Research - (2021) Volume 9, Issue 6
Hyperbilirubinemia as a New Diagnostic Marker for Acute Appendicitis and its Role as a Predictor of Complicated Appendicitis: A Prospective Study
Shaik Khader Basha, RG Santhaseelan and PK Baskaran*
*Correspondence: PK Baskaran, Department of General Surgery, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
Aim: The present study was done to assess the relationship between hyperbilirubinemia and acute appendicitis and to evaluate its credibility as a diagnostic marker for acute appendicitis and its predictive potential in diagnosis of complicated appendicitis. Methodology: This one-year cross sectional study was conducted in the department of general surgery, Sree Balaji Medical College and Hospital during the period of April 2018 to April 2019. A total of 100 patients with clinical diagnosis acute appendicitis or complicated appendicitis were studied. The serum bilirubin and liver function tests were carried out in all the patients. Results: In this study, male (58%) outnumbered females (42%) and overall, the mean age was 29. The mean total serum bilirubin of all 100 patients was 1.491±1.0319 mg/dl which was above the normal range (>1.0 mg.dl) considered for the study, hence indicating the presence of hyperbilirubinemia. The mean of direct bilirubin was 1.290±0.7483mg/dl while that of indirect bilirubin was 0.504±0.2494 mg/dl. Among the patients with inflamed appendix, 26 patients (34.66%) were found to have elevated bilirubin (>1.0mg/dl). In patients diagnosed with appendicular perforation (n=25), 19 patients (76%) had bilirubin elevated (>1.0mg/dl), while only 6 patient (24%) had normal level (<1.0 mg/dl). Thus, hyperbilirubinemia was seen in 34.66% of patients with acute appendicitis and 76% of patients with complicated appendicitis. Sensitivity and specificity of bilirubin in diagnosing acute appendicitis and appendiceal perforation was 76% and 65.33% respectively. Similarly positive predictive value and negative predictive value of bilirubin was 42.22% and 89.09%. Conclusion: Serum bilirubin routinely added to the blood investigation can be useful laboratory investigation for aiding in the diagnosis of acute appendicitis. Can be easily done and cheaply available. Patients with three times the normal bilirubin value and clinical signs of appendicitis and appendicular perforation have higher probability of having complicated appendicitis.
Keywords
Acute appendicitis, Appendicular perforation, Hyperbilirubinemia, Bilirubin
Introduction
Acute appendicitis is one of the most common case presenting as a surgical emergency [1,2]. Appendicitis has been evolving through ages depicting its importance of early diagnosis and appropriate management. The diagnosis of appendicitis is more of a clinical even with latest advances in the diagnostic modalities. Misdiagnosis of appendicitis is 15.3% even in the hands of an experienced surgeon [3]. There are 36 negative appendicectomies done globally to prevent one case of appendicitis per se as per main got. And it can be potentially life threatening to the patient if the diagnosis is late or delayed leading to perforation, peritonitis, abscess, sepsis. Hence appendicitis should be diagnosed early and negative appendicectomies have to be avoided to prevent unnecessary surgical morbidity. surgical exploration can lead to anaesthetic complications, future hernias can develop because of abdominal wall muscle weakness, it also causes post- operative adhesion and in pregnant women it can lead to fetal loss and lastly an abdominal scar.
Even well experienced surgeons make their diagnosis based on history, clinical Examination and findings, and laboratory investigations which are only 80% positive [4]. As ultrasonography and CT is unavailable in the rural areas and with an intention to reduce negative appendicectomies and delay in diagnosis of complicated appendicitis, there arises a gap for available diagnostic markers. Even Though Alvarado scoring, WBC count and CRP are used as laboratory markers. Recent studies on rise in bilirubin value suggest high specificity and comparable sensitivity than former it can be easily done laboratory marker [5,6].
