Case Report - (2020) Volume 8, Issue 6
Immediate Implant Placement in Fresh Extraction Socket With Xenograft and Platelet Rich Fibrin-A Case Report
Koyel Bhowal*, Samiran Ghosh and Soumitra Ghosh
*Correspondence: Koyel Bhowal, Department of Oral and Maxillofacial Surgery, Guru Nanak Institute of Dental Sciences and Research, India, Email:
Abstract
Immediate implantation has provided the opportunity to achieve better and faster functional results. The placement of implant immediately not only prevents the collapse of the socket by reducing the crestal bone loss, but also enhances the soft tissue esthetics. A variety of regenerative techniques using combinations of bone grafts and barrier membranes have been suggested promoting bone regeneration in localized defects at implants placed into extraction sockets. Platelet rich fibrin (PRF) possesses an inherent property to accelerate soft and hard tissue healing. It has several advantages which include ease of preparation/application, minimal expense, and lack of biochemical modification. Recently, a combination between bone graft materials and Platelet-Rich- Fibrin (PRF) is implemented in the implantology. In this article, a case report has been elaborated where a healthy patient with 18 years old having fractured maxillary anterior tooth. Following extraction of tooth dental implant was placed within extraction socket and labially placed xenograft and platelet rich fibrin along with barrier membrane. The aim of this case report was to assess the possibility for augmentation of the alveolar ridge in the frontal region of the upper jaw, utilizing a combination of bone graft material, mainly xenograft and platelet rich fibrin.
Keywords
Immediate implant, Xenograft, Platelet rich fibrin
Introduction
Implant-supported restoration of the maxillary anterior segment that is biologically, functionally, and esthetically acceptable following traumatic injuries in the maxillary anterior segment is always complex [1]. Careful extraction of the fractured root, residual labial bone preservation, proper flap design, ideal positioning of the implant, appropriate soft tissue contour, and the crown emergence are all important steps necessary to achieve a predictable, stable, functional, and esthetic success [2]. Immediate implants were first described by Schulte, et al. in a clinical report, followed by histologic studies that confirmed the procedure as successful. They are designed to prevent bone resorption following extraction. With this method, the ridge dimension and height are maintained, and several surgical procedures omitted, shortening the healing period. However, healing of the tissues is always difficult to control and the development of new techniques and materials to improve these treatments is still necessary [3]. A variety of regenerative techniques using combinations of bone grafts and barrier membranes have been suggested promoting bone regeneration in localized defects at implants placed into extraction sockets. GBR is the most frequently used technique for bone regeneration in conjunction with or prior to implant placement. Platelets play a crucial role not only in hemostasis, but also in the wound healing process. PRF represents a new revolutionary step in the platelet gel therapeutic concept. Unlike other platelet concentrates, this technique does not require any gelifying agent, but no more than centrifugation of the natural blood without additives. Zaki et al. developed the PRF in 2001 in France and the production protocol of PRF attempted to accumulate platelets and released cytokines in a fibrin clot. This biomaterial presents a specific biology which offers several advantages including promoting wound healing, bone growth and maturation, graft stabilization, wound sealing, and hemostasis, and improving the handling properties of graft materials. PRF can also be used as a membrane. Clinical trials suggest that the combination of bone grafts and growth factors contained in PRF may be suitable to enhance bone density [4].
Case Report
An 18-year-old woman presented with a fractured maxillary right central incisor that was fractured during a recent sport-related accident. Probing pocket depths and mobility of adjacent teeth were within normal limits. Diagnostic impressions were taken. Clinical examination of the remaining root or tooth in need for extraction to ensure absence of infection and presence of four intact socket walls. Preoperative CBCT radiograph was evaluated. CBCT showed fractured of 11 and no fracture of labial and palatal cortex.
Surgical procedure
Briefly after induction of local anesthesia (block and infiltration with 1:1,00,000 epinephrine), atraumatic extraction of 11 was done with periotome. Following extraction, a thorough curettage of the remaining alveolus was performed to eliminate any residual infective tissue in the avulsion socket that could compromise the osseointegration of an immediately placed implant. sequential drilling with copious irrigation was carried out till the desired dimensions (2-3 mm apical to the apical part of the socket to get proper primary stability).4mm diameter and 14 mm length implant was placed in 11 region and primary stability achieved was 35 N-cm (Figures 1 and 2).
