Research - (2024) Volume 12, Issue 8
Rowa Mahmoud Aljondi*, Waad Saad Al-Harthi, Samaher Mohammed Al-Yanbaayi, Abdulrzzag Abdulkarim Alghamdi, Salem Saeed Alghamdi and Abdulrahman Tajaldeen
*Correspondence: Rowa Mahmoud Aljondi, Department of Applied Radiologic Technology, University of Jeddah, Saudi Arabia, Email:
Abstract
Background and Purpose: Among health problems that can damage the brain, stroke is one of the most dangerous. However, there is relatively little information on the risk factors related to stroke in Saudi Arabia, especially in Jeddah. To address this research gap, this study aims to identify stroke features on sectional imaging and associated risk factors in Jeddah, Saudi Arabia. Materials and Methods: A retrospective hospital-based method was conducted with 132 patients to evaluate stroke cases collected from governmental institutions in Jeddah, Saudi Arabia. Results: The study revealed that evidence of stroke was present in the sample of approximately 60% males and 40% females. Most of the patients (81%) were age 50 and older. Regarding the risk factors, the findings showed that 27.5% of the sample had at least 1 of 4 targeted comorbidities (hypertension [HTN], diabetes mellitus [DM], old stroke, and coronary heart disease [CHD]). In this segment of the sample, 67% had HTN, 61% DM, 39% old stroke, and 17% CHD. Furthermore, stroke was acute in most of the patients (60%), chronic in 35%, and subacute in 15%. The majority of the patients had had ischemic stroke (85.5%). Conclusion: The study findings indicated that the males exhibited a higher stroke incidence rate than the females in all age groups. The major type of stroke was ischemic stroke. Males had higher chances of acute strokes, while females had an increased rate of chronic strokes. The most common risk factors were HTN and diabetes. This study suggests that controlling these factors early could help prevent stroke at an older age.
Keywords
stroke; ischemia; CT scan; elderly patients; risk factors; MRI.
Introduction
Stroke is a significant health problem that can lead to death [1, 2]. It prevents oxygen and nutrients from reaching the brain cells, causing them to die within a few minutes. In addition, it may result in various injuries to brain and body functions [3, 4]. Worldwide, it affects more than 15 million people each year [5-7]. It is considered a disease of aging because most strokes occur in older people (more than 65 years old). Moreover, the number stroke is increasing worldwide due to the growth of elderly populations globally [8]. Stroke is one of the main pathologies with the potential to harm the humas brain. It occurs whenever there is a loss of blood supply to any area of the brain, and it is a serious global healthcare problem in both developing and developed countries, resulting in harmful effects on individuals and families at all societal levels [9, 10]. Between 2010 and 2030, it is predicted to affect 4.5 million people per year, leaving more than 9 million stroke survivors around the world [11]. Strokes can occur when brain veins become blocked or arteries in the brain burst, depending on the type of illness. Strokes are divided into two types: ischemic and hemorrhagic [12]. Ischemic stroke is a heterogeneous disease that can be caused by a variety of underlying pathological conditions [13]. It is the most common type of stroke, occurring when a blood vessel in the brain or neck is blocked. An embolism is the movement of a clot from another part of the body to the brain; thrombosis is the presence of a clot within a blood vessel in the brain or neck; and stenosis is the extreme narrowing of an artery in or leading to the brain [14]. About 13% of strokes occur when an artery in or near the brain ruptures; this is called a hemorrhagic stroke. It is considered a life-threatening illness with huge impairment and death rates [15, 16]. Subarachnoid Hemorrhage (SAH) and Intracerebral Hemorrhage (ICH) are two types of hemorrhagic stroke. SAH is bleeding into the subarachnoid space, while ICH is bleeding into the brain parenchyma [17].