Acute Appendicitis is mostly polymicrobial in nature, causes bacterial translocation into the gut. There bacteria in turn releases endotoxins and stimulates production of pro inflammatory cytokines like TNF and IL1. These molecules reach the liver via portal venous system leading to hepatocyte dysfunction and prevent the release of bilirubin and produces cholestatic type of jaundice. Based on these observation, present study was done to empathize the predictive value of hyperbilirubinemia in appendicitis and potential to detect complicated appendicitis [7-9].
Materials and Methods
The current study was performed in the department of general surgery at Sree Balaji Medical College Hospital during the period of April 2018 to April 2019.
Place of study
The present study was conducted in the department of surgery, Sree Balaji medical college hospital, Chromepet, Chennai.
Source of data
Patients admitted with clinical diagnosis and planned for emergency surgery under the department of general surgery, Sree Balaji Medical College and Hospital during the study period.
Sample size
A total of 100 patients with pre-operative clinical diagnosis of appendicular pathology were included.
Selection criteria
Inclusion criteria
All patients clinically diagnosed as acute appendicitis and gangrenous appendicitis which were taken up for emergency surgery in surgical department. In both the group histopathological report were considered.
Exclusion criteria
Prior history of jaundice, Prior history of liver disease, Prior history of pancreatitis, Chronic alcoholism, Patients with hepatitis B, A and C and Taking drugs increasing liver parameters like rifampicin.
Procedure
The study was conducted after obtaining ethical committee clearance of Sree Balaji Medical College and hospital, Chromepet, Chennai. Based on the criteria patient admitted and underwent emergency appendicectomy for acute and complicated appendicitis in Sree Balaji Medical College and hospital were included. All eligible patients were informed about the purpose and usefulness of study. Then after obtaining informed consent as per consent form submitted in annexure.
All relevant clinical finding and history recorded in predesigned Patient proforma submitted in annexure. All patients clinically diagnosed as acute and complicated appendicitis were submitted to battery of blood investigation, then emergency appendicectomy and histopathological report attached.
Statistical analysis
The collected data were analysed with IBM.SPSS statistics software 23.0 Version. To describe about the data descriptive statistics frequency analysis, percentage analysis were used for categorical variables and the mean & S.D were used for continuous variables. To find the significant difference between the bivariate samples in independent groups the Unpaired sample t-test was used. To assess the efficacy of the tools the Sensitivity, Specificity, PPV and NPV was used. To find the significance in categorical data Chi-Square test was used similarly if the expected cell frequency is less than 5 in 2×2 tables then the Fisher's Exact was used. In all the above statistical tools the probability value .05 is considered as significant level.
Results
In our study conducted on “hyperbilirubinemia as a new diagnostic marker for acute appendicitis and its role as a predictor of complicated appendicitis: a prospective study” conducted from April 2018 to April 2019 at Sree Balaji Medical College and Hospital, Chromepet, Chennai. 100 cases of acute appendicitis undergoing emergency appendectomy were included in our study. Patients included in our study were resuscitated adequately before taken up for study. Patient’s details were collected and documented using the standard proforma. The details and values were compiled into a master chart and following observations were made (Table 1 to Table 10) and (Figure 1 to Figure 7).
Table 1: Sex distribution.
| Sex distribution | ||
|---|---|---|
| Frequency | Percent | |
| Female | 42 | 42 |
| Male | 58 | 58 |
| Total | 100 | 100 |
Table 2: Descriptive statistics of age.
| Descriptive statistics of age | |||||
|---|---|---|---|---|---|
| N | Minimum | Maximum | Mean | SD | |
| Female | 42 | 17 | 45 | 29 | 7.752 |
| Male | 58 | 16 | 64 | 29 | 11.3814 |
| Total | 100 | 16 | 64 | 29 | 9.9747 |
Table 3: Ultrasonogram finding.
| Ultrasound | ||
|---|---|---|
| Frequency | Percent | |
| Complicated appendicitis | 25 | 25 |
| Inflamed appendix | 59 | 59 |
| Normal appendix | 16 | 16 |
| Total | 100 | 100 |
Table 4: Total bilirubin levels.
