patients, whereas no patients had thrombocytosis. Hence with this study all the cirrhosis patients should be screened for hematological abnormalities, and necessary investigations and treatment should be done to prevent morbidity and mortality. In my study 86 percent had anaemia, 36 percent had leucocytosis and 56 percent had thrombocytopenia. Which indicates that earlier diagnosis of hematological abnormalities in decompensated chronic liver disease patients would help us to treat patients earlier and prevent morbidity and mortality?
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgement
The encouragement and support from Bharath University, Chennai, is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Zieve L. Jaundice, hyperlipidemia and hemolytic anaemia: A heretofore unrecognized syndrome associated with alcoholic liver cirrhosis. Ann Intern Med 1958; 48:471-96.
- Roberts EA, Schilsky ML. American association for study of liver diseases (AASLD). Practice guidelines on wilson disease. Hepatology 2003; 37:1475-92.
- Manns MP, McHutchison JG, Gordon SC, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: A randomised trial. Lancet 2001; 358:958-65.
- Macdougall IC. CERA (Continuous erythropoietin receptor activator): A new erythropoiesis-stimulating agent for the treatment of anemia. Curr Hematol Rep 2005; 4:436-40.
- Young NS. Acquired aplastic anemia. Ann Intern Med 2002; 136:534-46.
- Mathur M, Wanjari K, Turbadkar D. Seroprevalence of HIV, Hepatitis C and hepatitis B multitransfused thalassemics. Indian J Med Microb 2008; 26:205-6.
- Ghosh K, Joshi SH, Shetty S, et al. Transfusion transmitted diseases in haemophiliacs from western India. Indian J Med Res 2000; 112:61-4.
- Ong JP, Younossi ZM. Managing the hematologic side effects of antiviral therapy for chronic hepatitis C: Anemia, neutropenia, and thrombocytopenia. Cleve Clin J Med 2004; 7l:Sl7-21.
- Gurakar A, Fagiuoli S, Gavaler JS, et al. The use of granulocyte macrophage colony-stimulating factor to enhance hematologic parameters of patients with cirrhosis and hypersplenism. J Hepatol 1994; 21:582-6.
- Kumar EH, Radhakrishnan A. Prevalence of anaemia in decompensated chronic liver disease. World J Med Sci 2014; 10:56-60.
- Giannini EG. Review article: Thrombocytopenia in chronic liver disease and pharmacologic treatment options. Aliment Pharmacol Ther 2006; 23:1055-65.
- Afdhal N, McHutchison J, Brown R, et al. Thrombocytopenia associated with chronic liver disease. J Hepatol 2008; 48:1000-7.
- Peck-Radosavljevic M. Hypersplenism. Eur J Gastroenterol Hepatol 2001; 13:317-23.
- Rajan SK, Espina BM, Liebman HA. Hepatitis C related thrombocytopenia clinical and immune laboratory characteristics compared with chronic immune thrombocytopenic purpura. Br J Haematol 2005; 129:818-24.
- Bauduer F, Marty F, Larrouy M, et al. Immunologic thrombocytopenic purpura as presenting symptom of hepatitis C infection. Am J Hematol 1998; 57:338-340.
- Garcia-Suarez J, Burgaleta C, Hernanz N, et al. HCV-associated thrombocytopenia: clinical characteristic and platelet response after recombinant alpha 2b interferon therapy. Br J Haematol 2000; 110:98-103.
- McHutchison JG, Dusheiko G, Shiffman ML, et al. Eltrombopeg for thrombocytopenia in patients with cirrhosis associated with hepatitis C. N Engl J Med 2007; 357:2227-36.
- Peck-Radosavljevic M, Zacherl J, Meng YG, et al. Is inadequate thrombopoietin production a major cause of thrombocytopenia in cirrhosis of the liver? J Hepatol 1997; 27:127-31.
