Research - (2022) Volume 10, Issue 9
HYBRID LESION: A DIAGNOSTIC CHALLENGE
Saraswathi Gopal K, NagammaiN* and Mahesh Kumar P
*Correspondence: NagammaiN, Department of Oral Medicine and Radiology, Faculty of Dentistry Meenakshi Ammal Dental college and H, Meenakshi Academy of Higher Education and Research Institute, Meenakshi Ammal Dental College, India, Email:
Abstract
Hybrid lesions are lesions consisting of association of features of different pathologies. An uncommon association between simple bone cyst and fibro-osseous lesions has been reported in the literature. Here we report a rare case of solitary bone cyst associated with fibrous dysplasia (FD). Thus, the purpose of this paper is not only to present a rare case of hybrid lesion with but also to emphasize on the need of careful clinical, radiological and histopathological examination. This will decrease the incidence of misdiagnosis for such cases and will help in preventing recurrences.
Keywords
Hybrid lesion, Fibrous dysplasia, Solitary bone cyst
Introduction
The benign fibro-osseous lesions (BFOLS) of the jaws comprise a diverse, interesting and challenging group of conditions that pose difficulties in classification and treatment. Benign fibro-osseous lesions such as Fibrous dysplasia are considered as bone developmental anomaly characterized by hamartomata’s proliferation of fibrous tissue within the medullary cavity [1]. The normal medullary bone and cortices are replaced by a disorganized fibrous woven bone. Fibrous dysplasia occurs unilaterally, diagnosed in the second decade of life and is relatively common in maxilla. Females are less affected than males, with variable radiographic appearances and the lesion never cross the midline [2].
Solitary bone cyst (SBC) is also called as Traumatic Bone Cyst, Hemorrhagic Cyst, idiopathic bone cavity and also as pseudo cyst as it lacks epithelial lining. It is very rare and occurs of about 1% of all jaw cysts [3]. It is asymptomatic bone lesion affecting mainly children and young adults. Usually, routinely discovered in X-rays performed for other purposes.
An unusual association between SBC and fibroosseous lesions, including cemento-osseous dysplasia (COD), fibrous dysplasia(FD), ossifying fibroma (OF) and osteoblastoma [4]. Although theories have been proposed to explain this association is mainly due to disorderly bone production in fibrous dysplasia might result in obstruction of interstitial fluid drainage, leading to cyst formation. Always SBC occurs secondarily to fibrous bone diseases [5,6]. Lesions with features from various pathologies have been reported in the literature. These are called “hybrid lesions [7]. The purpose of this paper is to report a case of FD associated with SBC and to discuss the clinical, imaging and histopathological features of this hybrid lesion.
Case Report
A 23-year-old female patient reported to the department with the chief complaints of swelling in the left lower third of the face for the past five years. Presenting illness reveals development of swelling first, which is of the same size from the time of inception for the past 5 years. No history of pain, paraesthesia, discharge or any other constitutional symptoms associated with it. Past dental history reveals H/o consulting a dentist for the same before 5years for which she was diagnosed with dental caries and also performed extraction and curettage. After treatment also there was no reduction in the size of the swelling noted. Medical history was non-contributory and Review of system reveals no abnormalities detected.
On extra-oral examination presence of a diffuse swelling evident on the left side of inferior border of mandible in the region of 35,36,37 measuring 2 cm X 1 cm in its greatest dimension (Figure 1). It extends anteriorly from parasymphysis region to posteriorly 1.5cm in front of the left angle of mandible. Superiorly 3cm below the ala tragus line and inferiorly 0.5cm below the inferior border of mandible. Swelling was non-tender and hard to palpating fingers. On intra-oral examination reveals missing 36 with evidence of mild buccal cortical plate expansion in 36 and 37 regions which is non-tender and bony hard on palpation (Figure 2). Tooth pertaining to the region were vital and periodontally sound. Thus correlating the history and past dental treatment provisional diagnosis was given as Residual cyst in 36 regions.

Figure 1. Diffuse swelling evident on the left side of inferior border of mandible in the region of 35, 36, 3.
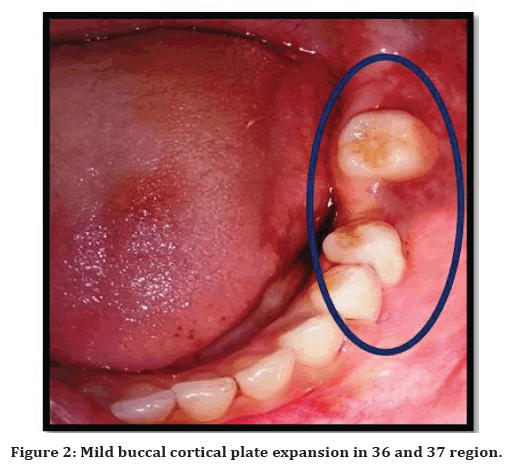
Figure 2. Mild buccal cortical plate expansion in 36 and 37 region.