| Total Bilirubin | ||
|---|---|---|
| Frequency | Percent | |
| >1 mg/dl | 45 | 45 |
| <=1 mg/dl | 55 | 55 |
| Total | 100 | 100 |
Table 5: Descriptive statistics of LFTS.
| Descriptive Statistics | N | Minimum | Maximum | Mean | S. D |
|---|---|---|---|---|---|
| Total bilirubin | 100 | 0.4 | 4.5 | 1.491 | 1.0319 |
| Direct Bil | 100 | 0.4 | 3.6 | 1.29 | 0.7483 |
| Indirect Bil | 100 | 0.1 | 1.1 | 0.504 | 0.2494 |
| SGOT | 100 | 10 | 53 | 27.08 | 9.6804 |
| SGPT | 100 | 11 | 47 | 26.87 | 9.1537 |
| ALP | 100 | 33 | 141 | 97.16 | 23.4373 |
Table 6: Total leucocyte count.
| Total count | ||
|---|---|---|
| Frequency | Percent | |
| < 10000 | 29 | 29 |
| >= 10000 | 71 | 71 |
| Total | 100 | 100 |
Table 7: Descriptive statistics of differential leucocyte count.
| Descriptive statistics | |||||
|---|---|---|---|---|---|
| N | Minimum | Maximum | Mean | S.D | |
| Total count | 100 | 6800 | 18700 | 11784 | 2718.798 |
| Neutrophils | 100 | 54 | 91 | 73.26 | 8.8929 |
| Lymphocytes | 100 | 8 | 44 | 21.89 | 7.8159 |
| Monocytes | 100 | 0 | 11 | 3.99 | 2.8832 |
| Eosinophils | 100 | 0 | 5 | 1.06 | 1.1443 |
Table 8: Comparison of mean serum bilirubin levels in patients with acute appendicitis (Inflamed) and appendicular perforation/ gangrene (Complicated).
| Comparison with Unpaired t-test | ||||||
|---|---|---|---|---|---|---|
| Groups | N | Mean | S. D | t- value | P-value | |
| Total bilirubin | Complicated | 25 | 2.74 | 1.24 | 9.705 | 0.0005** |
| Inflamed | 75 | 1.08 | 0.48 | |||
| Direct BIL | Complicated | 25 | 2.04 | 1.01 | 4.836 | 0.0005** |
| Inflamed | 75 | 1.04 | 0.41 | |||
| Indirect BIL | Complicated | 25 | 0.7 | 0.3 | 4.021 | 0.0005** |
| Inflamed | 75 | 0.44 | 0.19 | |||
**Highly Significant at P<0.01 level |
||||||
Table 9: ROC curve.
| Groups | Valid N (listwise) |
|---|---|
| Positivea | 25 |
| Negative | 75 |
Table 10: Area under the curve.
| Area under the curve | |||
|---|---|---|---|
| Area | P-value | 95% C.I | |
| LB | UB | ||
| 0.707 | 0.002** | 0.59 | 0.823 |
**Highly Significant at P<0.01 |
|||
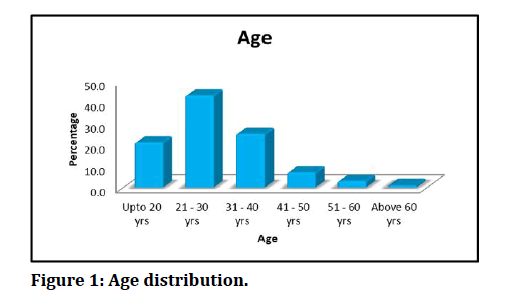
Figure 1: Age distribution.
