Research - (2021) Volume 9, Issue 6
Histopathological and Immunohistochemical Study of the Prostatic Lesions
*Correspondence: Bheemarao, Department of Pathology, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
Benign nodular hyperplasia and adenocarcinoma are the most common diseases encountered in the aging population. Screening protocols and awareness programs over the years significantly reduced the morbidity and mortality. Chronic prostatitis is the commonest inflammatory condition associated with the benign lesions. Conventional adenocarcinoma forms the most common type of prostatic adenocarcinoma and is moderately to poorly differentiated, as graded by Gleason's microscopic grading. The present study was hypothesized that use Immunohistochemical marker p63 along with racemase marker may help to differentiate the benign from malignant prostatic lesions in diagnostically challenging cases effectively.
Keywords
Prostate cancer, Adenocarcinoma, p63, Racemase, Lesions, Prostatitis
Introduction
The word prostate was derived from the Greek word "Prostates", literally meaning "One who stands before" (protector or guardian). The prostate was first described by Venetian anatomist Niccolos Massa in1536 and illustrated by Flemish anatomist Andreas Vesalius in 1538 [1]. Prostate gland occupies centre stage in the lives of many elderly males. Because of its location at bladder neck, enlargement of the gland leads to problems related to urinary obstruction. Incidence of prostatic disease, Benign Nodular Hyperplasia (BNH) and carcinoma prostate increases with age [2]. A recent American Urological Association (AUA) guidelines (2010) suggest an increase in the incidence of Benign Nodular Hyperplasia worldwide and predicts by the age of 60yrs, more than 50% of men will have microscopic evidence of disease [3].
Very few studies conducted on BNH patients from India suggest BNH as the most common pathological condition with an incidence of 92.97% [4]. Globally Carcinoma of Prostate is the 5th cause of cancer and 4th in cancer mortality Incidence is highest among black men in United States [5]. Prostatic carcinoma is more common in India compared to other Asian Countries and its incidence is increasing by 3.5% every year due to the westernization [6]. The combination of Digital rectal examination (DRE), Trans rectal Ultrasonogram, Serum Prostate Specific Antigen (S.PSA) estimation, supplemented with biopsy procedures represents a powerful diagnostic tool in the diagnosis of various prostatic lesions [5]. Histopathological examination of prostatic biopsy remains the gold standard for diagnosing all lesions including benign and malignant conditions.
The unrelenting challenge encountered when differentiating limited-volume prostate carcinoma and sometimes subtle variants from its many morphologic m1m1cs has increased the use of ancillary immunohistochemistry in prostate biopsies. The availability of prostate cancer-associated and basal cellassociated markers has been an invaluable addition to diagnostic surgical pathology [7].
Hence the present study is undertaken to study the incidence of benign and malignant prostatic lesions among the Trans Urethrally Resected Prostate (TURP) biopsies. Additionally, the histology of the benign and malignant prostatic lesions was also studied. Further Gleason's microscopic grading for the malignant lesions and p63 expression of the prostatic lesions in selective cases were also evaluated.
Materials and Methods
During the two year period of study between August 2010 to July 2012, 06 TURP specimens were received in the Department of Pathology, Sree Balaji Medical College and Hospital, Bharath University. Relevant clinical data including age, the presenting complaints, digital rectal examination were recorded. S.PSA values were considered in selected cases. In our cases, the TURP specimen ranged in volume from 8 to 20 cc. Every tissue was carefully examined for the presence of yellow and firm or gray hard areas and necrotic areas. Fixation was done by neutral buffered 10% formalin for 12 hrs and then the specimen was submitted for processing. After processing, 4-5μ sections were cut and Hematoxylin and Eosin staining was done.
Haematoxylin and eosin stain
• Sections were deparaffinised and brought to water.
• Stained with Hematoxylin for 5 minutes.
• Rinsed well in running tap water.
• Dehydrated with 1% acid alcohol- 3 to 4 times.
• Rinsed in tap water-30 seconds.
• Stained with 1 % aqueous eosin for 2 minutes.
• Washed in running tap water - 2minutes.
• Sections were dehydrated with graded ethanol, cleared and mounted with DPX (DextrenePolysterene Xylene).
Every slide was examined thoroughly for the presence of benign, premalignant and malignant features. The cases of prostatic adenocarcinoma were graded using Gleason microscopic grading. Other special stains like Alcian blue pH 1, periodic acid schiff (PAS) were performed wherever necessary. Immuno staining with basal cell marker- p63 was done for 20 cases whose S.PSA> 14ng/ml and their immuno expression was noted. Normal prostate glands served as internal positive control. The clinical and histological data so obtained were analyzed and compared with another similar study.
Results
During the period of study (August 2010 to July 2012), 106 TURP specimens were received 1n the Department of Pathology - Sree Balaji Medical College and Hospital, Bharath University. Among the 106 cases of prostatic biopsies, there were 94(88.61 %) cases of Benign Nodular Hyperplasia, 1 (0.94%) case of Prostatic Intraepithelial Neoplasia, 11(10.4%) cases of Carcinoma Prostate observed.
Incidence of prostatic disorders
Benign Nodular Hyperplasia (BNH) was the most common histological lesion encountered (94 cases-88.61%) with maximum incidence in VII decade.
Carcinoma of Prostate was the second most common type of lesion encountered (11 cases-10.4%) and one case of Prostatic intraepithelial neoplasia (PIN) was encountered in the present study (Table 1 and Table 2).
| S. No. | Type | Total Number (%) |
|---|---|---|
| 1 | Total No. Of Prostatic Biopsies | 106 |
| 2 | Total No. of BNH cases | 94(88.67%) |
| 3 | Total No. PIN | 1(0.94%) |
| 4 | Total No. of Carcinoma of prostate | 11(10.4%) |
Table 1: Incidence of prostatic disorders.
| S.No | Age Group Yrs. | BNH | PIN | CA-Prostate | Total cases (%) |
|---|---|---|---|---|---|
| 1 | 41-50 | 8 | 0 | 0 | 8(7.55%) |
| 2 | 51-60 | 29 | 0 | 1 | 30 (28.30%) |
| 3 | 61-70 | 41 | 1 | 6 | 48( 45.30%) |
| 4 | 71-80 | 16 | 0 | 3 | 19(17.92%) |
| 5 | >80 | 0 | 0 | 1 | 1(0 .94% ) |
Table 2: Prostatic disorders: Age incidence.
