Research Article - (2022) Volume 10, Issue 12
Incidence of Subclinical Hypothyroidism in GDM With increased risk of Preterm Delivery
V Sathya1, Giridharan Bupesh2 and S Vasanth1*
*Correspondence: Dr. S Vasanth, Department of Research and Development wing, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chromepet, Chennai, Tamil Nadu, India, Email:
Abstract
Metabolic and many endocrine changes during pregnancy are mainly due to the minor alterations in physiology of mother and fetus. The two common endocrinopathies during pregnancy are gestational diabetes mellitus and thyroid disorders. However, there is no sufficient evidence to prove the association between subclinical hypothyroidism, Gestational Diabetes Mellitus (GDM) and perinatal outcome. Hence, the present clinical investigation is to determine the combined morbidity of GDM and subclinical hypothyroidism and its association with adverse maternal and fetal outcomes. The rate of preterm delivery is elevated in GDM cases with SCH and 21% of SCH pregnant women had preterm delivery compared to 5.6% in euthyroid cases and was statistically significant (p=0.20). The studies also indicate an increased risk of subclinical hypothyroidism in women with GDM and maternal thyroid hormone status was related to the degree of metabolic imbalance. The screening for GDM in women during early pregnancy tends to reduce morbidity in foetus and mother through dietary or drug management. Furthermore, the study emphasizes on the importance of evaluation of thyroid function in women with GDM owing to the increase in high perinatal and neonatal morbidity.
Keywords
Subclinical hypothyroidism, Gestational diabetes mellitus, Neonatal morbidity, Preterm delivery
Introduction
Metabolic and many endocrine changes during pregnancy are changes on the borderline between due to the minor alterations in physiology of mother and fetus. The two common endocrinopathies during pregnancy are gestational diabetes mellitus and thyroid disorders. Gestational diabetes mellitus is the most common risk factor during pregnancy, which affects both the mother and the fetus. The other complications of gestational diabetes mellitus are hypertension, caesarean sections, macrocosmic fetuses and shoulder dystocia, fetal demise, neonatal hypoglycaemia, polycythaemia, neonatal jaundice and hypocalcaemia are the other complications of patients with Gestational Diabetes Mellitus (GDM) [1,2].
The second common endocrinopathy during pregnancy is hypothyroidism [3]. Hypothyroidism during pregnancy will lead to higher rate of abortion during the stage of gestation, gestational hypertension, postpartum haemorrhage and placental abruption. Uncontrolled hypothyroidism during pregnancy has a great risk of developing multinodular goiter and small or large gestational age. Increased risk of miscarriage, intrauterine fetal death, developmental disorders and mental illness is the serious effects of maternal hypothyroidism. Based on the hormonal level and clinical presentation. Thyroid disorder is divided into clinical and sub clinical disease. A prevalence range of 2% to 5% is seen in subclinical hypothyroidism [4]. The thyroid gland will get affected by sustained hyperglycaemia and continuous endeavours by the body to correct for this imbalance of carbohydrate metabolism. So many studies shows that diabetes mellitus and thyroid dysfunction are found to exit together [5,6]. Both thyroid metabolism and carbohydrate metabolism will result in functional abnormalities of one another. American Diabetes Association (ADA) proposed that pregnant woman with diabetes mellitus should be periodically checked for thyroid dysfunction [7].
However there is no sufficient evidence to prove the association between subclinical hypothyroidism and gestational diabetes mellitus and perinatal outcome. Earlier reports suggest an increased risk for subclinical hypothyroidism in women with GDM. Hence, we conducted a clinical study to determine the combined morbidity of GDM and subclinical hypothyroidism and its association with adverse maternal and fetal outcome.
When a woman’s pancreatic function is unable to overcome the diabetogenic potency during pregnancy, this leads to a condition called as gestational diabetes mellitus. GDM is defined as any carbohydrate intolerance that appears during pregnancy [8].
In US, annually 1,35,000 cases of GDM cases (3-8%) and in India (18.9%) are diagnosed are reported during pregnancy. The risk factors for GDM are calculated using obstetric, family and personal history with current pregnancy [9,10].