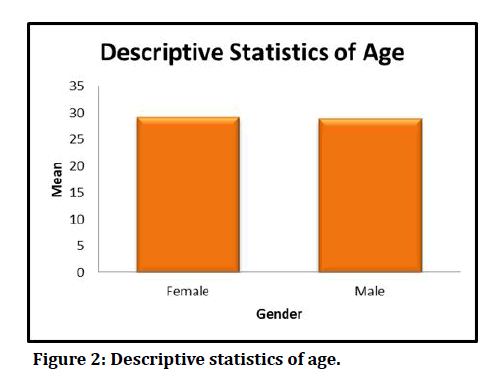
Figure 2: Descriptive statistics of age.
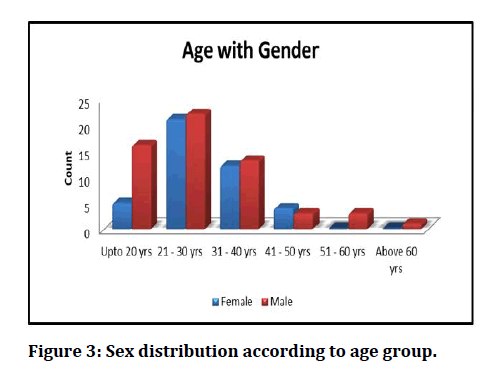
Figure 3: Sex distribution according to age group.
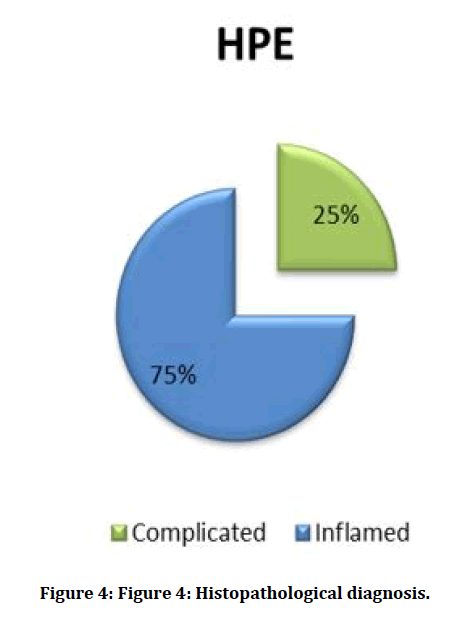
Figure 4: Histopathological diagnosis.
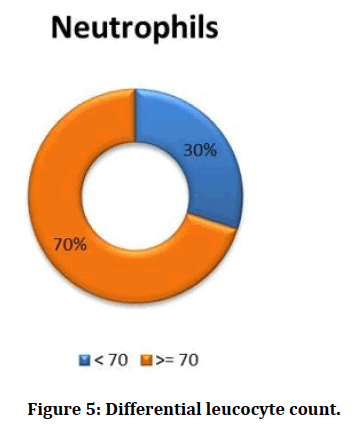
Figure 5: Differential leucocyte count.
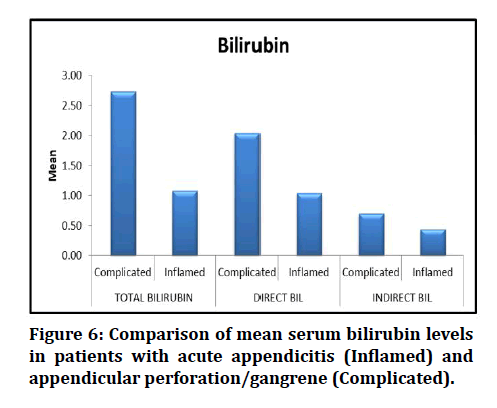
Figure 6: Comparison of mean serum bilirubin levels in patients with acute appendicitis (Inflamed) and appendicular perforation/gangrene (Complicated).
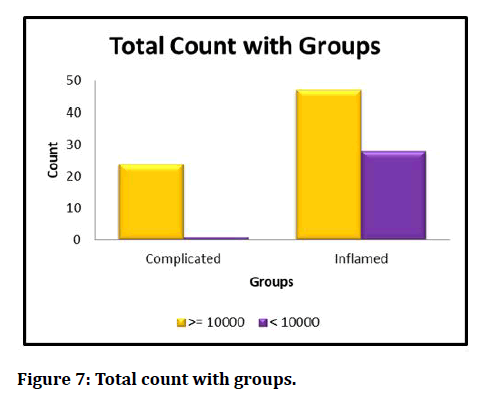
Figure 7: Total count with groups.
