Research - (2021) Volume 9, Issue 11
Hypoparathyroidism the Cause of Seizure, Misdiagnosed as Epilepsy
Kannan Meera Devi*, V Padma, Sathyapriya, Sarath Bhaskar and Saketh Ramineni
*Correspondence: Kannan Meera Devi, Department of General medicine, Sree Balaji Medical College and Hospital, India,
Abstract
A 27 year aged male presented to the emergency with repeated seizures which has been diagnosed as epilepsy before from 14 years of age. The biochemical tests and brain imaging studies were indicative of seizures which occurred due to underlying hypocalcaemia, and an impression of idiopathic hypoparathyroidism was given. Once the replacement of calcium and vitamin D done, the patient get well soon and he is free of seizures, and he is stopped taking anti epileptics. This case mainly shows the presence of brain calcinosis with underlying idiopathic hypoparathyroidism; the cause of acutely presenting seizures due to stimulating factors which are other than epilepsy; and their significance, in these situations, of considering the other curable causes for seizures other than epilepsy.
Keywords
Parathyroid hormone, Seizure, Epilepsy, Hypocalcemia
Introduction
An seizure of adult onset is a condition that is frequently encountered. Patients are mostly diagnosed as with diagnosis of epilepsy and in some patients, proper tests to find precipitating factors and curable causes are not done. This reported case shows such a situation where a patient having hypocalcaemia-causing seizures who was with idiopathic hypoparathyroidism (IH) but was managed for epilepsy long period. We considering the importance of acute symptomatic seizures and there should be a purposeful approach to investigate adults with new presentation of seizures. And also we enlight Hypocalcemia , the main cause of this seizures and in this patient we have discussed the presence of calcinosis of brain in IH and the main part of brain calcinosis condition and hypocalcaemia as the cause of seizures [1-3].
Case Report
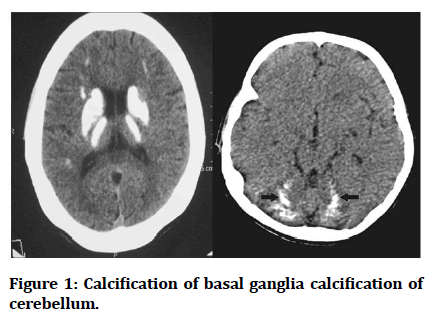
A 27year aged male presented to emergency with repeated seizure episodes which are preceded by history of paraesthesia in oral region and fingertip. As per findings he was considered to be a patient of epilepsy and he did not want to do any further investigations and follow up for the cause of seizures. On the time of examination, signs such as chovsteks and trousseau were present. In lab parameters, serum corrected calcium - 1.02 millimol/L (low), magnesium- 0.73 milli mol/L, phosphate level 2.59 milli mol/L (high), and total 25-OH vitamin D was 55.98 nano mol/L (low). His serum parathyroid hormone 0.7 picomol/L which is low, even vitamin D is insufficient, confirming Idiopathic Hypoparathyroidism. Cerebellum and basal ganglia calcification in seen in CT brain. Intravenous calcium infusion was initially given and on chronic oral calcium supplements with alfa-calcidol to keep calcium level in at least a low normal level. So finally antiepileptic drugs are not given as the cause of seizures are due to long-term hypocalcaemia . After his 4 months of follow-up, he was seizure free (Figure 1).
Figure 1: Calcification of basal ganglia calcification of cerebellum.
Discussion
Seizure is characterized as a "transient occurrence of signs or symptoms due to abnormal brain neuronal activity that is excessive or synchronous. Epilepsy has a history of minimum one seizure which can produce subsequent seizures and related neurobiological, psychological, cognitive and social disorders due to a change in the brain. The description of the cause of seizure has now been widely explored to find the difference among acutely presenting seizure symptoms and seizures that is happening in close relation with CNS acute insult, which may be due to other causes like toxic, structural and seizures which are unprovoked or epileptic conditions where there is no identical estimated for acute symptomatic seizures. And usually any seizures could be investigated for provocative causes that can cause acute symptomatic seizures in adults diagnosed with new onset seizures. Study should start with a detailed clinical assessment at the bedside and more research linked with clinical findings initially such as brain imaging where there is suspicion of ay brain structural lesion. Initial investigation to be CT brain due to cost-effectiveness and accessibility; however, CT can overlook certain anomalies, and if there are still questions about in lesion that is structural, MRI is suggested. There is contradictory data for the study of metabolic disorders or drug intoxication responsible for seizures. It is recommended that laboratory investigations should be driven by clinical features indicating a inducible factor, such as those of our patients who had complaints of around oral and fingertip paraesthesia, and thus a serum calcium values were mandatory. In the investigation part of this new episode seizures, studies did not give any use of doing csf analysis and once again, and this is proceed to clinical examination; this is a required study for patients who are HIV positive and also have seizure episodes, because of high risk of CNS infections in these people. In neurologically stable patients after seizure episode within half an hour to one hour and in patients with altered consciousness, electroencephalography (EEG) should be used or when the neurological focal symptoms are not justified by the lesion.
Acute symptomatic seizure etiology is classified as two groups: one is due to neurological insults or injury and the other is due to systemic conditions. Neurological insults include acute stroke (15 percent), traumatic brain injury (15 percent), and CNS infections (14 percent) which are 50 percent of the cases. Electrolyte and metabolic disorders (8%) include systemic diseases; medications, toxic substances and medicines, anoxic encephalopathy. A unique usual cause of symptomatic acute seizures which is related to neurology in sub- Saharan Africa has: neurocysticercosis, a CNS infections and HSV electrolyte disturbances like hyper natremia, hyponatremia, hyper calcemia and hypocalcaemia associated with seizures. Biochemical abnormalities should be found in one day time of seizure episode, in order to electrolyte disturbance with episodes of seizures. Seizures associated with hypocalcaemia depend on how much calcium levels are decreased. Owing to decreased extracellular calcium concentration rather than diminished intracellular levels, the resulting hypocalcaemia results in increased neuronal excitability also generalized seizures tonic clonic or motor focal types which may occur along with decreased calcium levels.