Insulin resistance, beta cell dysfunction and GDM: Majority of women with GDM appear to have beta cell dysfunction which leads to insulin resistance and found to be higher in pregnant women [11]. Measurement of insulin sensitivity before and after pregnancy has shown insulin resistance in both lean and obese women who had developed GDM. Leptin, inflammatory marker TNF-2, C-reactive protein are elevated and reduced adiponectin have been noticed in some women with GDM. Additionally, alteration in insulin signalling pathway, reduction in PPAR expression and abnormal subcellular localization of GLUT4 transporters and decrease in insulin meditated fat cells are observed in women with GDM. Beta cell dysfunction over years, leads to progressive hyperglycemia and diabetes mellitus. The genetics of GDM is not well understood in women who are all affected with chronic insulin resistance.
Screening and testing strategies: IADPSG and American Diabetes Association (ADA) has endorsed a fasting plasma glucose level>126 mg/dl (6.99 mmol/L), Hb Alc>6.5% (748 mmol/mol) and random blood sugar>200 mg/dl (11.1 mmol/l) for diagnosing GDM and GTT with 75 gram, 2 hours oral glucose tolerance test at 24-28 weeks of gestation.
However, the ACOG recommends universal screening as the most sensitive approach for diagnosing GDM. Glucose challenge test, 50 g glucose, 1 hour glucose challenge test at 24-28 weeks of gestation in the first step in screening GDM. Glucose concentration>130 mg/dl (>7.22 mmol/l) or 140 mg/dl (>7.77 mmol) if followed with 100 g, 3 hour oral GTT.
O’ Sullivan criteria for diagnosing GDM by using the 100 g, 3 hours OGTT, along with subsequently derived values (Tables 1 and 2).
| Time of glucose measurement | Original values (O’ Sullivan and Mahan), whole blood, somogyi-nelson method |
Rounded O’ Sullivan values | NDDG (NDDG modification) plasma |
C&C modification (carpenter and coustan), plasma, glucose oxidase |
|---|---|---|---|---|
| Fasting | 90 | 90 | 105 | 95 |
| 1 hour | 165 | 165 | 190 | 180 |
| 2 hour | 143 | 145 | 165 | 155 |
| 3 hour | 127 | 125 | 145 | 140 |
Table 1: Threshold glucose values, mg/dl (mmol/L).
| At first visit, assign diagnosis of pre-existing diabetes if any of the following are present: |
| Fasting blood glucose ≥ 126 mg/dl (≥ 6.99 mmol/L) |
| HbA1c ≥ 6.5% (≥ 48 mmol/ml) |
| Random blood glucose ≥ 200 mg/dl (≥ 11.1 mmol/L) |
| At first visit, assign diagnosis of GDM if present: |
| Fasting blood glucose ≥ 92 mg/dl (≥ 5.11 mmol/L) and<126 mg/dl (<6.99 mmol/L) |
| At 24-28 weeks gestation, perform 75 gm, 2 hours OGTT. assign diagnosis of GDM if one or more of the following blood glucose values is met or exceeded: |
| Fasting 92 mg/dl (5.11 mmol/L) |
| 1 hour 180 mg/dl (9.99 mmol/L) |
| 2 hour 153 mg/dl (8.49 mmol/L) |
Table 2: IADPSG recommendations..
Adapted from the international association of diabetes and pregnancy study groups consensus panel.
Complications of GDM: Urinary tract infection is the common condition experienced by women who do not have GDM. An increased risk of pylonephritis preeclampsia asymptomatic bacteriuria is the other risk factors of GDM. Moreover, there is a risk of about 10% of polyhydraminisos with the additional risk of abruption placentae, preterm labor and postpartum uterine atony if glucose control is very poor with increased incidence of still birth and macrosomia at 26 to 28 weeks of gestation. Consequently, neonatal hypoglycemia, shoulder dystocia and fetopelvic disproportion that may lead to operative delivery are the complications associated with macrosomia.