Most of the patients in our study was found to be in young, aged adults aged between 21 to 30 age group. 43 % of patients are from this age group. Mean age of presentation was 29 years (Table 1). The overall mean of all 100 patients in the study was 29 years with SD of 9.9747. The mean and standard deviation in males were 29 and 11.3814. The mean and standard deviation in females were 29 and 7.7520 (Table 2 and Figure 2).
The mean total bilirubin levels in patients diagnosed as inflamed appendicitis was 1.08 ± 0.48, in patients with complicated appendicitis was 2.74±1.24. The direct and indirect bilirubin levels in patients with inflamed appendicitis was 1.04±0.41 and 0.44 ± 0.19, respectively. The direct and indirect bilirubin levels in patients with complicated appendicitis was 2.04±1.01and 0.70 ± 0.30 respectively (Table 8 and Figure 6).
Discussion
Acute appendicitis remains the most common acute surgical condition of the abdomen, it is also most misdiagnosed condition. Appendectomy is the most performed emergency procedure for acute appendicitis in the world. The lifetime risk of developing acute appendicitis is 8%for the people in western countries. The highest incidence of acute appendicitis is in the 2nd and 3rd decade of life. It occurs commonly in childhood and early adult life, rarely in infancy. It occurs equally among males and females before puberty. Male to female ratio increases to 3:2 by age of 25 in young adults [10]. The lifetime rate of appendectomy is 12% for males and 25% for females, about 7% of all people undergoing appendectomy for acute appendicitis during their lifetime. Majority of appendicitis is believed to be caused by appendicular luminal obstruction. Fecolith is the usual cause of this luminal obstruction. Less common causes include hypertrophy of the lymphoid tissue, intestinal parasites, and tumours. appendix contains bacterial flora normally like that present in normal large intestine. Escherichia coli and Bacteroides fragilis are the most common organisms observed in normal appendix, acute appendicitis, perforated appendicitis, and gangrenous appendicitis [11,12].
However, a broad variety of both anaerobic and facultative bacteria may be present. Acute appendicitis is diagnosed mainly by the clinical examination. It is often difficult to diagnose as classical signs and symptoms suggesting acute appendicitis may not be present in all patients. Different presenting symptoms and clinical signs mimic the diagnosis of acute appendicitis, especially in women. The decision to operate on clinical suspicion alone can lead to removal of normal appendix, it happens in 15 -50% of cases. Precise diagnosis can be made by additional tests and expectant management or both. The above delay in diagnosis may lead to perforation or gangrene of the appendix leading to increased morbidity. Safe alternative is to do appendectomy as soon as the condition is suspected, but this strategy leads to unnecessary appendectomy [13].
There is still ongoing debate regarding the optimal management of acute appendicitis with several studies proposing conservative and nonoperative management. To achieve an accurate and early diagnosis many additional tests, scoring systems, imaging modalities like ultrasonography, CT, MRI is done and laparoscopy can be employed. None of the above tests alone will diagnose acute appendicitis, these tests are always inferior to clinical examination and signs unless combined. [14].
Hyperbilirubinemia is a new diagnostic marker for perforated and gangrenous appendicitis which is postulated recently. These results due to an imbalance in synthesis and excretion of bilirubin by the liver. This study has been designed to verify the association of hyperbilirubinemia in cases acute appendicitis and its complications. This study is a single centre cross sectional, observational study conducted in the department of general surgery, Sree Balaji Medical College and Hospital, Chromepet, Chennai over a period of one year from April 2018 to April 2019 on 100 patients admitted for acute appendicitis and underwent emergency appendectomy. In our study of 100 patients, 58 patients (58%) were males while remaining 42 patients (42%) were females. This observation was like other studies. [15]. The 71 patients, 37 (52.10%) were male and 34 (47.90%) were female’ [16-19]. Stated in his study that ‘Of 50, 40 cases were male and 10 females’ Most of the patients in our study was found to be in young adults aged between 21 to 30 yrs age group. 43 % of patients are from this age group. Mean age of presentation was 29 years. The mean and standard deviation in males were 29 and 11.3814. The mean and standard deviation in females were 29 and 7.7520, respectively. The mean age of distribution in our study population corresponds to other studies [20] stated that ‘The average was 27.1 years.