Nevertheless, relatively little information exists on the risk factors related to stroke. Still, various non-modifiable risk factors that may cause stroke have been identified, such as genetic factors, race, gender, and age [18-20]. For instance, about one out of every four men and nearly one out of every five women above the age of 45 years can expect to have stroke if they live to their 85th year [21]. Furthermore, modifiable risk factors for stroke have been identified, such as chronic diseases (Hypertension [HTN] And Diabetes Mellitus [DM]), cigarette smoking, obesity, physical inactivity, and trauma [22, 23]. Of these risk factors, HTN is considered the most important due to the long-term increase in blood vessel pressure [24]. The number of patients with stroke may increase in the future because of inadequate control of the major risk factors and demographic changes [25-28]. Ischemic stroke is a frequent complication of Chronic Heart Failure (CHF), a disease that causes serious morbidity and mortality. CHF has been associated with two or three incidences of stroke in individuals. Approximately 15% of strokes are caused by CHF [29]. Computed Tomography (CT) scanning has become the first-line modality for the diagnosis of stroke in emergencies due to its widespread availability, speed, accuracy, and low cost in detecting subarachnoid and cerebral bleeding. CT scans of the brain can diagnose ischemic areas within 6 hours of stroke onset [30]. However, there is limited information on the identification of stroke type on sectional imaging and associated risk factors among patients, especially in Saudi Arabia [31]. This study aims to clarify the features of stroke on sectional imaging and associated risk factors among patients with stroke in Jeddah, Saudi Arabia.
Materials and Methods
Study Design
This is a retrospective study conducted to evaluate the prevalence and incidence of stroke and risk factors among stroke patients. Stroke cases were collected from governmental institutions (King Abdulaziz Hospital and East Jeddah Hospital) in Jeddah, Saudi Arabia, from June 2020 to 2023, including demographic data (e.g., age and gender), patients’ medical history, radiological examination data, imaging findings, stage of stroke, type of stroke, and its location in the brain from radiological reports. The total sample size was 132 patients between 34 and 102 years old. The current study defined a stroke case as a focal neurological deficit caused by a hemorrhage or cerebral infarction, as determined by a CT scan. Only patients who came to the hospital, presented with stroke, and underwent a CT scan and/or had a follow-up MRI scan were included in this study.
Imaging Considerations
Only patients who had a brain CT scan without a contrast agent were included in the present study. MRI was considered for follow-up patients (1.5 Tesla). The site of bleeding was assessed based on brain CT and /or MRI results.
CT Stroke Protocol
CT stroke studies were obtained using CT scanners. The image acquisition protocol was as follows: slice thickness: 10 mm; table increment: 10 mm; acquisition parameters: 120 kVp/300 mA. A caudocranial scanning direction was selected, covering the foramen magnum to the vertex of the skull (Figure 1).
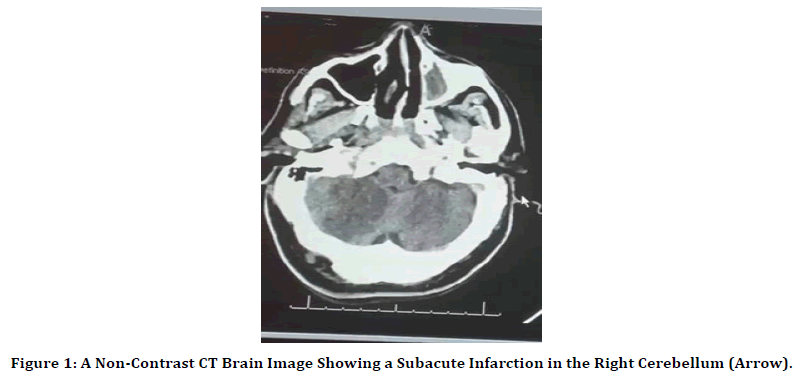
Figure 1. A Non-Contrast CT Brain Image Showing a Subacute Infarction in the Right Cerebellum (Arrow).
MRI Stroke Protocol
MRI stroke protocols were obtained using MRI scanners. The suggested acquisition protocols included at least the following sequences:
1. T1 weighted; plane: sagittal (or volumetric 3D) (T1 FSE) or gradient
2. T2 weighted; plane: axial T2 FSE
3. FLAIR; plane: axial
4. Diffusion-weighted imaging (DWI); plane: axial (Figure 2)

Figure 2. An MRI Brain Image (DWI Sequence) Showing an Acute Infarction in the Left Parietal Lobe (Arrow) with Underlying Hemorrhagic Component.
