Case Report - (2022) Volume 10, Issue 12
HYPOMAGNESEMIA CAUSING POSTERIOR REVERSIBLE ENCEPHALOPATHY SYNDROME
Pon Divya Bharathi*, Manimekalai Periyasamy and Vinatha MC
*Correspondence: Dr. Pon Divya Bharathi, Department of General Medicine, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, India, Email:
Abstract
Various unspecific neurological complications can be caused by hypomagnesaemia, it can challenge the diagnosis. Posterior Reversible Encephalopathy Syndrome (PRES) is one of these complications, which is exceedingly rare and in English language literature, it was only mentioned twice. Case presentation, we're reporting a case report involving a 60 years old male, presented with PRES, correlated with hypomagnesaemia affecting only the cerebellar hemispheres. Following the exclusion of all the possibilities, we began magnesium replacement therapy with other potential etiologies of PRES, led to an important yet fluctuating clinical development and chemical enhancement. Following dis continuation of proton pump inhibitors, a complete recovery with no requirement for more supplementation was achieved. Conclusion, the work of magnesium in the pathophysiology of posterior reversible encephalopathy syndrome is highlighted. In each PRES case with unknown etiology, underlying hypomagnesaemia should be considered.
Keywords
Hypomagnesaemia, Encephalopathy, Vitamin D, Magnesium, Pathophysiology
Introduction
The 2nd most dominant intracellular action, magnesium, following is potassium and 4th extracellular most abundant overall, action. Out of total magnesium, 99% is intracellular processed, primarily in the bone. The muscles are stretched. The plasma magnesium, that accounts for just one percent of total body magnesium, which can be ionized or connected to either anions or protein. In various physiological functions, magnesium plays a crucial role; thus its hemostasis is regulated strictly by absorption in the small intestine and excreted through kidneys. Normally, hypomagnesaemia is identified as having a level of magnesium under 0.66 mmol/l (1.6 mg/dl). An adequate dietary intake is recommended by the German society for nutrition to prevent hypomagnesaemia. Chronic etiologies of hypomagnesaemia include popular etiologies of insufficient food, alcoholism, vomiting and diarrhea. Other mal absorption, steatorrhea, short gut disorders associated with increased GI magnesium loss include mal absorption, pancreatitis and genetic defects involving absorption of magnesium. Hypomagnesaemia, similarly, may be the effect of increased renal wastage of magnesium caused by certain drugs diuretics, inhibitors of EGFR, calcineurin inhibitors, carboplatin, aminoglycoside, cisplatin, pentamidine, rapamycin, antibiotics and amphotericin B and genetic defects such as Bartter's syndrome and gitelman syndrome. Proton pump inhibitors cause hypomagnesaemia, possibly by influencing the absorption of the intestines. Patients with mild deficiency of magnesium can present with signs such as anxiety, exhaustion, muscle spasms and weakness of muscles. Significant complications like heart arrhythmias, epilepsy, neuromuscular irritability, muscular irritability, weakness and respiratory depression can be caused by critically low magnesium levels [1]. Through hypomagnesaemia a broad range of neurological disorders can also result, such as spontaneous nystagmus main down beat with myopathy, ataxia, cerebellar syndrome and the condition of Posterior Reversible Encephalopathy Syndrome (PRES) [2]. Some effects like agitation, depression, cognitive confusion and coma are also reported. In the setting of hypomagnesaemia, we record a case of PRES here and include a literature review on cerebellar symptoms correlated with it.
Case Presentation
A 60-years-old man was admitted with complaints of thoracic discomfort, vertigo, nausea and ataxia. Possibility of acute coronary disease was eliminated. Patient was then referred to us because of worsening of the neurological symptoms during his first week of treatment. He displayed extraordinary limb and trunk ataxia, rest, postural and deliberate tremor, extreme dysarthria, nystagmus and moderate cognitive impairment on clinical review. The patient was unable to walk or eat without help. Acetylsalicylic acid, pantoprazole, atorvastatin, spironolactone, opipramol, ferrosanol and ramipril were included in his existing oral medication. Patient is a known case of hypertension, CAD and gastrointestinal bleeding episode caused in 2016 angio dysplasia and in 2012 he had pulmonary embolism. In furthermore, he had a previous medical history of chronic diarrhea. Without any organic a etiology for the last two years, vitamin D deficiency after replacement and persistent hypokalemia. The patient also gave history of alcohol use, drank two glasses of beer on a regular basis. He was hospitalized six months ago in the neurology department. At that moment, an acquired cranial Magnetic Resonance Imaging (MRI) showed a symmetric in both cerebellar hemispheres, hyper intensity. Exclusion of cerebellar paraneoplasty syndrome and bacterial or viral syndrome. A lumbar puncture, autoimmune encephalitis, was carried out. The outcome of the study of cerebrospinal fluid was the Standard. NMDA receptor antibodies, AMPA1 and AMPA2 receptors and autoantibodies against Ma2 and M2, as well as antibodies to herpes simplex, were not present in the CSF. An empirical treatment of aciclovir and rocephin has been started, but the antiviral treatment was discontinued after excluding herpes simplex in CSF. The BP was marginally raised during surveillance; thus an antihypertensive drug was started counseling. In colonoscopy and gastroscopy only H pylori negative gastritis has been shown. Dysarthria improved well and the patient was then discharged from the hospital with a posterior reversible encephalopathy syndrome diagnosis based on the MRI finding.
