Research - (2022) Volume 10, Issue 6
Insulin Adherence and Barriers among Patients with Diabetes in Saudi Arabia
Mohammed Saad Alqahtani*, Mohammed Mesfer Alqahtani, Talal Zaidan Alruwaili, Sultan M Alkahtani, Abdulmajeed M Alshaikhi, Abdulaziz A Basalem, Turki M Bin Saqyan, Khalid A lkhudhairi and Abdullah A Twair
*Correspondence: Mohammed Saad Alqahtani, Department of Internal Medicine, Prince Sattam Bin Abdulaziz University, Saudi Arabia, Email:
Abstract
Insulin adherence and barriers among patients with diabetes in Saudi Arabia ABSTRACT Introduction Diabetes is one of major metabolic chronic diseases that demand a continuous medical attention. Diabetes is classified generally into 2 types mainly; Type 1 Diabetes (T1DM) known to have absolute insulin deficiency which occurs due to autoimmune B-cell destruction and Type 2 Diabetes (T2DM) in which the body develops insulin resistance that occur due to the progressive loss of adequate B-cell insulin secretion. And there are other types such as Gestational and specific types which occur due to other causes. According to the World Health Organization (WHO), Saudi Arabia is the second highest country in the Middle East regarding the rate of diabetes, and ranks the seventh worldwide. Almost 3 million people of the population are pre-diabetic and 7 million are diabetic. As diabetes has a multisystem effect on general health outcome that includes macrovascular complications, such as, stroke coronary heart disease and peripheral vascular disease, and there are other microvascular complications, such, retinopathy and neuropathy, end-stage renal disease along with lower-extremity amputations. Diabetes management must be based on the pathophysiology of the disease. Therefor type 1 and type 2 diabetes may differ in their management. Insulin is an essential treatment for type 1 but type 2 is more complex, thus the treatment highly depends on individual bases and the progression of the disease. Along with an intensive non-pharmacological lifestyle modification program. Insulin regulates the metabolism of glucose in the body. Both types of diabetes can benefit from the use of exogenous insulin. There are different types of insulin based on the mode of action with different onset of action, duration and peak effect that is based on the patient needs. Therefore, insulin is commonly classified into, rapid, short, intermediate and long acting. Rapid acting insulin taken before meal " prandial or pre-bolus " and long-acting insulin last up to 24 hours and taken once to twice daily, and Premixed insulin’s (mixtures of prandial and basal insulin’s twice daily. The usual injection sites are the abdomen, front or lateral of thigh, lateral aspect of arm, and lateral upper quadrant. Rotation of injection are important. The standard route of insulin delivery is subcutaneous insulin injections. There are many ways to deliver insulin subcutaneously such as vials and syringes, insulin pens, and insulin pumps. Glucose-control highly depends on patient's adherence. However, there are many barriers that may affect adherence to the use of insulin; such as being busy, skipping meal, social distress and emotional problems. An international study done in China, France, Japan, Germany, Spain, Turkey, the UK or the USA shows (33.2%) of patients reported insulin non-adherence at least 1 day in the last month, with an average of 3.3 days. (72.5%) of physician's report that their typical patient does not take their insulin as prescribed, with a mean of 4.3 days per month of basal insulin non-adherence and 5.7 days per month of prandial insulin non-adherence and there is a local study in Saudi Arabia that included a sample size of 387, reported that the level of adherence with basal bolus insulin was 61.9%. and that there was no significant difference in the level of adherence between the two genders. With the highest adherence level being in the younger age groups (14-29). As there is insufficient local data our aim is to assess diabetic patients™ adherence and barriers to insulin therapy. Aim: This study aimed to assess diabetic patients™ adherence and barriers to insulin therapy. Patients and methods this is a cross-sectional study conducted among diabetic patients (type 1 and type 2) in Saudi Arabia. A self-administered questionnaire was distributed among the targeted patients using social media platforms. The questionnaire includes basic demographic characteristics, assessment of adherence to insulin, and assessment of barriers to insulin adherence. Results: 336 diabetic patients participated (females 75.6% vs. males 24.4%). Type 1 diabetes constituted most of the patients (92.6%) with fast-acting insulin’s being the most common insulin used (83.3%). 72.9% were worried about the occurrence of hypoglycemia events. Those who thought that insulin injections caused bruising and embarrassment were the independent significant predictors of poor insulin adherence while being married and having social or private health insurance were the independent significant predictors of good insulin adherence. Conclusion: About half of the diabetic patients were adherent to insulin therapy. Being married and having medical insurance are likely to have better adherence than the other patients while believing that insulin injections can cause bruising and embarrassment negatively affected their adherence to insulin therapeutic regimen. Keywords Diabetic patients, insulin adherence, barriers, diabetes Statistical Analysis The data were analyzed using Statistical Packages for Social Sciences (SPSS) version 26 Armonk, NY: IBM Corp. Adherence to insulin has been measured using 6 statements as illustrated in Figure 2, where a 5-point Likert scale type of categories as the answer options ranging from “always†coded as 1 to “never†coded as 5. The total adherence score had been calculated by adding all 6 items and a score range from 6 to 30 had been generated which means, the higher the score the higher adherence to insulin. By using 60% as a cutoff point to determine the level of adherence, patients were classified as poor adherence if the score was 60% or below while above 60% were classified as good adherence. Continuous variables were presented using means and standard deviations while categorical were summarized using numbers and percentages. The level of adherence was compared with the socio-demographic characteristics and the barriers toward insulin adherence by using the Chi-square test. Significant results were then placed into a multivariate regression model to determine the independent predictor associated with poor adherence where the odds ratio, as well as the 95% confidence interval, was also being reported. A p-value cut-off point of 0.05 at 95% CI was used to determine statistical significance.