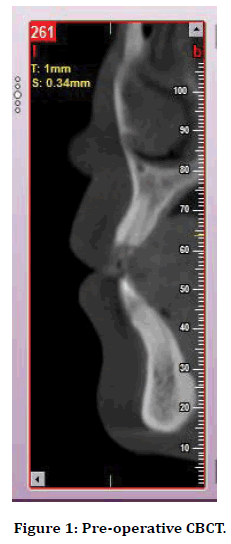
Figure 1. Pre-operative CBCT.
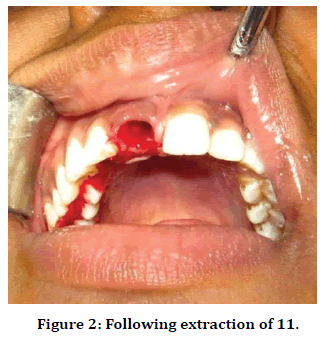
Figure 2. Following extraction of 11.
Preparation of Platelet rich fibrin (PRF-)
The PRF preparation for the test group was started 30 minutes before surgery.
Ten milliliters of whole blood were drawn by venipuncture of the antecubital.
vein and collected into two blood collection tubes (test tube).
The tubes were initially centrifuged for 10 min at the rate of 3,000 revolutions per minute.
Blood centrifugation immediately after collection allows the composition of a structured fibrin clot in the middle of the tube, just between the red corpuscles at the bottom and the acellular platelet-poor plasma at the top.
The PRF was easily separated from the red corpuscles base (preserving a small red blood cell layer) using a sterile tweezers and scissors just after removal of poor platelet plasma, and then transferred onto a sterile dapen dish.
Xenograft and platelet rich fibrin were mixed and placed labially between implant and labial cortical bone. The bone graft was covered with resorbable collagen membrane, which was covered by healing abutment. Sutures were placed in interproximal gingival adjacent to implant.
Prosthetic phase
After 3 months’ porcelain fused to metal crown restorations were placed after radiographic evaluation and determining their final stability.
Postoperative follow up
Post-operative follows up continue clinically and radiographically 6 months followed crown placement (Figures 3 to 16).

Figure 3. Drawing blood (9ml of blood as per requirement).
Figure 4. The centrifuge.

Figure 5. Platelet rich fibrin.
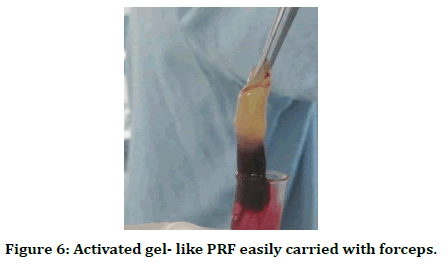
Figure 6. Activated gel- like PRF easily carried with forceps.
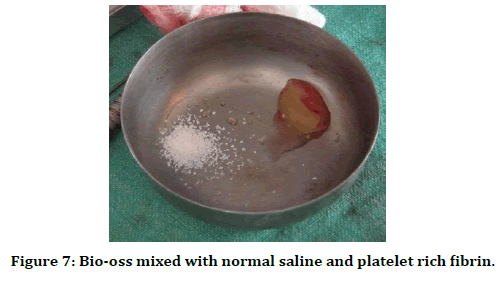
Figure 7. Bio-oss mixed with normal saline and platelet rich fibrin.
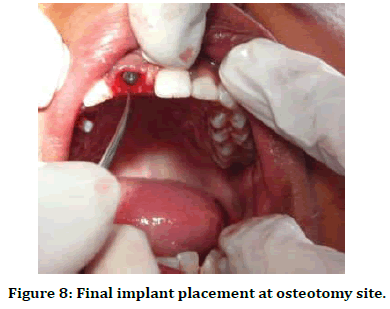
Figure 8. Final implant placement at osteotomy site.
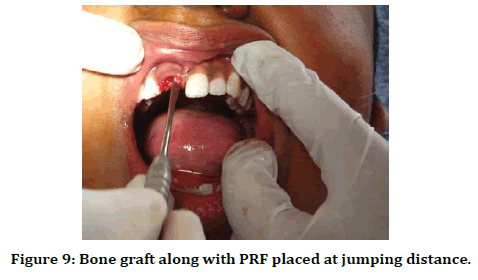
Figure 9. Bone graft along with PRF placed at jumping distance.