Clinical presentation
In the present study difficulty in micturition (69 cases) was the most common presentation followed by frequency of micturition (22 cases). 14 cases presented with hesitancy as chief complaint while 16 cases presented with other complaints like burning micturition, retention of urine and hematuria (Table 3).
| S.NO | Clinical features | BNH | PIN | ADENO CA |
|---|---|---|---|---|
| 1 | Difficulty in micturition | 62 | 1 | 6 |
| 2 | Hesitancy | 12 | 0 | 2 |
| 3 | Frequency | 20 | 0 | 2 |
| 4 | Burning micturition | 8 | 0 | 1 |
| 5 | Retention of urine | 2 | 1 | 1 |
| 6 | Hematuria | 1 | 0 | 2 |
Table 3: Clinical presentation.
Digital rectal examination
Out of 94 benign cases, 88 cases were firm where as 6 cases were hard in consistency. Out of 11 malignant cases, 8 cases were hard and 3 were firm in consistency. LGPIN was firm in consistency (Table 4).
| S.No | DRE | BNH | PIN | ADENO CA | Total lesions (%) |
|---|---|---|---|---|---|
| 1 | Firm | 88 | 1 | 3 | 92(86.79%) |
| 2 | Hard | 6 | 0 | 8 | 14(13.21%) |
Table 4: Digital rectal examination.
Prostatic disorders and serum PSA levels
Among the BNH patients, S.PSA levels were obtained from 36 cases out of which 23 cases were noted having the S.PSA levels in the range of 4-20 ng/ml, followed by 7 cases with S.PSA in the range of 0-4 ng/ml. Among the adenocarcinoma patients, S.PSA levels were obtainedfrom 11cases out of which 8 cases were found to have high levels of S.PSA levels in the range of 21 -80ng/ml. The lowest value of serum PSA among the carcinoma prostate patients was 14.5 ng/ml and the highest value noted was 109.5 ng/ml. S.PSA level obtained for PIN patient was 17.4ng/ml (Table 5).
| S.No. | S. PSA ng/ml | BNH (n=36) | Adeno ca (n=ll) | PIN (n=l) |
|---|---|---|---|---|
| 1 | 0-4 | 7 | 0 | 0 |
| 2 | 13 | 0 | 0 | |
| 3 | 10 | 2 | 1 | |
| 4 | 21-40 | 6 | 4 | 0 |
| 5 | 41-60 | 0 | 3 | 0 |
| 6 | 61-80 | 0 | 1 | 0 |
| 7 | > 80 | 0 | 1 | 0 |
| (n=no. of cases) | ||||
Table 5: Prostatic disorders & S. PSA levels.
Microscopic features in benign lesions
In the present study, 94 prostatic specimens were showing Nodular Hyperplasia. The lesions were composed of varying proportions of epithelium and stroma. Corpora amylacea was seen in majority of cases. 17 cases were showing chronic inflammatory cell infiltrate composed of admixture of lymphocytes and plasma cells. 4 cases were associated with Basal cell Hyperplasia characterised by basal cell proliferation and 1 case was associated with squamous metaplasia. 3 cases of Nodular Hyperplasia were associated with foci of AAH characterised by localised well circumscribed proliferation of small glands admixed with larger glands. 2 cases were showing non-specific granulomatous prostatitis with epithelia cell granulomas while 1 case was associated with prostatic abscess characterised by neutrophil aggregate in and around the acini (Table 6).
| S.NO | Microscopic findings | No. of cases (n=94) |
|---|---|---|
| 1 | Nodular Hyperplasia(NH) | 66 |
| 2 | Basal cell Hyperplasia | 4 |
| 3 | Squamous metaplasia | 1 |
| 4 | Atypical Adenomatous hyperplasia | 3 |
| 5 | Chronic prostatitis | 17 |
| 6 | NonSpecific Granulomatous prostatitis | 2 |
| 7 | Prostatic Abscess | 1 |
Table 6: Microscopic findings in benign lesions.
Prostatic intraepithelial neoplasia
Low grade PIN in 1 case showed features of epithelial crowding and stratification. The nuclei were enlarged with anisonucleosis and nuclear chromatin was apparently normal. High grade PIN was associated with carcinoma in 1 case which showed cribriform pattern of glands with luminal bridging and a sieve like pattern. Adjacent area showed small glands infiltrating the stroma (Table 7).
| S.NO | Lesions | No. of cases |
|---|---|---|
| 1 | LGPIN | 1 |
| 2 | HGPIN with Carcinoma | 1 |
Table 7: Prostatic intraepithelial neoplasia.
Microscopic prostate features in carcinoma
11 cases of prostatic carcinoma were identified in the present study. All of them were adeno carcinomas involving the prostate. All of them showed one or more of the different growth patterns and were categorized depending on the predominant growth pattern. In this study, the commonest pattern was the acinar pattern in 6 cases, followed by fused glandular pattern and cribriform pattern in 4 cases and sheets of cells in 3 cases. Cribriform pattern with central necrosis was present 1n one case. Tumor cells arranged in glands, sheets, cords, had nuclear enlargement, hyperchromasia with prominent nucleoli at places (Table 8). The adjacent tissue in these cases showed Nodular Hyperplasia in 5cases, HGPIN in 1 cases and inflammation (Table 9).
| S.NO | Microscopic findings | No. of cases |
|---|---|---|
| 1 | Discrete glands | 6 |
| 2 | Fused glands | 4 |
| 3 | Cribriform pattern | 4 |
| 4 | Sheets | 3 |
| 5 | Cribriform with central necrosis | 1 |
Table 8: Microscopic findings in carcinoma prostate.
| S.NO | Adjacent prostatic tissue | No. of cases |
|---|---|---|
| 1 | Nodular Hyperplasia | 5 |
| 2 | HGPIN | 1 |
| 3 | Inflammation | 2 |
Table 9: Associated findings in carcinoma prostate.