Mean age -26.93±9.33’. ‘Out of the 964 patients included in study, the mean age reported was 28.7 years’ Our studies have shown that appendicitis is more common in males and in younger age groups. Majority of female patients were from age group 21 to 30 years. After the age of 30 years the ratio decreases with equal or greater incidence in females. This is also supported by the below journal [21,22] where he states ‘The disease is slightly more common in males, with a male: female ratio of 1.4:1, In teenagers and young adults, the male–female ratio increases to 3:2 at age 25; thereafter, the greater incidence in males’ declines. In Our study we observed that out of 100 patients 55 of them had normal total bilirubin value of < 1.0mg/dL (55%) while hyperbilirubinemia was found in 45 patients (45%). This corresponds to the below studies conducted [23] found that ‘Of the 71 patients, total serum bilirubin was elevated in 41 (57.70%) of them’, observed that ‘Among 50 cases, total SB (TSB) was raised in 38 (76%) cases whereas 12 (24%) cases had normal TSB level’ [24] had found hyperbilirubinemia in 59 (38%) of 157 patients studied with acute appendicitis. The mean total serum bilirubin of all 100 patients was 1.491 ±1.0319 mg/dL, which is minimally above normal range (≤1.0 mg/dL).
The mean in inflamed (uncomplicated) appendicitis was 1.08±0.48. The mean in perforated or gangrenous appendicitis (complicated) was 2.74±1.24 which is well above the normal range, indicating hyperbilirubinemia. The direct bilirubin and indirect bilirubin in patients diagnosed with acute appendicitis were 1.04±0.0.41mg/dl and 0.44±0.1941mg/dl respectively. Similarly, direct bilirubin and indirect bilirubin in patients diagnosed with complicated appendicitis were 2.04±1.01mg/dL and 0.70±0.30 mg/dL respectively. The total serum bilirubin was significantly elevated in gangrenous or perforated appendix than those in acute appendicitis (P<0.001). This was consistent with the studies done [25,26] who found average level of serum bilirubin in his study population to be 2.38 mg/dL. found a mean of 3.62mg/dL in his study population of complicated appendicitis. All patients were found to have SGOT and SGPT within normal limits, thus fulfilling our exclusion criteria. The mean SGOT and SGPT were 27.080± 9.6804 U/L and 26.870±9.1537U/L. The mean ALP values were 97.160±23.4373/L.
In our study all patients underwent ultrasonography imaging, 59(59%) patients were diagnosed as acute appendicitis, and 25 (25%) patients were diagnosed as having perforated or gangrenous appendix and 16 (16%) patients with normal appendix. Ultrasound was highly sensitive for detecting complicated appendicitis. We observed in our study that total leucocyte count was elevated in 71% of all the patients diagnosed as appendicitis. The mean TLC count of all patients was 11784±2718/mm3, in which majority of cells are neutrophils73.260 ±8.8929 % followed by lymphocytes 21.890±7.8159 %. These were consistent with other study like [27,28] stated in study ‘Of the 71 patients Total leukocyte count was found to be elevated in 33 (46.5%) patients. Regarding mean TLC stated that ‘Mean WBC was 16.4 × 103/μL (SD, ±5.2; 3.1 to 32.0 ×103/μL) for all patients. Mean WBCs in the simple and complicated groups were elevated respectively, with significantly higher levels in the complicated group’.