5. Susceptibility-weighted imaging (SWI); plane: axial
6. MR angiography (MRA); plane: axial with reconstructions
Risk Factors
The medical records of the patients were reviewed to determine the probable etiology of the stroke, independently of any imaging findings, for age, sex, ethnicity, smoking history, history of diabetes, HTN, hyperlipidemia, and clinical diagnosis at the time of the imaging reviews. Upon review of the imaging studies of the brain parenchyma, as well as previous studies, we concluded that the main common risk factors were as follows:
1. HTN: This was diagnosed either by a recall of high BP 140/90 mmHg on different occasions and at different times or from general practitioner records and the use of antihypertensive medications. A transient elevation in BP that settled without treatment was disregarded.
2. DM: This was considered if the random plasma glucose concentration was equal to or higher than 200 mg/dl in the presence of symptoms.
3. Smoking: Smoking status was categorized as either never smoked or currently smoke.
Other factors, such as old stroke or presenting with coronary heart disease, were categorized as no/yes.
Statistical Analysis
All collected data were analyzed using the Statistical Package for Social Sciences (SPSS) Version 26. Descriptive statistical analysis was used for patients’ characteristics and demographics. The Pearson chi-squared (χ2) test was used to compare risk factors and different characteristics of brain stroke. P-values ≤ 0.05 were considered statistically significant. However, many of the variables were collinear, indicating overlap. In these cases, we used only the most statistically significant variable in the final analysis.
Ethical Approval
This study was approved by the institutional review board of the Ministry of Health in Saudi Arabia, IRB number A01362. Patients were informed that their personal information would be kept confidential and that their clinical data and radiological images would only be used for research purposes in this project. A written consent form was waived due to the retrospective, observational nature of the study.
Results
Patient Population
A total of 132 patients admitted to the hospital from 2017 to 2022 were considered for this study. They all received a brain CT at baseline and subsequent follow-up brain MRI later. Furthermore, remote or old carotid infarcts were observed at baseline in 166 patients. All patients without confirmed stroke were excluded. The most frequent indications found in 36 patients included in this study were HTN (66.72%), DM (61.1%), known old stroke (38.9%), and congenital heart defects (16.7%) (Table 1).
| VARIABLES | CATEGORIES | FREQ. | % |
|---|---|---|---|
| Gender | Male | 78 | 59.5 |
| Female | 53 | 40.5 | |
| Total | 131 | 100 | |
| Age | < 40 | 9 | 7 |
| 40–49 | 14 | 10.9 | |
| 50–59 | 28 | 21.7 | |
| 60–70 | 45 | 34.9 | |
| > 70 | 33 | 25.6 | |
| Total | 129 | 100 | |
| Smoking | No | 130 | 99.2 |
| Yes | 1 | 0.8 | |
| Total | 131 | 100 | |
| Comorbidities (having at least one of four diseases: hypertension, diabetes mellitus, old stroke, and coronary heart disease) | No | 95 | 72.5 |
| Yes | 36* | 27.5 | |
| Total | 131 | 100 |
Table 1: Clinical Characteristics of the Study Patients
Clinical and Imaging Variables
The demographic and clinical data of the stroke patients are presented in (Table 2). Most of the stroke patients were older than 60 years (87/131, 60.5%) and more likely to be male (78/13, 59.5%). Approximately two-thirds of the patients (79/131, 60.3%) presented with acute stroke, and 45/131 (34.6%) developed chronic stroke, whereas only 20/131 (15.3%) were diagnosed with subacute stroke. Most patients 112/131 (85.5%) were diagnosed as having ischemic stroke, while the other 15/131 (11.5%) had essentially suffered hemorrhagic stroke. The most common stroke site was intracranial (lobar) infarction (42/131, 32.1%), followed by ischemic stroke in the middle cerebral artery (MCA) (28/131, 21.4%). The least common stroke sites were the Anterior Cerebral Artery (ACA) and Posterior Cerebral Artery (PCA) (both 2/131, 1.5%). Nearly half of the strokes affected the left side of the brain (50/131, 48.1%), somewhat fewer affected the right side (43/131, 41.3%), and only 11 patients (10.6%) had bilateral stroke. In Table 2, none of the percentages under the listed variables sum up to 100% (except “Side of the brain”) because a single patient may be included in more than one category.