The orhtopantography reveals complete loss of tooth structure evident in 36. Evidence of altered trabecular pattern in the mandibular left molar region with displacement of inferior alveolar nerve more superiorly and also with extensive resorption and downward bowing at the inferior border of mandible with thin intact cortex maintained (Figure 3). CBCT reveals presence of ill-defined mixed hypo dense and hyper dense area in the region of 35, 36, 37 which measures 1.3cm X 3.2cm X 1.6cm (AP X SI X MB) in its greatest dimension. Ground glass appearance of the trabercular pattern with bicortical plate expansion with a thin intact cortex still maintained. Superior lift of inferior alveolar nerve in the region of 35, 36, 37 observed (Figure 4). Hence the radiological diagnosis was made as Fibrous dysplasia in the left lower third of the mandible. Routine blood investigations along with serum examination for alkaline phosphatase activity and calcium profile were performed and the values were within normal limits and then the patient was subjected for histopathological examination. Histopathological examination revealed empty cancellous bone cavity that is present without a epithelial lining and with presence of a thin connective tissue layer features suggestive of solitary bone cyst.
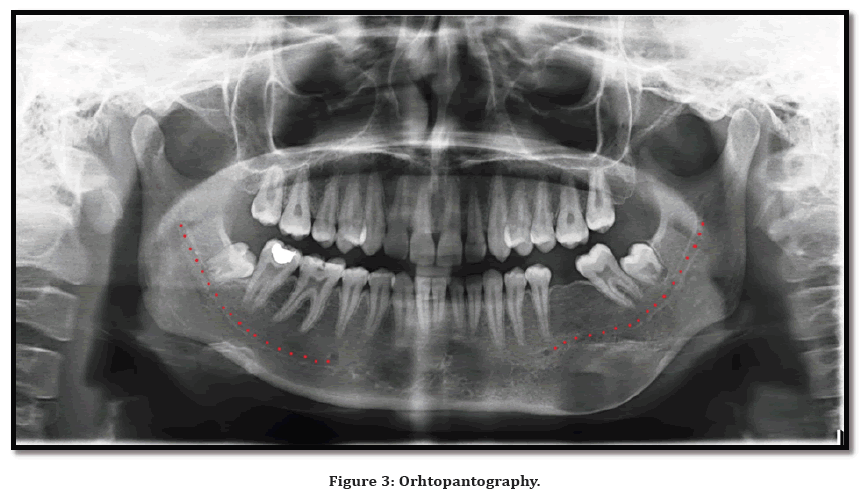
Figure 3. Orhtopantography.
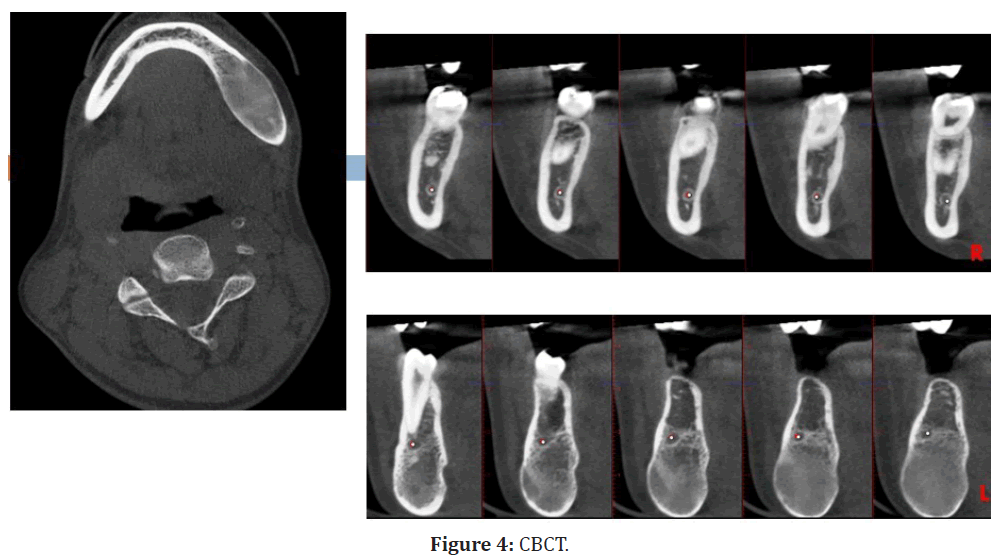
Figure 4. CBCT.