- Rios R, Sangro B, Herrero I, et al. The role of thrombopoietin in the thrombocytopenia of patients with liver cirrhosis. Am J Gastroenterol 2005; 100:1311-6.
- Fried MW, Shiffman ML, Reddy KR, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med 2002; 347:975-82.
- Laffi G, Tarquini R, Marra F. Thrombocytopenia in chronic liver disease: Lessons from transplanted patients. J Hepatol 2007; 47:625-9.
- American college of radiology, expert panel on gastrointestinal imaging. Liver lesion characterization. Reston 2002.
- Simonovsky V. The diagnosis of cirrhosis by high resolution ultrasound of the liver surface. Br J Radiol 1999; 72:29-34.
- Yang YY, Lin HC, Lee WC, et al. Plasma erythropoietin level in patients with cirrhosis and its relationship to the severity of cirrhosis and renal function. J Gastroenterol Hepatol 2003; 18:1156-61.
- McHutchison JG, Manns MP, Longo DL. Definition and management of anemia in patients infected with hepatitis C virus. Liver Int 2006; 26:389-398.
- http://repository-tnmgrmu.ac.in/6640/1/200100107durai_mavalavan.pdf
- Anbazhagan G, Mohan Raj P, Kalaivalli S, et al. Red blood cell abnormalities in decompensated chronic liver disease (DCLD). J Evidence Based Med Hlthcare 2015; 2:826-833.
- Garcia-Pagan JC, De Gottardi A, Bosch J. Review article: The modern management of portal hypertension--primary and secondary prophylaxis of variceal bleeding in cirrhotic patients. Aliment Pharmacol Ther 2008; 28:178-186.
- Abraldes JG, Bosch J. The treatment of acute variceal bleeding. J Clin Gastroenterol 2007; 41:S312-S317.
- Kravetz D. Prevention of recurrent esophageal variceal hemorrhage: review and current recommendations. J Clin Gastroenterol 2007; 41:S318-S322.
- Albillos A. Preventing first variceal hemorrhage in cirrhosis. J Clin Gastroenterol 2007; 41:S305-S311.
- Carr JM. Disseminted intravascular coagulation Ill cirrhosis. Hepatology 1989; 10:103-10.
- https://hemonc.mhmedical.com/book.aspx?bookID=1802
- Liangpunsakul S, Sithat M, Ulmer B, et al. Predictors and implications of severe hypersplenism in patients with cirrhosis. Am J Med Sciences 2003; 326: 111-16.
- Durai Mavalavan VM. Haematological abnormalities in decompensated chronic liver disease (Doctoral dissertation, Madras Medical College, Chennai).
- van Vlierbergh H, Delanghe JR, De Vos M, et al. Factors influencing ribavirin-induced hemolysis. J Hepatol 2001; 34:911-916.
- Afdhal N, McHutchison J, Brown R, et al. Thrombocytopenia associated with chronic liver disease. J Hepatol 2008; 48:1000-1007.
- Felix WR, Myerson RM, Sigel B, et al. The effect of portocaval shunt on hypersplenism. Surg Gyn Obs 1974; 139:899-904.
- Gschwantler M, Vavrik J, Gebauer A, et al. Course of platelet counts in cirrhotic patients after implantation of a transjugular intrahepatic portosystemic shunt-A prospective, controlled study. J Hepatol 1999; 30:254-9.
- Balarama G, Ashok M, Satheesh Kanna V, et al. Chemotherapeutic effect of farnesol against N-Diethyl nitrosamine (DEN) Induced experimental hepatocellular carcinoma in rats. Int J Scientific Res Sci Technol 2018; 4.
Author Info
E Halleys Kumar and A Radhakrishnan*
1Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, IndiaCitation: E Halleys Kumar, A Radhakrishnan, Haematological Abnormalities in Decompensated Chronic Liver Disease, J Res Med Dent Sci, 2021, 9(6): 360-367
Received: 06-May-2021 Accepted: 23-Jun-2021 Published: 30-Jun-2021