Carcinoma prostate and gleason's score
All of these 11 malignant cases were graded using Gleason's scoring system. Primary grade is assigned to the dominant pattern and secondary grade to the subdominant pattern. The two numeric grades are added to obtain the combined Gleason's score. In tumors with one pattern of arrangement, the number is doubled. Gleason score of 7 was the commonest pattern seen in 5 cases. Gleason score of 8 was seen in 3 cases and 6 were seen in 2 cases. Gleason score of 10 was seen in 1 case (Table 10). Among the 106 cases studied, 94 cases were BNH with associated changes constituting 88.67% of total cases. Adenocarcinoma (11) constitutes 10.4% of total cases and LGPIN (1) constitutes 0.94% of the total cases (Table 11).
| CGS | No. of cases | Gleasons score-Break up |
|---|---|---|
| 6 | 2 | 2(3+3) |
| 7 | 5 | 3(3+4),2(4+3) |
| 8 | 3 | 1(3+5),2(4+4) |
| 9 | 0 | 0 |
| 10 | 1 | 1(5+5) |
Table 10: Combined gleason's score-break up.
| CGS | NO. of cases | % |
|---|---|---|
| 5 TO 7 | 7 | 63.63% |
| 8 TO 10 | 4 | 36.40% |
Table 11: Incidence of carcinoma with gleason's score.
Mucin histochemistry in prostatic lesions
20 cases were selected for PAS and alcian blue staining, including 8 cases of Nodular Hyperplasia, 11 cases of adenocarcinoma and 1 case of low grade PIN (Table 12).
| HPE (no.of cases) | PAS | Alcian blue |
|---|---|---|
| BNH(8) | Positive | Negative |
| LGPIN(l) | Positive | Negative |
| ADENO CA(l 1) | Negative | Positive |
Table 12: Mucin expression in prostatic lesions.
Immunohistochemistry with P63-basal cell marker
Routinely p63, stains the basal cell nuclei of the normal prostatic glands. Positive expression of the p63 by the benign lesions indicates the presence of basal cell layer. Negative staining indicates the absence of basal cell layer in the malignant glands.
In this study, patients with S.PSA value >14ng/ml (20cases) were selected for p63 immunostaining and its expression was noted. Out of 20 cases, 9 cases showed p63 positivity and 11 cases showed p63 negativity (Table 13).
| HPE (no.of cases) | p63 Expression | |
|---|---|---|
| Positive | Negative | |
| BNH(8) | 8 | 0 |
| LGPIN(l) | 1 | 0 |
| ADENO CA(l 1) | 0 | 11 |
| Total(20) | 9 | 11 |
Table 13: p63 expression in prostatic lesions.
Hisotpatholoigal findings are shown in Figures 1 to Figure 21.
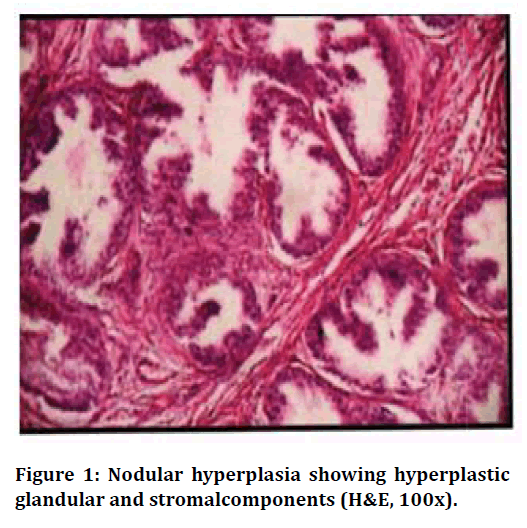
Figure 1. Nodular hyperplasia showing hyperplastic glandular and stromalcomponents (H&E, 100x).
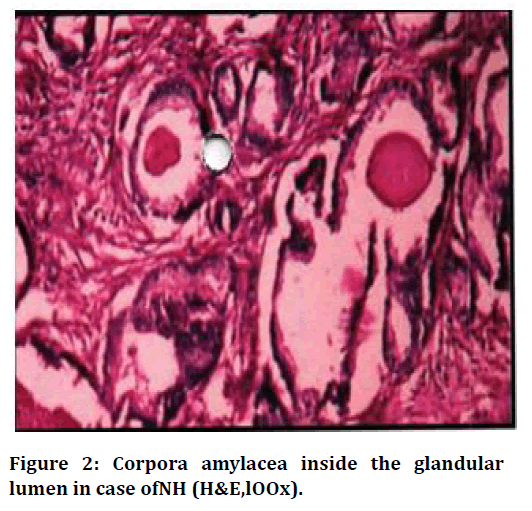
Figure 2. Corpora amylacea inside the glandular lumen in case ofNH (H&E,lOOx).
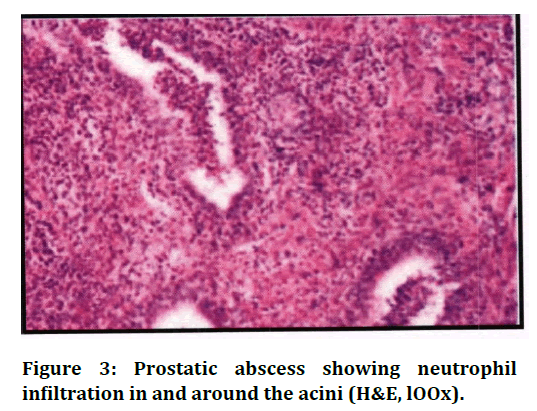
Figure 3. Prostatic abscess showing neutrophil infiltration in and around the acini (H&E, lOOx).
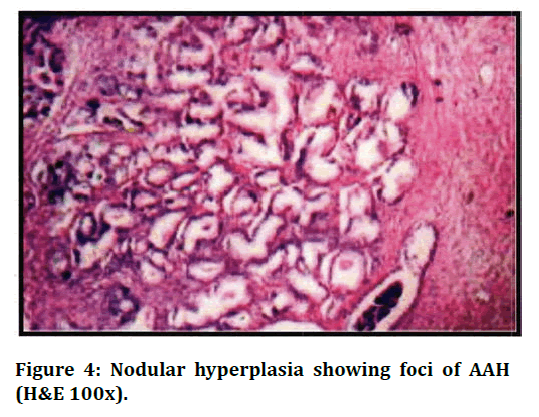
Figure 4. Nodular hyperplasia showing foci of AAH (H&E 100x).