There are no structural brain lesions in acute symptomatic seizures due to electrolyte abnormalities; anyways IH is excluded one as calcification brain or calcinosis also occurs. The pathogenesis remains uncertain, even though the highest occurrences, between 74 percent and 92 percent .Brain calcinosis is postulated to occur due to poor control of calcium and also calcium phosphate high levels, especially in CSF which has deposition of calcium mainly in periventricular area. The most commonly affected locations are the lenti form nucleus and caudate nuclei- basal ganglia, while more severe calcification of intracerebellar area affects other parenchymal structures of brain, as discussed in this patient could occur. The degree of effect of brain with calcification is closely related with the intensity and length of hypocalcaemia, with a crucial period of disease greater than 4 or more years before the period of calcification occurs and a 12 percent increase in the likelihood of brain calcinosis for every year of hypocalcaemia symptoms. Brain calcification's clinical presentation is complex and encompasses the following: seizures, emotional decline and cerebellar and extrapyramidal malfunction movement disorders.the presence of calcinosis of brain in IH can be indicated by seizure episodes, however epilepsy developing risk is 0.9 percent only , implying that the seizure cause may not seem to be linked to brain calcinosis condition instead to the neuronal excitability of low calcium levels. The seizure prevalence in IH was 64 percent in an Indian cohort, upto 90 percent or below had a generalized tonicclonic seizure, while there were also partial complex seizures (4.4 percent) . As in our patient in CT brain it’s easy to visualize basal ganglia calcification, but imaging studies such as 18FFDG used to validate basal ganglia calcification by decreasing glucose uptake by basal ganglia, which directly indicates the degree of calcification of basal ganglia. The recommended therapy for IH is supplementation with calcium and vitamin D, even if it is not shown to slow the brain calcinosis progression.
Calcium preserved in the lower border of normal range is to prevent hypercalciuria and the subsequent nephrolithi asis. Drugs that are used as antiepileptics in the treatment of IH seizures; in the India n cohort of IH and seizure patients, the majority of patien ts got single drug such as phenytoin is used more frequently, then by valproate (40 percent) and carbamazepine and levetiracetam. In this research, for the last three clinic visits, drugs for epilepsy was going on even till 2 years of seizure free episode and only stopped when the patient having regula r EEG and after serum calcium level came up till the average of greater than 1.8 mmol/ L. The first medication discontinued when AEDs were stopped was the drugs which were started first and the dose of the drugs was reduced by 25 percent. The antiepileptic’s drug effects on the absorption activity of calcium and the metabolism of vitamin D influences th e homeostasis of calcium.In this analysis, after the patient had been seizure-free.In an Indian study, when discontinuing antiepileptic drugs such a valproate, phenytoin and carbamazepine was linked with high calcium levels and when we are looking for replacement of calcium and vitamin D, in IH, the calcium effects of AEDs should be taken into co nsideration [4-6].
Conclusion
The case illustrates the acute episode of symptomatic seizures induced by disease mechanisms which are not the usual epilepsy causes and also shows the importance of considering the other treatable conditions being cause of seizures in the proper clinical environment. In this patient, he currently remains seizure free and off antiepileptic medications, despite a previous diagnosis of epilepsy. In addition, we show importantly the hypoparathyroidism entity of brain calcinosis which is also a diagnosis that should also be considered when we find such radiological features in the CT imaging studies.
References
- Ba-Diop A, Marin B, Druet-Cabanac M, et al. Epidemiology, causes, and treatment of epilepsy in sub-Saharan Africa. Lancet Neurol 2014; 13:1029-1044.
- Nardone R, Brigo F, Trinka E. Acute symptomatic seizures caused by electrolyte disturbances. J Clin Neurol 2016; 12:21-33.
- Han P, Trinidad BJ, Shi J. Hypocalcemia-induced seizure: Demystifying the calcium paradox. ASN Neuro 2015; 7:1759091415578050.
- Basak RC. A case report of basal ganglia calcification-a rare finding of hypoparathyroidism. Oman Med J 2009; 24:220.
- Goswami R, Sharma R, Sreenivas V, et al. Prevalence and progression of basal ganglia calcification and its pathogenic mechanism in patients with idiopathic hypoparathyroidism. Clin Endocrinol 2012; 77:200-206.
- Modi S, Tripathi M, Saha S, et al. Seizures in patients with idiopathic hypoparathyroidism: Effect of antiepileptic drug withdrawal on recurrence of seizures and serum calcium control. Eur J Endocrinol 2014; 170:777-783.
Author Info
Kannan Meera Devi*, V Padma, Sathyapriya, Sarath Bhaskar and Saketh Ramineni
1Department of General medicine, Sree Balaji Medical College and Hospital, India2Department of General medicine, Sree Balaji Medical College and Hospital, India
3Department of General medicine, Sree Balaji Medical College and Hospital, India
4Department of General medicine, Sree Balaji Medical College and Hospital, India
Citation: MK Rajasekar, Nithya Balasubramanian, Hypoparathyroidism the Cause of Seizure, Misdiagnosed as Epilepsy, J Res Med Dent Sci, 2021, 9(11): 109-111
Received: 06-Oct-2021 Accepted: 01-Nov-2021