Thus the final diagnosis was made with correlating the past dental history, present clinical features, radiological features and histopathological features as Hybrid lesion fibrous dysplasia with coexisting solitary bone cyst in the left lower third of the mandible. Bony recountouring was done as a treatment protocol and patient is under regular follow-up.
Discussion
The term BFOLS, in and of itself, is not meant to be a specific diagnosis 8. Fibro-osseous lesions are a heterogeneous group of entities consisting of a variably cellular, fibro vascular stroma along with varying amounts of mineralized material consistent with either bone or cementum. Differential diagnosis among fibro-osseous lesions can be difficult, as these lesions don’t present a well-defined behavior [8,9]. Thus with adequate clinical, radiological and histopathological information is needed for the identification. Our case has two kinds of different lesions fibrous dysplasia and solitary bone cyst.
Fibrous dysplasia is also called fibrocystic disease, focal osteitis fibrosa, fibro osteodystrophy, and Jaffe- Lichtenstein. First described by Lichtenstein in 1938 and by Lichtenstein and Jaffe in 1942 .It is considered as hamartomatous disorder of bone metabolism which can cause facial disfigurement of the face due to its occurrence in the period of bone growth and development. It is a hereditary, non-acquired infection occurs due to transformation of the Gs alpha subunit of protein coupled receptor leading about up direction of cAMP that prompts to abandons activation of osteoblasts with stimulating creation of irregular bone in a prominent connective tissue stroma [10]. It is caused replacement of normal bone by an excessive proliferation of cellular fibrous connective tissue intermixed with irregular bony trabeculae [11]. It represents approximately 7% of all benign osseous tumors and may affect any bone of the skeleton [12]. Fibrous dysplasia can display in one bone (monostotic) or numerous bones (polyostotic) and can be connected with other condition, for example, café-aulait skin spots, as well as endocrine disorders (precocious puberty, renal phosphate wasting, hyperthyroidism, and additionally development hormone abundance. Females are more commonly affected than males. The monostotic form is more common and affects people at 20–30 years of age, whereas the polyostotic form has its onset mainly in children younger than 10 years of age. Monosotic form begins as asymptomatic painless swelling in the affected area leading to facial asymmetry with the maxilla being more commonly affected than the mandible. With the mandible involved, it may safely be called monoostotic FD, however, when the maxilla is involved, it may be more apt to call it craniofacial FD.
Syndrome association
Multiple bone involvement with café-au-lait pigmentation Jaffe Lichtenstein syndrome.
PFD associated with café aula it pigmentation and endocrinopathy including hyperthyroidism, sexual dysfunction is recognized as McCune Albright syndrome.
Mazabraud’s syndrome is one such syndrome where FD is associated with multiple soft tissue myxomas.
Radiology features
Intraoral radiography and panoramic radiographs are the most commonly used first line imaging, although computed tomography gives images which are most representative of the lesion [13-15]. The pagetoid appearance is the most common, whereas the sclerotic form is commonly called as the ground glass appearance, and the cyst-like form is a rare variant. Borders of FD are contiguous with normal adjacent bone. Displacement of teeth and resorption of roots is rare. Unqiue features are present when it is seen on maxilla such as expand into the antrum by displacing its cortical boundary in the original contour of the antral wall and this marks a differentiating feature from other neoplasm [16]. It behaves peculiarly in the mandible because it displaces the inferior alveolar canal superiorly. Histopathological the trabeculae present as a curvilinear shaped giving a Chinese script pattern [17].
Solitary bone cyst
Usually aetiology of the traumatic bone cyst is unknown though many theories were based on Traumahaemorrhage theory. Theory states that clot breaks down and leaves an empty cavity within the bone. Steady expansion of cyst may occur only to secondary obstruction of lymphatic or venous drainage. Expansion tends to cease when lesion reaches the cortical layer of bone. Most frequently occur in young persons with over 75 % of cases occur in the second decade of life. Posterior portion of the mandible is more commonly involved. Pulps of the teeth in the involved area are vital. When the cavity is opened surgically, it is found to contain either a small amount of serosanguinous fluid, shreds of necrotic blood clot, fragments of fibrous connective tissue or nothing. Radiologically presence of smoothly outlined radiolucent area with a thin sclerotic border and mostly involve the molar area of the body of the mandible. Histopathological reveals a thin connective tissue membrane lining the cavity.