Subclinical hypothyroidism: The Subclinical Hypothyroidism (SCH) during pregnancy is defined as elevated levels of serum Thyroid Stimulation Hormone (TSH) and determined using serum thyroxine total T4 or Free T4 (FT4) concentration as reference. The serum triiodothyronine (total T3) level is normal. Subclinical hypothyroidism mostly occurs in pregnant women (2-2.5%) and most prevalent in China (4.0%), Belgium (6.8%) and very high in northern Spain (13.7%) and less than 2% in children.
The diagnosis of SCH are based on laboratory test reports as there is no specific symptoms for SCH and hypothyroidism and varies with lifestyle modificatication or conditions like pregnancy. The primary hypothyroidism is identified based upon the elevated level of serum TSH concentration using trimester specific TSH reference ranges to prevent misclassification of thyroid dysfunction during pregnancy.
The recommended range as per American thyroid association includes 0.1 to 2.5 mV/l, 0.2 to 3.0 mV/l and 0.3 to 3.5 mV/l for first, second and third trimester respectively and also characterized with elevated iodine renal clearance, serum T4 binding globulin and placental inner ring de iodination of T3 and T4.
The most frequent cause of hypothyroidism in developing countries is due to severe iodine deficiency and chronic autoimmune thyroiditis in developed countries. In SCH women 50% of thyroid auto antibodies and in overt hypothyroidism about 80% are detected. Hence, women with SCH mostly Thyroid peroxidase Antibodies (TPOAB) is preferred to predict the chances of thyroid autoimmunity.
A negative result for thyroid antibodies is observed after first trimester due to the immuno suppression during pregnancy. Hence, thyroid scan is recommended to detect thyroid texture in patients with increased TSH and negative thyroid antibodies.
The role of iodine in SCH: In pregnancy requirement of iodine increases about 50% which is met with dietary intake of 250 μg/day. The demand is mainly due to an elevated glomerular filtration and renal iodine clearance and transplacental iodine transfer to the fetus, during later gestational period. In chronic iodine deficient pregnant women, depletion of iodine thyroid storage leads to goitre and maternal hypothyroidism. In 2011, about 393 million (44.2%) were iodine deficient that includes pregnant and child bearing age women in Europe, SCH in Belgium and the risk is slowly increasing in high income countries.
The iodine deficiency may cause deleterious on fetal development. Hence, prophylaxis with iodine in any form will reduce mortality in infants and children with improvement in cognitive function.
According to WHO, pregnant and lactating women should be provided with 250 μg Iodine daily and is mainly achieved by supplementation of 150-250 μg potassium iodide.
Adverse effects of SCH on mother and child
Maternal effects: The hypothyroidism during pregnancy may lead to pre-eclampsia, abortion; hypertension, cretinism and death of foetus and treatment with levothyroxine may hinder these complications.
Materials and Methods
One hundred Gestational Diabetes Mothers (GDM) about 20 to 28 weeks in the antenatal clinic in the department of obstetrics and gynaecology of sree balaji medical college and hospital were selected for the present study. Institutional Ethics Committee (IEC) clearance, informed consent from participants was obtained.
Inclusion criteria: All patients diagnosed first time with abnormal glucose metabolism during pregnancy and patients willing for the study.
Exclusion criteria: Previous history of thyroid disorders, type 1 or 2 diabetes mellitus, multiple pregnancy and patients with significant illness that may contribute to glycemic and thyroid hormones level. Detailed history was taken and thorough general physical examination was done for all the cases.
Fasting blood samples were collected and stored at stored at 70°C at the laboratory for measuring FBS, thyroid profile and HbA1c. Then 2 hours Oral Glucose Challenge Test (OGCT) was done as a screening test and well diagnosed for GDM if plasma glucose values exceed; FBS->92 mg/dl, OGCT->140 mg/dl and HbA1c->5.5 and grouped as patients with elevated TSH, low levels of free thyroxin “hypothyroid”, those with elevated TSH and normal FT4 “subclinical hypothyroid”; pregnant women who had low and high TSH and FT4 “hyperthyroid”, women with low TSH and normal FT4 “subclinical hyperthyroid”. Women with normal levels of both thyrotropin and free thyroxine “Euthyroid” and then the maternal and fetal outcome were observed.