Among the patients diagnosed with uncomplicated acute appendicitis (n=75), 49 patients (65.33%) were having normal total serum bilirubin levels (≤1.0mg/dL), 26patients (34.66%) had elevated total serum bilirubin levels. In patients with perforated or gangrenous appendicitis (n=25), only 6(24%) patients had total serum bilirubin within normal limits, rest of 19(76%) patients had elevated total serum bilirubin levels. Hence hyperbilirubinemia is found in most of the patients with perforated or gangrenous appendicitis (76%). The sensitivity, specificity, positive predictive value, negative predictive value was calculated for the total serum bilirubin as a test for predicting gangrenous or perforated appendix using 2×2 table. The sensitivity and specificity of serum bilirubin as a marker in predicting perforated or gangrenous appendicitis was 76% and 65.33% respectively. Similarly, the negative predictive value and positive predictive value for the test is 89.09% and 42.22% respectively. ROC curve was drawn, area under the curve (AUC) was 0.707. Our study revealed that there is isolated increase in total serum bilirubin level without significant elevation in liver enzymes, is a significant predictor of perforated or gangrenous appendix (p<0.001). Our study showed total serum bilirubin to have low specificity of 65.33% and high sensitivity of 76.00%. The negative predictive value was 89.09% comparable towhich showed 100% [29] where there was three times the risk of having perforated or gangrenous appendix in patients with hyperbilirubinemia (>1.0mg/dL) [30] showed that hyperbilirubinemia had a specificity of 86% for appendiceal perforation or gangrene. Hence in patients suspicious of perforation or gangrene elevation of serum bilirubin can be used as a test to diagnose and manage perforated or gangrenous appendicitis.
Conclusion
Total serum bilirubin was significantly elevated in patients with complicated (gangrenous or perforated) appendicitis than those with acute appendicitis. Total serum bilirubin level as a test for predicting complicated (gangrenous or perforated) appendicitis is an overly sensitive, less specific with a high negative predictive value. Hence it is a valuable indicator in patients likely to have complicated (gangrenous or perforated) appendicitis. Total serum bilirubin should be used along with clinical examination and other laboratory investigations in the assessment of patients suspected of appendicitis.
Funding
No funding sources.Ethical Approval
The study was approved by the Institutional Ethics Committee.Conflict of Interest
The authors declare no conflict of interest.Acknowledgements
The encouragement and support from Bharath University, Chennai, is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.References
- O’Connel PR. The vermiform appendix. In: Russel RCG, Williams NS, Bulstrode CJK Editors. Bailey &Love ‘s Short practice of surgery. 24th Edn London: Arnold; 2004; 1210.
- Harold E, Nathanson LK. Appendix and appendicectomy. In: Zinner MJ, Schwartz SI. Harold E. Editors. Maingot’s abdominal operation 10th Edn. 1997; 2:1202.
- Deutsch AA, Shani N, Reiss R. Are some some appendectomies unnecessary? An analysis of 319 white appendices. J Royal College Surg Edinburgh 1983; 28:35-40.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3950177/
- Vesalius A. De humani corporis fabrica liber v basel, Switzerland: Johanes Oporinu 1543.
- Fitz RH. Perforating inflammation of the vermiform appendix with special reference to its early diagnosis and treatment. Am J Med Sci 1886; 321.
- D’Alia C, Lo Schiavo MG, Tonante A, et al. Amayand ‘s hernia: Case report and review of the literature. Hernia 2003; 7:89-91.
- McBurney C. The incision made in the abdominal wall in cases of appendicitis, with a description of a new method of operating. Ann Surg 1894; 20:38-43.
- Meade RH. An Introduction to the History of General Surgery. Philadelphia, PA: Saunders; 1968.
- Korner H, Sondenaa K, Soreide JA, et al. Incidence of nonperforated and perforated appendicitis: age-specific and sexspecific analysis. World J Surg 1997; 21:313-317.