Association of between fibro-osseous lesions and SBC
First described by Melrose et al. [18]. Reason for formation of SBC related to fibrous bone diseases might be associated with osteocyte death provoked by lack of cellular nutrition. Fischer19 reported that fibro-osseous tissue precedes SBC. Hybrid lesions are rare and so diagnosing will be very challenging. Thus much literature is needed for us to understand the interrelationship between lesions better.
Conclusion
The association of fibrous dysplasia and solitary bone cyst is very rare and thus only very few cases are reported in the literature. The association of this lesion is mainly due to Ischaemia that provokes the apoptosis of osteocytes and lead to formation of cavity in the medullary portion of the bone. There is an important need to report such similar or other such similar cases in literature and so the diagnosis and treatment will be more precise and so there is no reoccurrence seen.
References
- Jawanda MK, Narula R, Shankari M, et al. Hybrid lesions comprising central giant cell granuloma and fibrous dysplasia: A diagnostic challenge for pathologist. J Oral Maxillofac Pathol 2015; 19:408.
- Neville BW, Damm DD, Allen CM, et al. Oral and maxillofacial pathology. 2nd Edn. Philadelphia, PA: WB Saunders Company; 2003.
- Rajendran R. Shafer's textbook of oral pathology. Elsevier India 2009.
- Saito Y, Hoshina Y, Nagamine T, et al. Simple bone cyst. A clinical and his¬topathologic study of fifteen cases. Oral Surg Oral Med Oral Pathol 1992; 74:487-491
- Wakasa T, Kawai N, Aiga H, et al. Management of florid cemento-osseous dysplasia of the mandible producing solitary bone cyst: Report of a case. J Oral Maxillofac Surg 2002; 60:832-835.
- Fisher AD. Bone cavities in fibro-osseous lesions. Br J Oral Surg 1979; 14:120-127.
- Crusoé-Rebello I, Torres MG, Burgos V, et al. Hybrid lesion: Central giant cell granuloma and benign fibro-osseous lesion. Dentomaxillofac Radiol 2009; 38:421-425.
- Waldron CA, Giansanti JS. Benign fibro-osseous lesions of the jaws: A clinical-radiologic-histologic review of sixty-five cases. Oral Surg Oral Med Oral Pathol 1973; 35:190–201.
- Singer SR, Mupparapu M, Rinaggio J. Clinical and radiographic features of chronic monostotic fibrous dysplasia of the mandible. J Can Dent Assoc 2004; 70:548–552.
- Ashrafi SK, Asim KY, Suhail Z. Fibrous dysplasia of mandible. J Coll Physicians Surg Pak 2012; 22:728.
- Mahajan S, Kamboj M, Baoz K. Maxillofacial fibrous dysplasia. Indian J Dent Res 2005; 16:151.
- Ham DW, Pitman KT, Lassen LF. Fibrous dysplasia of the clivus and sphenoid sinus. Military Med 1998; 163:186-189.
- Kumar Srichinthu K, Ragunathan Yoithapprabhunath T, Chitturi RT, et al. Fibro osseous lesions–classifications, pathophysiology and importance of radiology: A short review. Int Biol Biomed J 2016; 2:11-20.
- Shapeero LG, Vanel D, Ackerman LV, et al. Aggressive fibrous dysplasia of the maxillary sinus. Skeletal Radiol 1993; 22:563.
- Obisesan AA, Lagundoye SB, Daramola JO, et al. The radiologic features of fibrous dysplasia of the craniofacial bones. Oral Surg Oral Med Oral Pathol 1977; 44:949-959.
- Wood NK, Goaz PW. Solitary radiolucencies with ragged and poorly defined borders. In: Wood NK, Goaz PW. Differential diagnosis of oral and maxillofacial lesions. St. Louis: Mosby 1997; 363.
- Rajendran R. Shafer's textbook of oral pathology. Elsevier India 2009.
- Melrose RJ, Abrams AM, Mills BG. Florid osseous dysplasia. A clinical-pathologic study of thirty-four cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1976; 41:62-82.
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Author Info
Saraswathi Gopal K, NagammaiN* and Mahesh Kumar P
Department of Oral Medicine and Radiology, Faculty of Dentistry Meenakshi Ammal Dental college and H, Meenakshi Academy of Higher Education and Research Institute, Meenakshi Ammal Dental College, Chennai, Tamil Nadu, IndiaReceived: 09-Aug-2022, Manuscript No. jrmds-22-74247; , Pre QC No. jrmds-22-74247(PQ); Editor assigned: 11-Aug-2022, Pre QC No. jrmds-22-74247(PQ); Reviewed: 26-Aug-2022, QC No. jrmds-22-74247(Q); Revised: 31-Aug-2022, Manuscript No. jrmds-22-74247(R); Published: 07-Sep-2022