| VARIABLE | CATEGORIES | FREQ.* | %** |
|---|---|---|---|
| Stroke stage | Chronic | 45 | 34.6 |
| Acute | 79 | 60.3 | |
| Subacute | 20 | 15.3 | |
| Type of stroke | Ischemic stroke | 112 | 85.5 |
| Hemorrhagic stroke | 15 | 11.5 | |
| Side of the brain | Left hemisphere | 50 | 48.1 |
| Right hemisphere | 43 | 41.3 | |
| Bilateral | 11 | 10.6 | |
| Bleeding site within brain | Anterior cerebral artery (ACA) infarcts | 2 | 1.5 |
| Middle cerebral artery (MCA) infarcts | 28 | 21.4 | |
| Posterior cerebral artery (PCA) infarcts | 2 | 1.5 | |
| Cerebellar infarcts | 21 | 16 | |
| Intraventricular hemorrhage | 4 | 3.1 | |
| Basal ganglia infarcts | 19 | 14.5 | |
| Lobar | 42 | 32.1 | |
| Lacunar infarcts | 14 | 10.7 | |
| Thalamus | 9 | 6.9 |
** None of the percentages under the listed variables sum up to 100% (except “Side of the brain”) because a single patient may be placed in more than one category.
Table 2: Stroke Characteristics of the Study Participants (N = 131)
In (Table 3) no significant association between the risk factors and being at the chronic stage. However, in some of the cases, smaller p-values indicate females having a relatively higher likelihood of being at the chronic stage (42% compared to 30% in males). In addition, hypertensive patients have a relatively higher likelihood of being at the chronic stage (50% compared to 31% in non-hypertensive patients). The same can be seen with diabetes and old stroke, which have similar percentages. Moreover, no significant association was found between the risk factors and being at the acute stage. Here, it is evident that males have a relatively higher likelihood of being at the acute stage (64% compared to 55% in females). Additionally, hypertensive patients had a relatively higher likelihood of being at the acute stage (71% compared to 58% in non-hypertensive patients). However, diabetic patients have a relatively lower likelihood of being at the acute stage (50% compared to 62% in nondiabetics). In addition, patients with CHD have a relatively higher likelihood of being at the acute stage (83% compared to 59% in patients without CHD).
| CHRONIC STAGE | |||||
| RISK FACTORS | CATEGORIES | N | CHRONIC | P-VALUE | |
| No | Yes | ||||
| Gender | Male | 78 | 70.50% | 29.50% | 0.138 |
| Female | 52 | 57.70% | 42.30% | ||
| Age | < 40 | 9 | 55.60% | 44.40% | 0.883 |
| 40–49 | 14 | 71.40% | 28.60% | ||
| 50–59 | 28 | 71.40% | 28.60% | ||
| 60–70 | 44 | 63.60% | 36.40% | ||
| > 70 | 33 | 63.60% | 36.40% | ||
| Hypertension | No | 106 | 68.90% | 31.10% | 0.098 |
| Yes | 24 | 50.00% | 50.00% | ||
| Diabetes | No | 108 | 68.50% | 31.50% | 0.13 |
| Yes | 2 | 50.00% | 50.00% | ||
| Old stroke | No | 116 | 67.20% | 32.80% | 0.239 |
| Yes | 14 | 50.00% | 50.00% | ||
| Coronary heart disease | No | 124 | 65.30% | 34.70% | 1 |
| Yes | 6 | 66.70% | 33.30% | ||
| ACUTE STAGE | |||||
| RISK FACTORS | CATEGORIES | N | ACUTE | P-VALUE | |
| No | Yes | ||||
| Gender | Male | 78 | 35.90% | 64.10% | 0.363 |
| Female | 52 | 45.30% | 54.70% | ||
| Age | < 40 | 9 | 33.30% | 66.70% | |
| 40–49 | 14 | 28.60% | 71.40% | 0.589 | |
| 50–59 | 28 | 50.00% | 50.00% | ||
| 60–70 | 44 | 42.20% | 57.80% | ||
| > 70 | 33 | 33.30% | 66.70% | ||
| Hypertension | No | 106 | 42.10% | 57.90% | 0.356 |
| Yes | 24 | 29.20% | 70.80% | ||
| Diabetes | No | 108 | 37.60% | 62.40% | 0.341 |
| Yes | 22 | 50.00% | 50.00% | ||
| Old stroke | No | 116 | 39.30% | 60.70% | 0.781 |
| Yes | 14 | 42.90% | 57.10% | ||
| Coronary heart disease | No | 124 | 40.80% | 59.20% | 0.402 |
| Yes | 6 | 16.70% | 83.30% | ||
| Female | 52 | 45.30% | 54.70% | ||
Table 3: Identification of Stroke Stages
In (Table 4) diabetes was significantly associated with ischemic stroke (p-value = 0.042). This is reflected in the percentage having this type of stroke in diabetic and nondiabetic patients (100% compared to 83%, respectively); thus, diabetic patients have a relatively higher likelihood of this type of stroke. The results also demonstrate that patients with old strokes have a relatively higher likelihood of ischemic stroke (100% compared to 84% without old stroke). Patients with CHD also have a relatively higher likelihood of ischemic stroke (100% compared to 85% without CHD).