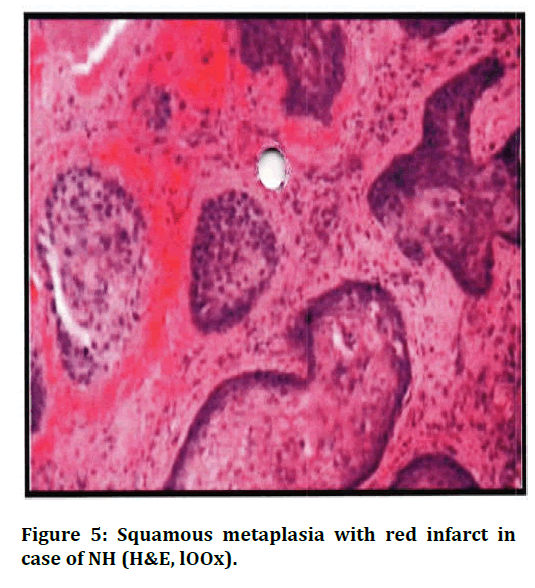
Figure 5. Squamous metaplasia with red infarct in case of NH (H&E, lOOx).
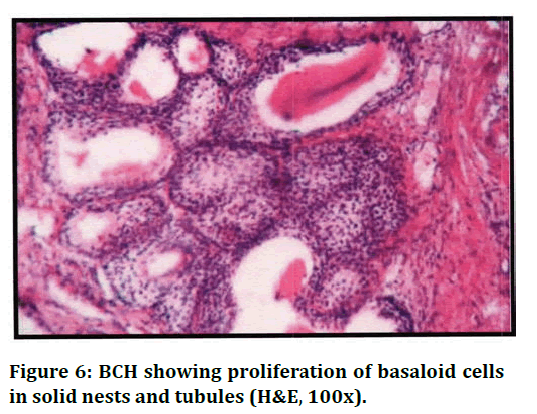
Figure 6. BCH showing proliferation of basaloid cells in solid nests and tubules (H&E, 100x).
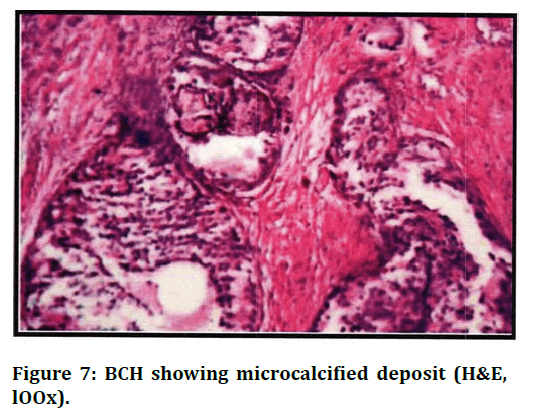
Figure 7. BCH showing microcalcified deposit (H&E, lOOx).
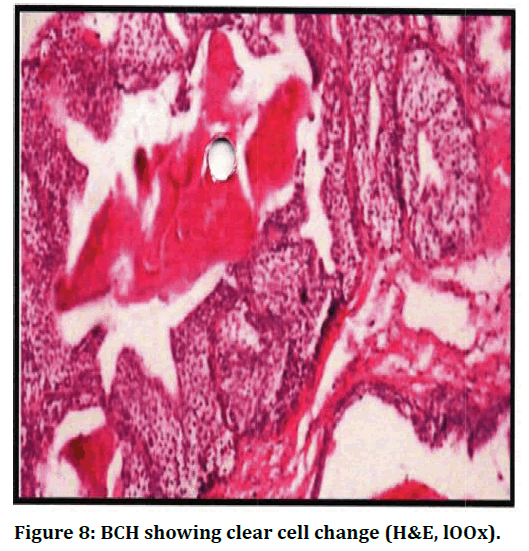
Figure 8. BCH showing clear cell change (H&E, lOOx).
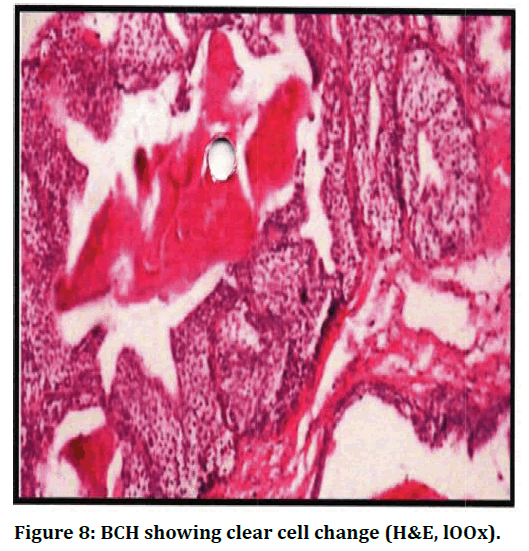
Figure 9. Non specific granulomatous prostatitis showing granulomas causing destruction of the acini (H&E, lOOx).
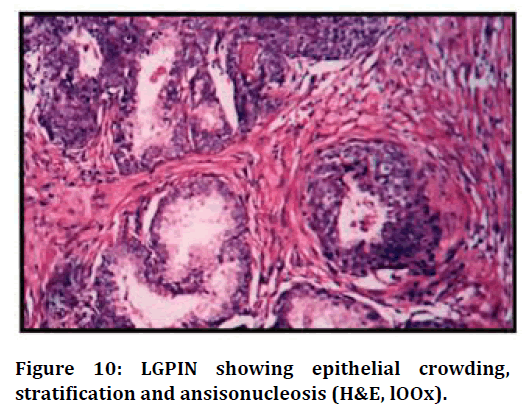
Figure 10. LGPIN showing epithelial crowding, stratification and ansisonucleosis (H&E, lOOx).