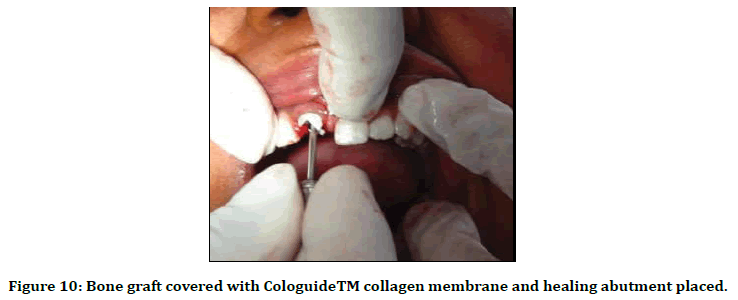
Figure 10. Bone graft covered with CologuideTM collagen membrane and healing abutment placed.
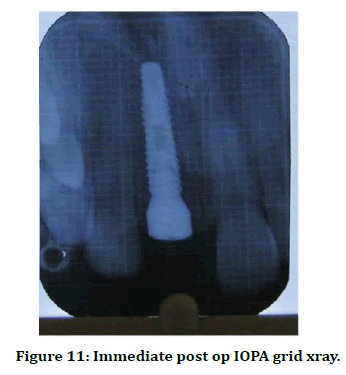
Figure 11. Immediate post op IOPA grid xray.
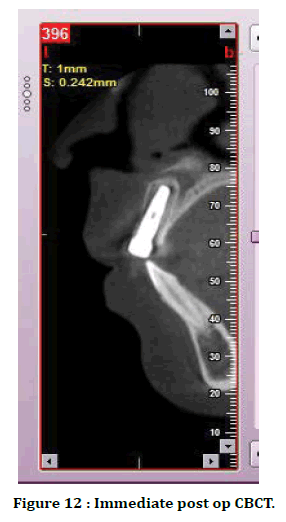
Figure 12. Immediate post op CBCT.
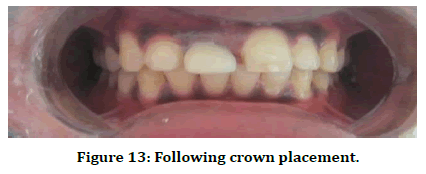
Figure 13. Following crown placement.
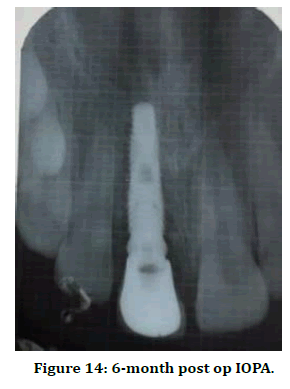
Figure 14. 6-month post op IOPA.
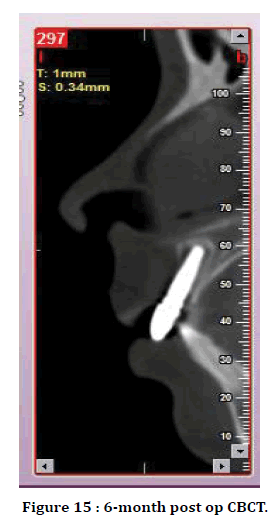
Figure 15. 6-month post op CBCT.
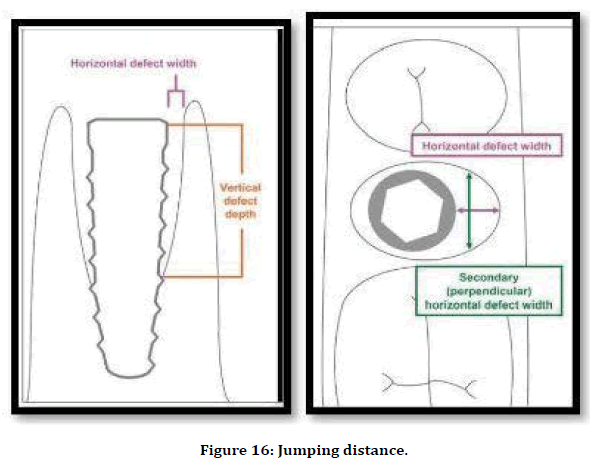
Figure 16. Jumping distance.
Discussion
When a dental implant is placed into a fresh extraction socket, a space between the implant periphery and surrounding bone occurs. A gap can occur on any aspect of an immediately placed implant: Buccal, lingual, or proximally. This space between the implant periphery and surrounding bone is called the gap or jumping distance. Bone fill in the gap between the implant and the peripheral bone is important [4].
GBR is a surgical procedure that uses barrier membranes with or without particulate bone grafts or/and bone substitutes. Osseous regeneration by GBR depends on the migration of pluripotential and osteogenic cells(e.g. osteoblasts derived from the periosteum and/or adjacent bone and/or bone marrow) to the bone defect site and exclusion of cells impeding bone formation(e.g. epithelial cells and fibroblasts) [5].