| RISK FACTORS | CATEGORIES | N | ISCHEMIC STROKE | P-VALUE | |
|---|---|---|---|---|---|
| NO | YES | ||||
| Gender | Male | 78 | 15.40% | 84.60% | 0.805 |
| Female | 52 | 13.20% | 86.80% | ||
| Age | < 40 | 9 | 0.00% | 100.00% | 0.402 |
| 40–49 | 14 | 21.40% | 78.60% | ||
| 50–59 | 28 | 10.70% | 89.30% | ||
| 60–70 | 44 | 15.60% | 84.40% | ||
| > 70 | 33 | 18.20% | 81.80% | ||
| Hypertension | No | 106 | 14.00% | 86.00% | 0.751 |
| Yes | 24 | 16.70% | 83.30% | ||
| Diabetes | No | 108 | 17.40% | 82.60% | 0.042 |
| Yes | 22 | 0.00% | 100.00% | ||
| Old stroke | No | 116 | 16.20% | 83.80% | 0.22 |
| Yes | 14 | 0.00% | 100.00% | ||
| Coronary heart disease | No | 124 | 15.20% | 84.80% | 0.592 |
| Yes | 6 | 0.00% | 100.00% | ||
Table 4: Identification of Ischemic Stroke.
Discussion
The current study was conducted to identify the vascular risk factors associated with different stroke types and their distribution within the brain in Jeddah, Saudi Arabia. The distribution of stroke patients included 78 males (60%) and 53 females (40%). This agrees with a study conducted in the city of Al-Madinah Al-Munawarah in Saudi Arabia that examined the rate of first-time stroke incidents in males and females. The distribution of stroke in the sample was 55.49% for men and 44.51% for women [32]. This is also in line with another study conducted in the Ha’il Region in Saudi Arabia that examined the stroke-associated comorbidities of stroke patients, reporting that 59% were males and 41% were females [33]. A similar study conducted in the Riyadh Region, Saudi Arabia, assessed knowledge about stroke risk factors and willingness to make behavioral changes among individuals living in the Kingdom of Saudi Arabia who had experienced a stroke, finding that 58.4% were male and 41.6% were female[34] . Although strokes among women are of a severe nature, stroke is more frequently encountered among men [35]. These differences can be explained by differences in the influence of genes and hormones according to gender [36-38]. A number of studies have explored the connection between genes and atherosclerosis, finding that male plaques are controlled by a gene connected with the myeloid, immune, and hematological systems [36-38]. Vascular structure can be affected by sex hormones [39]. Estradiol, which is a type of estrogen hormone, may prevent low-density lipoprotein (LDL) consumption and metabolism, and it is known that estradiol can protect premenopausal females from stroke [32]. However, after menopause, the protection gradually decreases as the levels of estradiol decrease. Previous studies have demonstrated an increase in female ischemic stroke after menopause and a decrease in sexual hormones [40-42]. Testosterone was found to be a great antiatherogenic; however, this is not the case when the level of testosterone is high or if there is excessive use of external testosterone [43]. Consistent with previous studies, we found that the incidence of stroke increases with age [44, 45]. The results of our study showed that the average age of most stroke patients was 50 years, representing 81% of the sample. This is in line with a study with a Saudi Arabian cohort that found that the incidence of stroke increased with age, especially at the age of 75 years and above, in both men and women. A study from the Ha’il Region in Saudi Arabia showed that men are more susceptible to stroke when they are younger, whereas older women are more susceptible as they age. In a prospective observational study conducted with 13,822 Middle Eastern and North African stroke patients to investigate age distribution, stroke subtypes, severity grades, risk factors, functional outcomes, and level of care, a predominant prevalence of stroke and a mean stroke age range of 59 to 71 years were found in males [46]. This can also be connected to hormonal changes. It has been shown that older females who had stroke at an older age had unpleasant outcomes, as they faced a decrease in life quality, mental issues such as depression, and cognitive deficits. Stroke is a rapidly expanding health concern in Saudi Arabia, where it is regarded as a