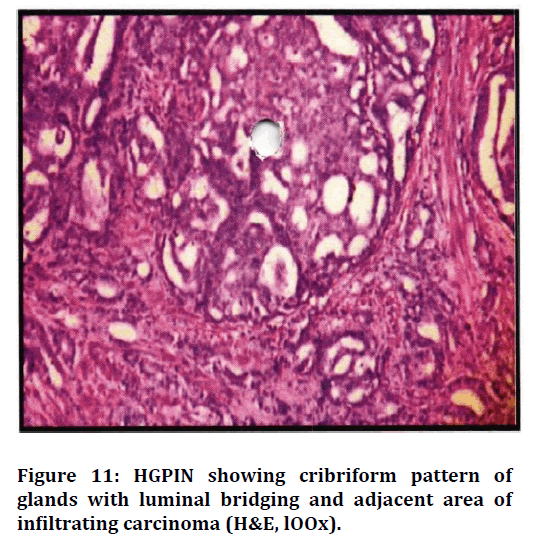
Figure 11. HGPIN showing cribriform pattern of glands with luminal bridging and adjacent area of infiltrating carcinoma (H&E, lOOx).
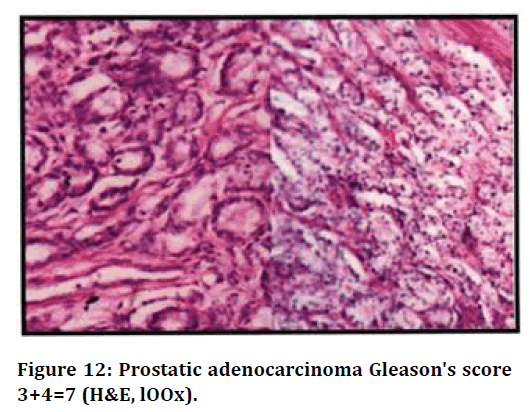
Figure 12. Prostatic adenocarcinoma Gleason's score 3+4=7 (H&E, lOOx).
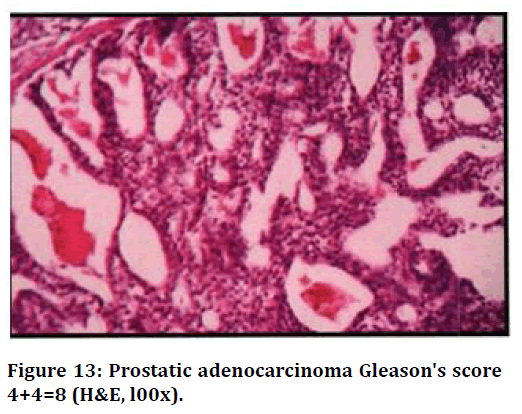
Figure 13. Prostatic adenocarcinoma Gleason's score 4+4=8 (H&E, l00x).
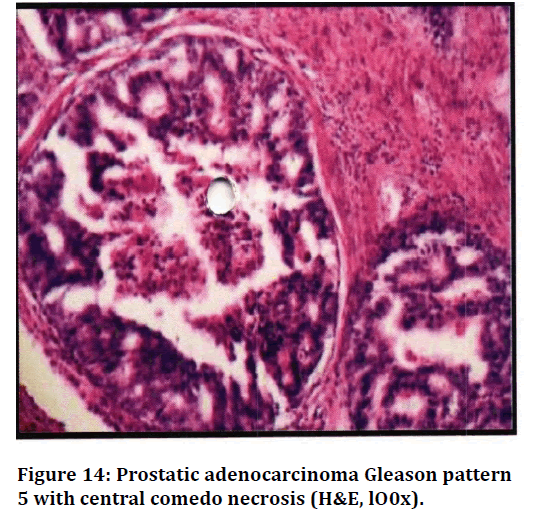
Figure 14. Prostatic adenocarcinoma Gleason pattern 5 with central comedo necrosis (H&E, lO0x).
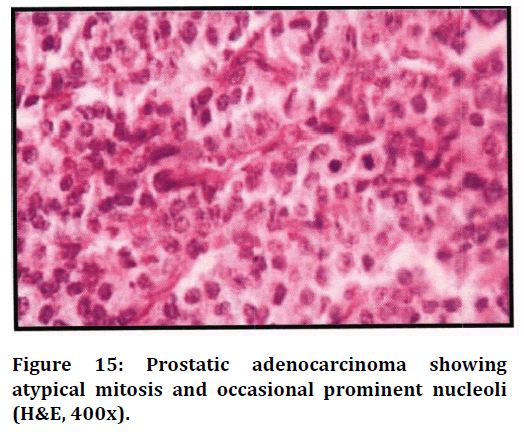
Figure 15. Prostatic adenocarcinoma showing atypical mitosis and occasional prominent nucleoli (H&E, 400x).
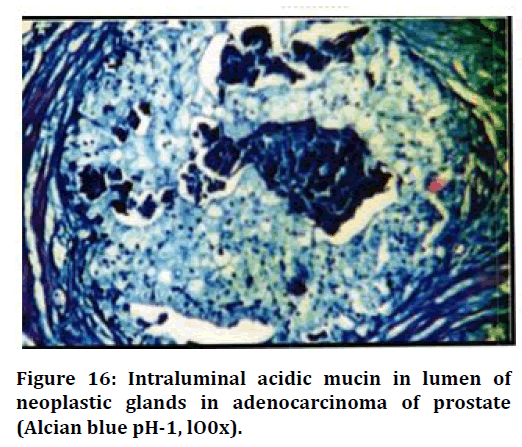
Figure 16. Intraluminal acidic mucin in lumen of neoplastic glands in adenocarcinoma of prostate (Alcian blue pH-1, lO0x).
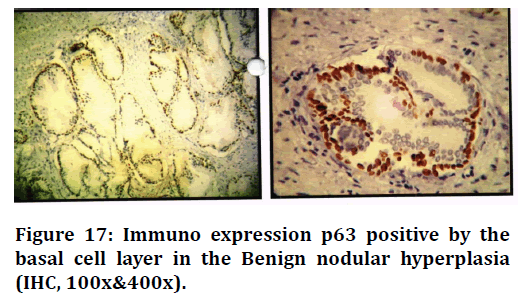
Figure 17. Immuno expression p63 positive by the basal cell layer in the Benign nodular hyperplasia (IHC, 100x&400x).
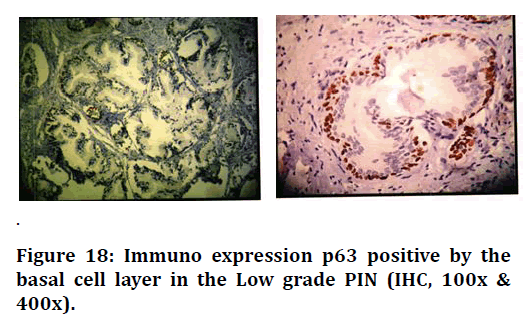
Figure 18. Immuno expression p63 positive by the basal cell layer in the Low grade PIN (IHC, 100x & 400x).