Results
The statistical analysis was carried out by IBM SPSS version 20 (Figures 1-3 and Tables 3-5).
|
Thyroid Status |
||||
|---|---|---|---|---|---|
Euthyroid |
Subclinical hypothyroidism |
P value |
|||
Mean |
SD |
Mean |
SD |
||
FBS (mg/dl) |
103.42 |
8.61 |
105.18 |
8.51 |
0.34 |
OGCT (75 mg) |
146 |
11 |
153 |
9 |
0.003 |
HbA1c (%) |
5.61 |
0.19 |
5.68 |
0.18 |
0.06 |
Table 3: Glycemic parameter in GDM cases.
|
Thyroid status |
P |
|||
|---|---|---|---|---|---|
Euthyroid |
Subclinical hypothyroidism |
||||
Mean |
SD |
Mean |
SD |
||
TSH (mU/L) |
2.048 |
0.702 |
4.603 |
0.701 |
<0.0001 |
FT4 (ng/dl) |
1.185 |
0.19 |
1.004 |
0.15 |
<0.0001 |
Table 4: Thyroid hormones level in GDM cases.
| Mode of delivery | Euthyroid | SCH | ||
|---|---|---|---|---|
| Count | Column N% | Count | Column N% | |
| Spontaneous vaginal delivery | 16 | 22.20% | 2 | 7.10% |
| Assisted VD | 12 | 16.70% | 6 | 21.40% |
| Elective CS | 12 | 16.70% | 4 | 14.30% |
| Emergency CS | 32 | 44.40% | 16 | 57.10% |
Table 5: Distribution of mode of delivery.
Discussion
In 100 cases 28% of GDM cases had subclinical hypothyroidism and 78% remain Euthyroid Table 1. The mean FBS in the pregnant euthyroid women and pregnant women with SCH was 103.40 mg/dl and 105.20 mg/dl respectively with no statistical significance (p=0.34). The mean hour OGCT in the pregnant euthyroid
women and pregnant women with SCH was 146 and 153 mg/dl respectively were statistical significance (p=0.003) Figure 1. Indicates that 28% of GDM women developed subclinical hypothyroidism during pregnancy and 72% remain euthyroid. The mean TSH in the pregnant euthyroid women and SCH was 2.04 and 4.6 mU/L respectively and was statistically significant (p=0.0001) Table 2 and Figure 2. The mean free T4 values are 1.18 and 1.00 mU/L respectively and was statistically significant (p=<0.0001) figure 3 and the he normal values of TSH and Free T4 in pregnant women are different from that of non-pregnant women. The rate of preterm delivery is elevated in GDM cases with SCH and 21% of SCH pregnant women had preterm delivery compared to 5.6% in euthyroid cases and was statistically significant (p=0.20). Table 3 shows the different mode of delivery among the study groups. The percentage of emergency C section was increased in GDM cases (57.1%) with subclinical hypothyroidism in comparison with euthyroid cases.
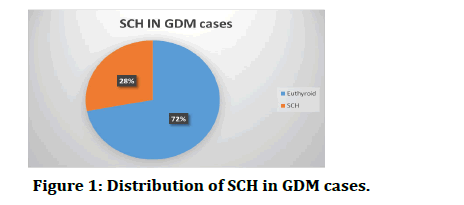
Figure 1: Distribution of SCH in GDM cases.
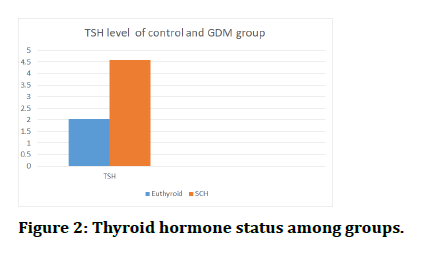
Figure 2: Thyroid hormone status among groups.