leading cause of illness and death. This is related to the country’s rapidly changing lifestyle and the high prevalence of cardiovascular diseases, such as HTN, diabetes, dyslipidemia, and obesity, all of which are key risk factors for stroke. Studies conducted in Saudi Arabia have shown that HTN and DM are the two main causes of ischemic stroke. The results of our study demonstrated that 27.5% of the sample proved to have at least 1 of 4 comorbidities (67% HTN, 61% DM, 39% old stroke, and 17% CHD). HTN and diabetes are the most common risk factors associated with stroke. It is known that HTN is the main cause of hemorrhagic stroke due to increased blood pressure. Previous studies and trials have also highlighted a significant relationship between stroke and HTN. DM is also considered a risk factor for all types of strokes, and the disease is more common in ischemic stroke patients than in hemorrhagic stroke patients. The results of our study identified the types of strokes, as well as their location and the side of the brain affected by stroke. Overall, the most prevalent stroke type was ischemic (85.5%), which was found to be more likely to affect diabetic patients. Regarding the stages of stroke, males were more likely to have an acute stroke than females, while females had a relatively higher risk of chronic stroke. In our study, more than half of the cases had a stroke in the left hemisphere, 40% in the right hemisphere, and 10% had bilateral strokes. The findings suggest that the locations with the highest likelihood of stroke are the cerebral lobes (32% of the patients) and the MCA (21%, mostly occurring in younger patients). Diabetic patients exhibited a higher rate of stroke and thalamic hemorrhage compared to nondiabetic patients. The evidence further revealed that an increase in the risk factors associated with hemorrhagic stroke, such as HTN, previous cerebral hemorrhage, and chronic hepatic disease, might increase the percentage incidence of hemorrhagic stroke and its distribution within the brain. Knowledge of vascular risk factors and cerebral anatomy is crucial for understanding the mechanisms involved in the localization of strokes. The main limitations of this study included the sample size and the unequal distribution of vascular risk factors in stroke patients. It was difficult to retrospectively identify the vascular risk factors and distribution of strokes, as there was not enough follow-up data for measurable risk factors. This was because in most of the cases, these results were conducted on first-time visiting patients at the hospitals. Furthermore, there was a lack of information on the patients in the medical records system due to the rapid and urgent methods of treatment; most stroke patients were admitted through the emergency room. Therefore, the results cannot be generalized to the entire population. Further expanded longitudinal studies that include larger sample sizes are needed, with follow-up assessments to clarify the relationship between risk factors and their distribution in stroke patients.
Conclusion
The findings of this study highlight the stroke regions most affected by vascular risk factors. HTN and diabetes are the most common risk factors associated with stroke. The majority of strokes were of the ischemic type, and diabetic patients had a relatively higher likelihood of ischemic stroke. Ischemic stroke most commonly affected regions within the brain in the MCA, which was common in the younger patients (< 40 years old), and the thalamus was the region most affected with stroke in diabetic patients. Males had a higher stroke incidence rate than females in all age groups. Regarding the stages of stroke, males were more likely to have an acute stroke than females, while females had a relatively higher risk of chronic stroke. This study suggests that controlling these factors early could help prevent stroke at an older age. Finally, it is strongly recommended that the awareness of the vascular risk factors of stroke be raised in the Kingdom of Saudi Arabia.
References
- Vl F. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003; 2:43-53.