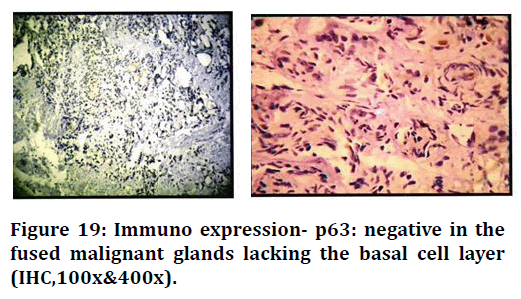
Figure 19. Immuno expression- p63: negative in the fused malignant glands lacking the basal cell layer (IHC,100x&400x).
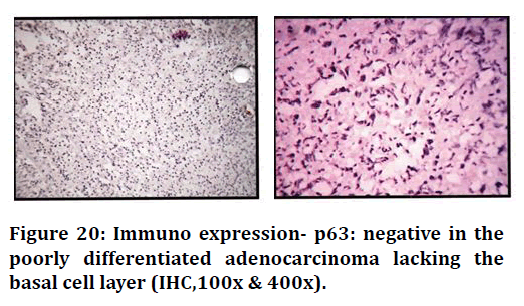
Figure 20. Immuno expression- p63: negative in the poorly differentiated adenocarcinoma lacking the basal cell layer (IHC,100x & 400x).
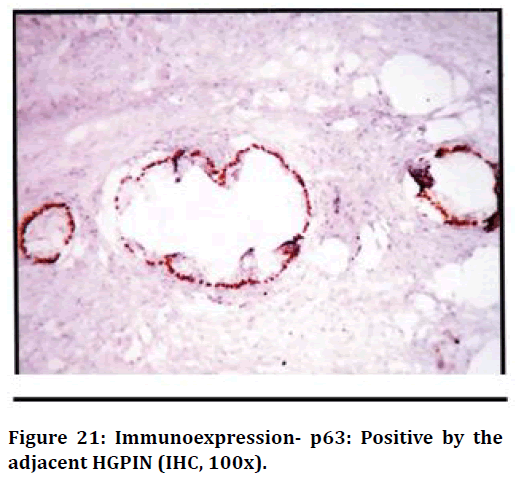
Figure 21. Immunoexpression- p63: Positive by the adjacent HGPIN (IHC, 100x).
Discussion
Prostatism is a common malady in the geriatric age group. Benign nodular hyperplasia and Carcinoma of the prostate are increasingly frequent with advancing age and are uncommon before the age of forty years. A careful examination of the prostate in unselected autopsies disclosed nodular hyperplasia. In approximately 20% of the men in 40 yrs of age, a figure that increases to 70% by age 60 and to 90% by eighth decade of life [8].In India the incidence of benign prostatic hyperplasia is estimated to be 92.97% [7].
Carcinoma of the prostate Is the most common malignant tumor in men over the age of 65 years. In patients with clinically detected nodules, raised PSA, needle biopsy/ trucut needle biopsy is an established tool to confirm the diagnosis. It is currently estimated that in United States of America approximately 241,740 (29%) new cases are detected every year, of which approximately one fifth prove to be lethal [9]. In India the incidence of carcinoma of prostate is estimated at 8/100,000 persons [4].
Incidence of prostatic disorders
The incidence of prostatic disorders increases with increasing age in male population. Mittal et al(l 989) in their study compns1ng of 185 biopsies, reported BNH in 172 (92.97%) cases and carcinoma prostate in 13(7.02%) cases [10]. Novis et al (1999) in their study of 15,753 prostatic biopsies reported highest incidence for benign lesions (55.5%) followed by carcinoma (33.4%) [11]. In the study by Mohammed and Alhasan (2003) they reported 235(77.6%) cases of BNH and 68(22.4%) cases of carcinoma pros tate [12]. Cavalcanti et al (2005) in their series of 142 prostatic biopsies reported BNH in 61 (42. 9%) patients and carcinoma prostate in 31(21.8%) cases. There were 19 cases of atypical small acinar proliferation and 31 cases of prostatic intraepithelial neoplasia [13]. Lokuhetty et al (2008) in their study compns1ng of 749 prostatic biopsies, noted an incidence of 60.6% for benign prostatic lesions and 35.2 % for malignant neoplasms [14]. In the present study comprising of 106 prostatic biopsies, there were 94(88.67%) cases of BNH and 11 (10.4%) cases of carcinoma prostate, 1case (0.94%)of prostatic intraepithelial neoplasia.
Benign nodular hyperplasia was the most commonly encountered lesion followed by carcinoma of the prostate and is similar to that of present study. The incidence of prostatic disorders in the present study, 88.67% for BNH cases and 10.4% for carcinoma prostate cases , was similar to that of the study by Mittal, Amin, 1989 [10] which estimated the incidence of BNH as 92.97% and carcinoma of prostate as 7.02%. In the present study, the incidence of benign lesions was 88.67%. NH alone was noted in 62.26% of total cases, the remaining 26.41% benign cases were composed of NH along with other lesions like prostatitis, basal cell hyperplasia, atypical hyperplasia and metaplasia. The lesions showed hyperplasia of both epithelial and stromal components. In this study, BNH lesions were more common in seventh decade of life presented with chief complaints of difficulty in micturition and increased frequency of micturition. The decline in the number of cases beyond the age of 80 years may reflect the average life span of people in our country.
In the present study, 4 cases (3.77%) were NH along with basal cell hyperplasia characterised by small uniform darkly staining basal cell forming solid nests, tubules and cords with peripheral palisading appearance. 2 cases showed clear cell change in BCH and calcified deposit was seen in 1 case. The present study showed only one case of squamous metaplasia (0.94%) associated with red infarct in addition to NH. However, study by Mittal et al showed metaplastic epithelium in 10.27% of cases.