- https://accessmedicine.mhmedical.com/content.aspx?bookid=2576§ionid=216215350
- Puylaert JB. Imaging and intervention in patients with acute right lower quadrant disease. Baillieres Clin Gastroenterol 1995; 9:37-51.
- Delic J, Savkovic A, Isakovic E. Variations in the position and point of origin of vermiform appendix. Med Arch 2002; 56:5-8.
- Fawcett DW, Raviola E. Bloom and fawcett: A textbook of histology Chapman and Hall: New york NY 1994; 636.
- Bluett MK, Halter SA, Salhnany KE , et al. Duplication of the appendix mimicking adenocarcinoma of the colon. Arch Surg 1987; 817-20.
- Jones BA, Demetriades DE, Segal IS, et al. The prevalence of appendiceal fecaliths in patients with and without appendicitis. A comparative study from Canada and South Africa. Annals Surg 1985; 202:80.
- https://www.elsevier.com/books/robbins-and-cotran-pathologic-basis-of-disease/kumar/978-1-4557-2613-4
- Vermulen B, Morabia A, Unger PP. Influence of white cell count on surgical decision making in patients with abdominal pain in the right lower quadrant. Eur J Surg 1995; 161:483-6.
- Gronroos M, Gronroos P. Leucocyte and c reactive protein in the diagnosis of acute appendicitis. BJS 1999; 86:501-504.
- Gurleyik E, Gurleyik G, Unalmiser S. Accuracy of serum C-reactive protein measurements in diagnosis of acute appendicitis compared with surgeon's clinical impression. Diseases Colon Rectum 1995; 38:1270-4.
- Green RM, Beier D, Goltan JL. Regulation of hepatocyte bile salt transporters by endotoxin and inflammatory cytokines in rodents. Gastroenterology 1976; 111:193-8.
- Atahan K, Üreyen O, Aslan E, et al. Preoperative diagnostic role of hyperbilirubinaemia as a marker of appendix perforation. J Int Med Res 2011; 39:609-18.
- Sand M, Bechara FG, Holland-Letz T, et al. Diagnostic value of hyperbilirubinemia as a predictive factor for appendiceal perforation in acute appendicitis. Am J Surg 2009; 198:193-8.
- Estrada JJ, Petrosyan M, Barnhart J, et al. Hyperbilirubinemia in appendicitis: A new predictor of perforation. J Gastro Surg 2007; 11:714-8.
- Jamaluddin M, Hussain SM, Ahmad H. Hyperbilirubinaemia a predictive factor for complicated acute appendicitis: A study in a tertiary care hospital. J Pak Med Assoc 2013; 63:1374-8.
- Chaudhary P, Kumar A, Saxena N, et al. Hyperbilirubinemia as a predictor of gangrenous/perforated appendicitis: A prospective study. Annals of gastroenterology: Quarterly Publication of the Hellenic Society of Gastroenterology 2013; 26:325.
- Addiss DG, Shaffer N, Fowler BS, et al. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990; 132:910.
- Estrada JJ, Petrosyan M, Krumenacker J, et al. Hyperbilirubinemia in appendicitis: A new predicator of perforation. J Gastrointestinal Surg 2007; 11:714–5.
- Khan S. Evaluation of hyperbilirubinemia in acute inflammation of appendix: A prospective study of 45 cases. KUMJ 2006; 15:281- 9.
- Sand M, Bechara FG, Holland-Letz T, et al. Diagnostic value of hyperbilirubinemia as a predictive factor for appendiceal perforation in acute appendicitis. Am J Surg 2009; 198:193-198.
Author Info
Shaik Khader Basha, RG Santhaseelan and PK Baskaran*
Department of General Surgery, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Shaik Khader Basha, RG Santhaseelan, PK Baskaran, Hyperbilirubinemia as a New Diagnostic Marker for Acute Appendicitis and its Role as a Predictor of Complicated Appendicitis: A Prospective Study, J Res Med Dent Sci, 2021, 9(6): 219-227
Received: 01-Apr-2021 Accepted: 18-Jun-2021