- Feigin VL, Owolabi MO, Abd-Allah F, et al. Pragmatic solutions to reduce the global burden of stroke: a World Stroke Organization–Lancet Neurology Commission. Lancet Neurol. 2023; 22:1160-206.
- Algahtani H, Shirah B, Hachinski V. Primordial and Primary Prevention of Ischemic Stroke in Saudi Arabia: A Combination Approach and Evolving Concepts. Saudi J Med Med Sci. 2024; 12:1-9.
- Christensen H. Long-term disability after transient ischaemic attack or minor stroke. Lancet Neurol. 2022; 21:859-60.
- Update AS. Heart disease and stroke statistics–2017 update. Circ. 2017; 135:e146-603.
- Roy-O’Reilly M, McCullough LD. Age and sex are critical factors in ischemic stroke pathology. Endocr. 2018; 159:3120-31.
- Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circ. 2011; 123:933-44.
- Chen R, Ovbiagele B, Feng W. Diabetes and stroke: epidemiology, pathophysiology, pharmaceuticals and outcomes. AJMS. 2016; 351:380-6.
- Wolfe CD. The impact of stroke. Br Med Bull. 2000; 56:275-86.
- Cloud GC, Williamson JD, Tran C, et al. Low-dose aspirin and the risk of stroke and intracerebral bleeding in healthy older people: secondary analysis of a randomized clinical trial. JAMA Netw Open. 2023; 6:e2325803-.
- Ahmed HG, Alquwaiay FK, AlDhamadi HF, et al. Stroke-associated comorbidities in Saudi Arabia. IJPRAS. 2020;9(2-2020):91-8.
- Nakibuuka J, Sajatovic M, Nankabirwa J, et al. Stroke-risk factors differ between rural and urban communities: population survey in Central Uganda. NEEPD. 2015; 44:156-65.
- Namale G, Kamacooko O, Kinengyere A, et al. Risk Factors for Hemorrhagic and Ischemic Stroke in Sub‐Saharan Africa. J Trop Med. 2018; 2018:4650851.
- Tai SY, Lu TH. Why was COVID-19 not the first leading cause of death in the United States in 2020? Rethinking the ranking list. AJPH. 2021; 111:2096-9.
- Li X, Chen G. CNS-peripheral immune interactions in hemorrhagic stroke. JCBFM. 2023; 43:185-97.
- Magid-Bernstein J, Girard R, Polster S, et al. Cerebral hemorrhage: pathophysiology, treatment, and future directions. Circ Res. 2022; 130:1204-29.
- Montaño A, Hanley DF, Hemphill III JC. Hemorrhagic stroke. Handb Clin Neurol. 2021; 176:229-48.
- Witt BJ, Brown Jr RD, Jacobsen SJ, et al. Ischemic stroke after heart failure: a community-based study. Am Heart J. 2006; 152:102-9.
- Haupt M, Gerner ST, Bähr M, et al. Neuroprotective strategies for ischemic stroke—future perspectives. Int J Mol Sci. 2023; 24:4334.
- Alfakeeh FK, Alghamdi YM, Alharbi BF, et al. HbA1c and risk factors’ prevalence in patients with stroke: a retrospective study in a tertiary care hospital in Saudi Arabia. Neurosci J. 2024; 29:18-24.
- Lip GY, Rasmussen LH, Skjøth F, et al. Stroke and mortality in patients with incident heart failure: the Diet, Cancer and Health (DCH) cohort study. BMJ open. 2012; 2:e000975.
- Kang SH, Kim J, Park JJ, et al. Risk of stroke in congestive heart failure with and without atrial fibrillation. Int J Cardiol. 2017; 248:182-7.
- Pullicino PM, Halperin JL, Thompson JL. Stroke in patients with heart failure and reduced left ventricular ejection fraction. Neurology. 2000;54:288-.
- Haeusler, K.G., U. Laufs, M. Endres, Chronic heart failure and ischemic stroke. Stroke, 2011. 42: p. 2977-2982.
- Pullicino P, Homma S. Stroke in heart failure: atrial fibrillation revisited?. J Stroke Cerebrovasc Dis. 2010;19:1-2.
- Doubal FN, Dennis MS, Wardlaw JM. Characteristics of patients with minor ischaemic strokes and negative MRI: a cross-sectional study. JNNP. 2011;82:540-2.