Prostatitis
In the present study, out of 106 cases, 20 cases had prostatitis. In cases of chronic non- specific prostatitis, lymphocytes, plasma cells and macrophages were seen. Bostwick [15] in his study has reported more cases of chronic abacterial as compared to bacterial prostatitis In this study only one case of prostatic abscess was present but in a study by Granados et al, [16] cases of prostatic abscess were present characterised by sheets of neutrophils in and around the acini [17].
In the present study 2 cases (1. 89%) of non-specific granulomatous prostatitis were noted, out of which one of the case showed well formed epitheloid granulomas with giant cell. There was no evidence of caseation. Mittal et al, showed granulomatous lesi in 1.6% of his cases [10].
Atypical adenoma tous hyperplasia
Yang et al study reported the incidence of Atypical Adenomatous Hyperplasia ranged from 2.2% to 19.6% in the TURP specimen [18]. In the present study, AAH was seen in 3 cases (1.50%). These lesions seen in TURP specimens, were small, multifocal and associated with NH. All these cases were in the age group of 68- 74 years.
Prost atic intra epithelial neoplasia
In the present study, 2 cases showed Prostatic Intra Epithelial Neoplasia. 1 case was LGPIN and another 1 case showed HGPIN associated with prostatic ca rcinoma. LGPIN was characterized by epithelial crowding, stratification but no prominent nucleoli was observed. HGPIN was characterised by pronounced epithelial crowding, nuclear enlargement, hyperchromasia and luminal bridging giving a cribriform appearance. Prominent nucleoli were also seen adjacent area showed small glands infiltrating the stroma.
In our study, PIN was seen in the age group of 6l – 70 years. In the study by McNeal and Bostwick frequency of PIN was highest in the age group 60 - 69yrs [19]. Brawer showed, the incidence of PIN was higher in organs with carcinoma than in those without. According to his study, PIN was found in 73% of prostates with carcinoma and 32% of prostates without carcinoma [20]. The incidence of PIN varies considerably in different studies probably because histological diagnosis of LGPIN shows subjective variation and many studies do not report LGPIN [18]. The incidence of HGPIN is relatively low in cases of prostatic carcinoma in our study because all the specimens were TURP which does not have enough material compared to radical prostatectomy specimen studied in other studies [21]. It is also suggested that transition zone might not be associated with HGPIN [20]. Moreover the incidence of isolated HGPIN is uncommon in TURP specimens (prevalence 2.3%) 87 It is common 1n peripheral zone as compared to transition zone [21].
Prostatic carcinoma
In the present study, the prevalence of carcinoma prostate was 10.40%. This is rather low compared to most reported series and there is wide variation in the incidence rate of prostate cancer in different parts of the world. The increased incidence of prostatic carcinoma in industrialized world is partly due to increased number of cases diagnosed by screening and case finding by serum PSA testing [22].
Age incidence of prostatic carcinoma in different studies
In the present study, peak incidence of prostatic carcinoma was seen in age group of 61- 70 years which was similar to many studies. The mean age and median age of patients with malignant neoplasm of prostate are 70.5 and 70 years.
Carcinoma prostate and Gleason’s score
Numerous grading system has been designed for the histopathological grading of prostate cancer. The Gleason grading system named after D.F.Gleason is now the predominant grading system. The prostate biopsy Gleason score correlates with tumor aggressiveness, tumor volume, serum PSA levels, prognosis and influence of the treatment policy. The Gleason score is also often used to determine eligibility of clinical trials including those for watchful waiting [23].
Murthy et al. in their study estimated that majority of carcinoma prostate (46%) had Gleason's score 2-4 ie) well differentiated tumors followed by moderately differentiated tumors (27%) with GS 5- 78. In the study done by Bing et al. there were 46% of carcinoma prostate patients presenting with GS 5-7 and 33.3% with GS 2-489.
Lokuhetty et al. reported 34.8% of carcinoma prostate patients with a GS 8-10 and 1.16% of them presenting with GS 2-4. Majority of the cases (63.5%) presented with GS 5-782.
In the present study 63.63% of carcinoma cases presented with GS 5-7, 36.40% with GS 8-10 and 9.10% with GS 2-4. In the present study majority of the adenocarcinoma of prostate (54.54%) were moderately differentiated with GS 5- 7 followed by poorly differentiated tumors (36.40%) with GS8-10. This was closely similar to that of study by Lokuhetty et al [13] wherein 63.95% of carcinoma patients presented with moderately differentiated GS 5- 7 and 34.88% presented with poorly differentiated tumors GS 8-10.
Serum PSA values
Normal levels of PSA are usually <4ng/ml but they vary according to the age of the patient. PSA levels <4 ng/ml of 60 years or less and levels <6.5 ng/ml in mean age of 60- 80 years are normal. PSA is elevated by any change that destroys the normal architecture of the prostate which allows diffusion of protease into the microvascular circulation [24]. In the present study, only 48 cases had serum PSA levels estimated. It is observed that, not all the cases of surgical resection of the prostate, serum PSA level estimation are requested.
(Out of 48 cases, 36 cases were benign. A total of 20 cases showed modest elevation of PSA levels and 16 cases showed elevation more than 10 ng/ml in benign cases. This is because, these cases of BNH was associated with prostatitis, abscess, infarcts and granulomatous prostatitis.) In the present study, 9 cases of prostatic carcinoma showed PSA levels >20ng/ml, however 2 cases had PSA levels = l 5ng/ml. This is attributed to study in which prostate cancers detected at lower PSA levels are more likely to have a small volume and are of low grade.
Immunohistochemistry with p63
Prostatic lesions on routine staining sometimes cause diagnostic difficulty especially in low volume needle biopsies and in TURP specimens with cautery effect. In such cases p63 renders more consistent staining than 34 E12, thereby differentiating benign from malignant lesions effectively 89. In the present study, all the benign lesions (9) stained positive for p63 but all the malignant cases (11) stained negative for p63 indicating the absence of basal cell layer.
Parson et al (2001 study observed that basal epithelial cells in normal, benign prostatic hyperplasia, and highgrade intraepithelial neoplasia tissue stained intensely for the p63 polypeptide, but the vast majority of adenocarcinoma specimens did not stain [25]. This observation suggested that staining for p63 may have better diagnostic utility 1n differentiating benign prostatic epithelial structures from prostate cancer.