The laboratory studies have revealed a very low level of magnesium 0.4 mg/dl; (range: 1.7-2.55 mg/dl), the level of hypocalcaemia 1.7 mmol/l (range: 2.1-2.5 mmol/l). Erum potassium 3.6 mmol/l, a low haemoglobin count 12.3 g/l, RBC value of 3.69 10*6/μl; low vitamin D level of 25 OH 7 ng/ml (range: 31–100 ng/ml), despite replacement therapy. And a normal value of 22.3 pg/ml Parathormone (PTH) level. The phosphate and sodium levels were within the normal range. The level of creatine kinase was high 450 U/l (range: With <174 U/I). The additional laboratory examinations, shows the normal range of electrophoresis. During the course of treatment, mild hypokalemia noted and the oral supplementation has been initiated. The cranial MRI showed poor residual hyper intensity possibly as a residual indicator in the cerebellar bi hemispheric hyper intensity predictor which was defined in the previous MRI. The findings of electroencephalography were regular. In order to exclude we performed a LP for para-neoplastic syndrome, which showed an unremarkable result. Another such potential cause of PRES, such as high blood pressure, has been missing, we believed cerebellar syndrome, due to hypomagnesaemia and the IV initiation of magnesium supplementation and oral intake of calcium was initiated. An intravenous supplementation was obtained by the patient along with oral supplements of calcium and potassium, 1 g of magnesium sulfate hepta hydrate every 2 days. After 2 weeks of supplementation, the magnesium level was with in normal range, as the level of calcium within 4 days. The patient demonstrated a strong clinical change in ataxia; he was able to walk and eat without assistance. After a hospitalization time of 14 days, the patient was discharged. The post stationary magnesium was received by the patient, three days a week, intravenous supplementation for 2 months. In particular, magnesium excreted in the 24 hour urine was normal, except the renal waste of magnesium. Subsequently, discontinued replacement therapy. The patient remained asymptomatic for more than 5 months (Figures 1 and 2).
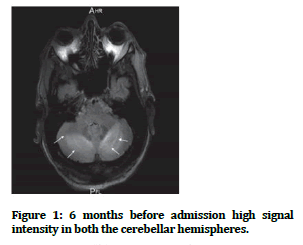
Figure 1: 6 months before admission high signal intensity in both the cerebellar hemispheres.
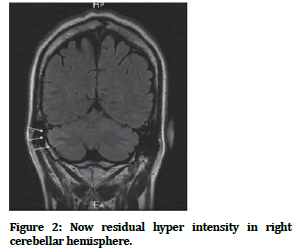
Figure 2: Now residual hyper intensity in right cerebellar hemisphere.