- Silva GS, Koroshetz WJ, González RG, et al. Causes of ischemic stroke. Acute ischemic stroke: Imaging and Intervention. 2011:25-42.
- Almandoz JE, Pomerantz SR, González RG, et al. Imaging of acute ischemic stroke: Unenhanced computed tomography. AIS, acute ischemic stroke. 2010:43-56.
- Gautam A, Raman B. Brain strokes classification by extracting quantum information from CT scans. Multim Tools Appl. 2023; 82:15927-43.
- Edzie EK, Gorleku PN, Dzefi-Tettey K, et al. Incidence rate and age of onset of first stroke from CT scan examinations in Cape Coast metropolis. Heliyon. 2021;7.
- Alahmari K, Paul SS. Prevalence of stroke in Kingdom of Saudi Arabia-through a physiotherapist diary. Mediterr J Soc Sci. 2016; 7:228.
- Al-Shenqiti AM, Ibrahim SR, Khaled OA, et al. Incidence of first time stroke: a Saudi experience. Eur Neurol. 2017; 77:147-51.
- Ahmed HG, Alquwaiay FK, AlDhamadi HF, et al. Stroke-associated comorbidities in Saudi Arabia. IJPRAS. 2020; 9:91-8.
- Althomali M, Liberatos P, Mubaraki AA, et al. Understanding risks for stroke and the importance of a healthy lifestyle among stroke patients at a tertiary hospital in Saudi Arabia. Saudi j health sci. 2024; 13:56-77.
- Appelros P, Stegmayr B, Terént A. Sex differences in stroke epidemiology: a systematic review. Stroke. 2009; 40:1082-90.
- Gasbarrino K, Di Iorio D, Daskalopoulou SS. Importance of sex and gender in ischaemic stroke and carotid atherosclerotic disease. Eur Heart J. 2022; 43:460-73.
- Hartman RJ, Owsiany K, Ma L, et al. Sex-stratified gene regulatory networks reveal female key driver genes of atherosclerosis involved in smooth muscle cell phenotype switching. Circ. 2021; 143:713-26.
- Hartman R, Siemelink M, Haitjema S, et al. Sex-dependent gene regulation of human atherosclerotic plaques by DNA methylation and transcriptome integration points to smooth muscle cell involvement in women. Atherosclerosis. 2021; 331:e217.
- Arnold AP, Cassis LA, Eghbali M, et al. Sex hormones and sex chromosomes cause sex differences in the development of cardiovascular diseases. ATVB. 2017; 37:746-56.
- Joseph J, Varkey BP, Varghese A, et al. Age, gender, and regional variations in stroke epidemiology in India: A systematic review and meta-analysis. IJCFM. 2024; 10:7-17.
- Shekhar S, Travis OK, He X, et al. Menopause and ischemic stroke: a brief review. MOJ toxicology. 2017; 3.
- Lisabeth L, Bushnell C. Stroke risk in women: the role of menopause and hormone therapy. Lancet Neurol. 2012; 11:82-91.
- Alves JV, da Costa RM, Pereira CA, et al. Supraphysiological levels of testosterone induce vascular dysfunction via activation of the NLRP3 inflammasome. Front Immunol. 2020; 11:1647.
- Asirvatham AR, Marwan MZ. Stroke in Saudi Arabia: a review of the recent literature. PAMJ. 2014; 17.
- Alharbi AS, Alhayan MS, Alnami SK, et al. Epidemiology and risk factors of stroke. Arch Pharm Pract. 2019; 10:60-6.
- Rukn SA, Mazya MV, Hentati F, et al. Stroke in the Middle-East and North Africa: A 2-year prospective observational study of stroke characteristics in the region—Results from the Safe Implementation of Treatments in Stroke (SITS)–Middle-East and North African (MENA). Int J Stroke. 2019;14:715-22.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Rowa Mahmoud Aljondi*, Waad Saad Al-Harthi, Samaher Mohammed Al-Yanbaayi, Abdulrzzag Abdulkarim Alghamdi, Salem Saeed Alghamdi and Abdulrahman Tajaldeen
Department of Applied Radiologic Technology, University of Jeddah, Saudi ArabiaPublished: 28-Oct-2024