M.H.Weinstein et al (2002) study proved that p63 immunostaining was diagnostically reliable and is sensitive in identifying basal cells in prostatic needle biopsies and TURP specimens. TURP specimens in which cautery artifact can impair the ability to detect high molecular weight cytokeratin, staining for p63 appears superior [26]. The results of p63 staining In prostatic adenocarcinoma in this study supports the results of Signoretti et al (2000), who performed p63 on 130 cases of invasive prostate cancer and found p63 negativity in 126(97%) cases [27].
Ud Din et al. noted that one of the 50 prostatic adenocarcinomas expressed p63 in his study. Negative p63 expression in adenocarcinomas 1n our present study also co- relates with it [28]. Negative p63 express10n of the malignant lesions in the present study correlates with Signoretti et al, Parson et al, Ud in et al. studies [25,27,28].
Conclusion
It is concluded from the present study that Use of immunohistochemical marker p63 along with racemase marker helps to differentiate the benign from malignant prostatic lesions in diagnostically challenging cases effectively.
Funding
No funding sources.Ethical Approval
The study was approved by the Institutional Ethics Committee.Conflicts of Interest
The authors declare no conflict of interest.
Acknowledegements
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.References
- Bruchovsky N,Goldenberg SL, Gleave M. Intermittent therapy for prostate cancer. End Related Cancer,1997; 4:153-77.
- Kumar VL, Majumder PK. Prostate gland: Structure, functions and regulations. Int Urol Nephrol 1997; 27:221-43.
- AUA practice guideline committee: AUA guideline on management of benign prostatic hyperplasia 2010. Guidelines at a glance for urologists 2011.
- Bid HK, Konwar R, Singh V. Benign prostatic hyperplasia. Is it a growing public health concern for India? Indian J Med Sci 2008; 62:373-4.
- Robbins and cotran pathologic basis of disease. 8th Edn 2010; 996-1002.
- Parkin DM, Bray F. Global cancer statistics 2002. CA Cancer J Clin 2005; 55:74-108.
- Manna AK, Pathak S, Gu-yen P, et al. Study of immunohistochemistry in prostafic lesions with special reference to proliferation and invasiveness. Indian J Surg 2011; 73:101-6.
- Yang A, Kaghad M, Wang Y, et al. p63, a p53 homolog at 3q27-29, encodes multipleproducts with transactivating, death-inducing, anddominant-negative activities. Mol Cell l 998; 2:305-316.
- Rebecca Siegel , Deepa Naishadham, Ahmedin Jamal. Cancer statistics 2012. Cancer J Clin 2012; 62:10-29.
- Mittal BV, Amin MB, Kinare SG. Spectrum of histological lesions 1n 185 consecutive prostatic specimens. J Postgrad Med 1989; 35:157-161.
- Novis D, Zarbo R, Valenstein P. Diagnostic uncertainity in needle biopsies. Arch Pathol Lab Med 1999; 123:687-91.
- Mohammed AZ , Alhassan SU , Edino ST, et al. Histopathological review of prostatic diseases in Kano, Nigeria. Niger Postgrad Med J 2003; 10:1-5.
- Cavalcanti FB, Alves VA, Pereira J, et al. Proliferative lesions of prostate: A multivariate approach to differential diagnosis. Pathol Oncol Res 2005; 11:104-07.
- Lokuhetty MD , Wijsinghe HD, Abeysuriya DT, et al. Transrectal ultrasound guided prostate biopsies: a single centre experience in Srilanka. Ceylon Med J 2009; 54:6-9.
- Bostwick DG, Amin MB. Male reproductive system. In: Damjanov, Linder J. Anderson's pathology. 1996; 1:2197- 2222.
- Stillwell JT, Engen ED, Farrow MG. The clinical spectrum of prostatitis granulomatous: Report of 200 cases. J Urol 1987; 138320- 323.
- Granados AE, Riley G, Salvador J, et al. Prostatic abscess diagnosis and treatment. J Urol 1992; 140:80-82.
- Epstein IJ, Yang JX. Prostatic intraepithelial neoplasia and its mimickers. In Prostate biopsy interpretation. 3rd Edn. Philadelphia: Lippincott W & W 2002; l1-l8.
- McNeal EJ, Bostwick GD. Intraductal dysplasia-A premalignant lesion of the prostate. Hum Pathol 1986; 17:64-71.
- Brawer KM. Prostatic intraepithelial neoplasia: A premalignant lesion. Hum Pathol 1992; 23:242-248.
- McNeal EJ. Morphogenesis of prostatic carcinoma. Cancer 1965; 18:1659-1666.
- Reiter ER, Dekernion BJ. Epidemiology, etiology, and prevention of prostate cancer. In: Walsh, Retik, Vaughan, et al. Campbell's urology. 8th Edn. Philadelphia: WB Saunder's, 2002; 3003-3024.
- Gleason DF. The veteran's administration cooperative urologic research group : Histologic grading and clinical staging of prostatic carcinoma. In Tannenbaum M (ed) Urologic pathology: The prostate, lea and febiger, Philadelphia 1977; 171-198.
- Murthy PD, Ray U, Morewaya J, et al. A study of thecorrelation of prostatic pathology and serum prostate-specific antigen(PSA) levels: A prospective from papua new Guinea. Med J 1998; 41:59-64.
- Parsons JK, Gage WR, Nelson WG, et al. Expression of p63 in normal, neoplastic and preneoplastic human prostate tissues. Urology 2001; 58:619-624.
- Weinstein MH, Signoretti S, Loda M. Diagnostic utility of immunohistochemical staining for p63, a sensitive marker of prostatic basal cells. Modern Pathol 2002; 15:1302-8.
- Signoretti S, Waltregny D, Dilks J, et al. p63 is a prostate basal cell marker and is required forprostate development. Am J Pathol 2000; 157:1769-75.
- Ud Din N, Qureshi A, Mansoor S. Utility of p63 immunohistochemical stSn in differentiating urothelial carcinomas from adenocarcinomas of prostate. Indian J Pathol Microbiol 2011; 54:59-62.
Author Info
Department of Pathology, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Ranjitham, Bheemarao, Histopathological and Immunohistochemical Study of the Prostatic Lesions, J Res Med Dent Sci, 2021, 9(6): 403-413
Received: 08-May-2021 Accepted: 23-Jun-2021