Discussion
PRES because of magnesium depletion is unusual, in only two instances has been identified. MRI studies in the present case revealed that the cerebellar hemispheres are only involved in the PRES representation. Isolated cerebellar participation in the case of PRES is very infrequent [3]. Diverse situations associated with PRES were recognized; this includes fluctuating BP, kidney failure, immunosuppressive treatment, eclampsia and autoimmune diseases [4]. In the case of ours, on admission to the hospital, elevated blood pressure levels were recorded was reduced rapidly without complications. Furthermore, during past hospitalization, only a slightly increase in BP level was reported, although the radiological findings resulted in PRES. Consequently, after eliminating another potential aetiology we suspected hypomagnesaemia, for PRES. In the chemical analysis showed an especially low magnesium concentration of 0.4 mg/dl. And the cause of severe hypomagnesaemia may be due to intake of PPI, chronic diarrhea, regular intake of alcohol, or a mixture of these. For many years, the patient was taking PPI and had chronic diarrhea for 2 years. In addition to that, he used to drink 2 wine glasses/day for several years. Notably, the amount of magnesium in 24 hr urine excluding renal waste was normal. Following discontinuation of PPI use, magnesium levels became normal. A severe hypomagnesaemia, followed by hypocalcaemia, mild hypokalemia were reported in blood tests. Chronic deficiency of vitamin D but a normal level of PTH. Depletion of magnesium can cause renal potassium secretion and reduced calcium levels by impairing or causing resistance to the development of PTH in target organs. PTH was within the usual range in the present case, despite the severe hypocalcaemia suggesting a secondary Hypoparathyroidism as a result of hypomagnesaemia [5]. But in, two cases which have been reported: Hypomagnesaemia and hypocalcaemia, elevated PTH has been associated. The parenteral magnesium replacement therapy has resulted in quick improvement clinically [6]. Before achieving the normal range, the patient will resume his normal daily activities without any assistance. After PPI is substituted with ranitidine, intravenous post stationary magnesium supplementation was completed. In the literature, there are about 10 case reports detailing hypomagnesaemia derived cerebellar syndrome. In four cases, short bowel syndrome caused hypomagnesaemia to develop after an operation. Hypomagnesaemia, especially, same like in our case, in all the cases that are reported, it was neglected and only diagnosed after ruling out such probable triggers in the second or third hospitalization. Acyclovir antiviral therapy was started in both the patients. Irrespective of the regimes for supplementation, clinical improvement was seen in 8/11 cases; and the reoccurrence of symptoms was reported in 3 instances. Hence hypomagnesaemia reflects a treatable cause of PRES and cerebellar syndrome [7,8].
Conclusion
Severe neurological symptoms are caused by hypomagnesaemia; including cerebellar syndrome and posterior reversible encephalopathy syndrome are included. Investigation considering the underlying hypomagnesaemia in these disorders, along with the presence of other conditions and long duration use of PPI is important. The PPI's replacement and intravenous supplementation could overcome the symptoms and avoid expensive unnecessary investigations.
References
- Pasina L, Zanotta D, Puricelli S, et al. Acute neurological symptoms secondary to hypomagnesaemia induced by proton pump inhibitors: A case series. Eur J Clin Pharmacol 2016; 72:641–643.
- Fugate JE, Rabinstein AA. Posterior reversible encephalopathy syndrome: Clinical and radiological manifestations, pathophysiology and outstanding questions. Lancet Neurol 2015; 14:914–925.
- Li D, Lian L, Zhu S. Isolated cerebellar involvement in posterior reversible encephalopathy syndrome. J Neurol Sci 2015; 357:101–105.
- Hamed IA, Lindeman RD. Dysphagia and vertical nystagmus in magnesium deficiency. Ann Intern Med 1978; 89:222-223.
- Coppeto JR, Monteiro ML, Lessell S, et al. Downbeat nystagmus: Long term therapy with moderate dose lithium carbonate. Arch Neurol 1983; 40:754‑755.
- Fischer M, Schmutzhard E. Posterior reversible encephalopathy syndrome. J Neurol 2017; 264:1608–1616.
- Pandita A, Lehmann DF. Magnesium sulfate treatment correlates with improved neurological function in Posterior Reversible Encephalopathy Syndrome (PRES): Report of a case. Neurologist 2018; 23:65–66.
- Hauser SL, Josephson SA. Harrison’s neurology in clinical medicine. McGraw Hill, 4th edition, New York, 2017.
Author Info
Pon Divya Bharathi*, Manimekalai Periyasamy and Vinatha MC
Department of General Medicine, Sree Balaji Medical College and Hospital, Chennai, Tamil Nadu, IndiaCitation: Pon Divya Bharathi, Manimekalai Periyasamy, Vinatha MC, Hypomagnesaemia Causing Posterior Reversible Encephalopathy Syndrome, J Res Med Dent Sci, 2022, 10 (12): 164-166.
Received: 10-Oct-2022, Manuscript No. JRMDS-22-57360; , Pre QC No. JRMDS-22-57360(PQ); Editor assigned: 14-Oct-2022, Pre QC No. JRMDS-22-57360(PQ); Reviewed: 25-Oct-2022, QC No. JRMDS-22-57360; Revised: 13-Dec-2022, Manuscript No. JRMDS-22-57360(R); Published: 20-Dec-2022