Xenografts are graft materials derived from the inorganic portion of animal bones; the most common source is bovine the removal of the organic component are processed to remove their antigenicity, while the remaining inorganic components provide a natural matrix as well as an excellent source of calcium. The first documented xenograft was done in 1600 [6]. The disadvantage of xenografts is that they are only osteoconductive and the resorption rate of bovine cortical bone is slow. In addition, patients may have anxiety to mad cow disease or bovine spongiform encephalitis [7]. According to Artzi et al. the disadvantages of the use of bovine bone include its slow resorption and healing with fibrous encapsulation that leads to very protracted or even no remodeling in the central part of the augmented socket [8].
In the year 2014, Kulkarni et al. stated that PRF is an excellent material for enhancing wound healing. The use of PRF dressings may be a simple and effective method of reducing the morbidity associated with donor sites of autogenous free gingival grafts [9].
Arrejaie et al. performed a study on 32 sites from 16 patients, divided into two groups. One group received an immediate implant with xenograft with PRF and another group received only xenograft. They observed that after 12 months of post-surgery regarding the reduction of defect height, no statistically significant differences were found between both groups [10].
Conclusion
In several studies showed platelet-rich fibrin (platelet-rich fibrin PRF) placed along with immediate implants in patients after tooth extraction showed high success rate .This technique offers advantages for patient comfort and the healing process as it contains many growth factors. It also facilitates elimination of post extraction healing period, reduction of the number of surgical sessions, preservation of alveolar width and height the fresh extraction sockets. Long term follow up required as according to Arrejaie et al. CBCT has a limitation in which it cannot differentiate between the natural bone and xenograft bone at 6 and 9 months because xenograft bone requires a long time to be replaced by natural bone.
Conflict of Interest
The authors confirm that this article content has no conflict of interest.
Consent
Written informed consent were obtained from the patients for publication of this case report and accompanying images.
References
- Amet EM. Management of unscheduled anterior tooth or prosthesis loss with extraction and immediate implant placement: A clinical report. J Oral Implantol 2010; 36:209–218.
- Dohan Ehrenfest DM, Vazquez L. Pulling out, extraction or avulsion? Implant Dent 2008; 17:4.
- Shulte W, Heimke G. The tubinger immediate implant. Quintessenz 1976; 27:17-23.
- Zaki SA, Mohamed SS, Hommos AM, et al. Study of the effect of the combination of platelet-rich fibrin (prf) and allogenous bone graft around immediate implants. Alexandria Dent J 2017; 42:127-134.
- Botticelli D, Berglundh T, Buser D, et al. The jumping distance revisited an experimental study in the dog. Clin Oral Implants Res 2003; 14:35-42.
- Cutrim ES, Peruzzo DC, Benatti B. Evaluation of soft tissues around single tooth implants in the anterior maxilla restored with cemented and screw-retained crowns. J Oral Implantol 2012; 38:700-705.
- Hassan KS, Alagl AS. Immediate dental implants, and bone graft. Implant dentistry the most promising discipline of dentistry. Intech Open 2011; 3:173-82.
- Artzi Z, Tal H, Dayan D. Porous bovine bone mineral in healing of human extraction sockets. Part 1 histomorphometry evaluations at 9 months. J. Periodontol 2001; 71:1015–1023.
- Kulkarni MR, Thomas BS, Varghese JM, et al. Platelet-rich fibrin as an adjunct to palatal wound healing after harvesting a free gingival graft: A case series. J Indian Soc Periodontol 2014; 18:399-402.
- Arrejaie A, Al-harbi F, Alagl AS, et al. Platelet-rich plasma gel combined with bovine-derived xenograft for the treatment of dehiscence around immediately placed conventionally loaded dental implants in humans: Cone beam computed tomography and three-dimensional image evaluation. Int J Oral and Maxillofacial Implants 2016; 1:31.
Author Info
Koyel Bhowal*, Samiran Ghosh and Soumitra Ghosh
Department of Oral and Maxillofacial Surgery, Guru Nanak Institute of Dental Sciences and Research, Panihati, Kolkata, IndiaCitation: Koyel Bhowal, Samiran Ghosh, Soumitra Ghosh, Immediate Implant Placement in Fresh Extraction Socket WithXenograft and Platelet Rich Fibrin–A Case Report, J Res Med Dent Sci, 2020, 8 (6): 163-169.
Received: 21-Aug-2020 Accepted: 21-Sep-2020