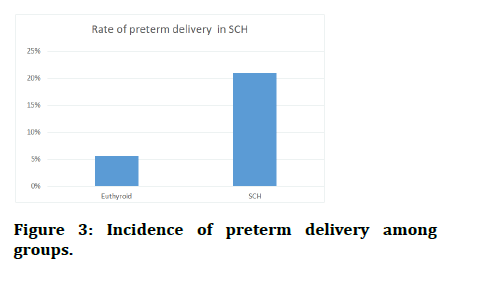
Figure 3: Incidence of preterm delivery among groups.
|
Thyroid Status |
||||
|---|---|---|---|---|---|
Euthyroid |
Subclinical hypothyroidism |
P value |
|||
Mean |
SD |
Mean |
SD |
||
FBS (mg/dl) |
103.42 |
8.61 |
105.18 |
8.51 |
0.34 |
OGCT (75 mg) |
146 |
11 |
153 |
9 |
0.003 |
HbA1c (%) |
5.61 |
0.19 |
5.68 |
0.18 |
0.06 |
Table 3: Glycemic parameter in GDM cases.
Conclusion
The goal of prenatal care is to ensure good health of mother and giving birth to a healthy baby. Carbohydrate intolerance is the most prevalent metabolic complication during pregnancy. The risk factors associated with GDM can be identified during early stage of pregnancy. The screening for GDM in women during early pregnancy tends to reduce morbidity in foetus and mother through dietary or drug management. The studies also indicate an increased risk of subclinical hypothyroidism in women with GDM and maternal thyroid hormone status was related to the degree of metabolic imbalance. Hence, it is very clear that there exists an interlink age between diabetes and thyroid disorders. This is supported by a recent meta-analysis that in 10,920 patients diagnosed with GDM had an 11% mean frequency of thyroid disease. Finally, the present study concludes that subclinical hypothyroidism and GDM are interlinked and pose an increased threat of preterm delivery. Furthermore, the study emphasizes on the importance of evaluation of thyroid function in women with GDM owing to the increase in high perinatal and neonatal morbidity.
References
- Tirosh D, Neta BT, Lena N, et al. Hypothyroidism and diabetes mellitus a risky dual gestational endocrinopathy. Peer J 2013; 43:e52.
- Langer O, Yogev Y, Most O, et al. Gestational diabetes: The consequences of not treating. Am J Obstet Gynecol 2005; 192:989-997.
- Tirosh D, Benshalom Tirosh N, Novack L, et al. Hypothyroidism and diabetes mellitus a risky dual gestational endocrinopathy. Peer j 2013; 1:e52.
- Glinoer D. The regulation of thyroid function in pregnancy: Pathways of endocrine adaptation from physiology to pathology. Endocr Rev 1997; 18:404-433.
- Feely J, Isles TE. Screening for thyroid dysfunction in diabetics. Br Med J 1979; 1:1678.
- Johnson Jl. Diabetes control in thyroid disease. Diabetes spectr 2006; 19:148-153.
- American diabetes association. Standards of medical care in diabetes-2013. Diabetes Care 2013; 36:S11-S66.
- Expert committee on the diagnosis and classification of diabetes mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes care 1997; 20:1183-1197.
- Metzger BE, Coustan DR. Summary and recommendations of the fourth international workshop conference on gestational diabetes mellitus. The organizing committee. Diabetes Care 1998; 21:B161-B167.
- Seshiah V, Balaji V, Balaji MS, et al. Gestational diabetes mellitus in India. J Assoc Physicians India 2004; 52:707-711.
- Xiang AH, Peters RK, Trigo E, et al. Multiple metabolic defects during late pregnancy in women at high risk for type 2 diabetes mellitus. Diabetes 1999; 48:848-854.
Author Info
V Sathya1, Giridharan Bupesh2 and S Vasanth1*
1Department of Research and Development wing, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chromepet, Chennai, Tamil Nadu, India2Department of Forest Science, Central University of Nagaland, Lumami, Zunhebeto, India
Citation: V Sathya, Giridharan Bupesh, S Vasanth, Incidence of Subclinical Hypothyroidism in GDM with Increased Risk of Preterm Delivery, J Res Med Dent Sci, 2022, 10 (12): 148-152.
Received: 29-Sep-2022, Manuscript No. JRMDS-22-77106; , Pre QC No. JRMDS-22-77106(PQ); Editor assigned: 03-Oct-2022, Pre QC No. JRMDS-22-77106(PQ); Reviewed: 17-Oct-2022, QC No. JRMDS-22-77106; Revised: 28-Nov-2022, Manuscript No. JRMDS-22-77106(R); Published: 05-Dec-2022