Keywords
Diabetic patients, Insulin adherence, Barriers, Diabetes
Introduction
Diabetes is one of major metabolic chronic diseases that demand a continuous medical attention. Diabetes is classified generally into 2 types mainly; Type 1 Diabetes (T1DM) known to have absolute insulin deficiency which occurs due to autoimmune B-cell destruction and Type 2 Diabetes (T2DM) in which the body develops insulin resistance that occur due to the progressive loss of adequate B-cell insulin secretion and there are other types such as Gestational and specific types which occur due to other causes [1]. According to the World Health Organization (WHO), Saudi Arabia is the second highest country in the Middle East regarding the rate of diabetes, and ranks the seventh worldwide. Almost 3 million people of the population are pre-diabetic and 7 million are diabetic [2]. As diabetes has a multisystemic effect on general health outcome that includes macrovascular complications, such as, stroke coronary heart disease and peripheral vascular disease, and there are other microvascular complications, such, retinopathy and neuropathy, end-stage renal disease along with lowerextremity amputations [3] (Figure 1).
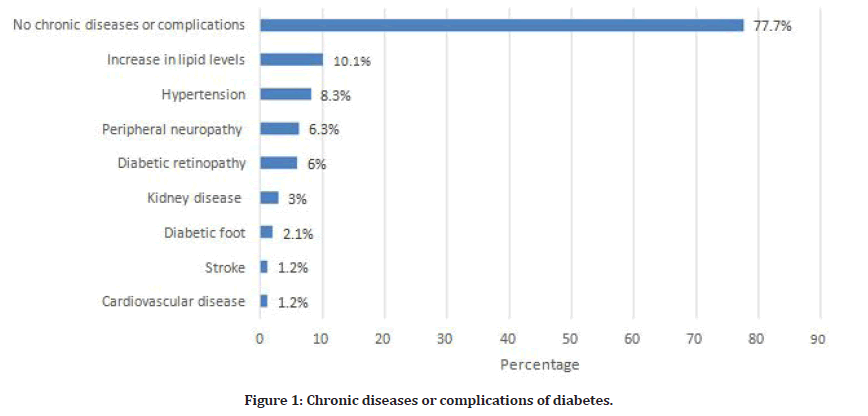
Figure 1: Chronic diseases or complications of diabetes.
Diabetes management must be based on the pathophysiology of the disease. Therefor type 1 and type 2 diabetes may differ in their management. Insulin is an essential treatment for type 1 but type 2 is more complex, thus the treatment highly depends on individual bases and the progression of the disease [4]. Along with an intensive non-pharmacological lifestyle modification program [5]. insulin regulates the metabolism of glucose in the body. both types of diabetes can benefit from the use of exogenous insulin. There are different types of insulin based on the mode of action with different onset of action, duration and peak effect that is based on the patient needs. Therefore, insulin is commonly classified into, rapid, short, intermediate and long-acting [6].
Rapid acting insulin taken before meal "prandial or pre-bolus" and long-acting insulin last up to 24 hours and taken once to twice daily, and Premixed insulin’s (mixtures of prandial and basal insulin’s twice daily. The usual injection sites are the abdomen, front or lateral of thigh, lateral aspect of arm, and lateral upper quadrant. Rotation of injection is important [7]. The standard route of insulin delivery is subcutaneous insulin injections. There are many ways to deliver insulin subcutaneously such as vials and syringes, insulin pens, and insulin pumps [8].
Glucose-control highly depends on patient's adherence. However, there are many barriers that may affect adherence to the use of insulin; such as being busy, skipping meal, social distress and emotional problems. An international study done in China, France, Japan, Germany, Spain, Turkey, the UK or the USA shows (33.2%) of patients reported insulin non-adherence at least 1 day in the last month, with an average of 3.3 days. (72.5%) of physician's report that their typical patient does not take their insulin as prescribed, with a mean of 4.3 days per month of basal insulin non-adherence and 5.7 days per month of prandial insulin non-adherence [9] and there is a local study in Saudi Arabia that included a sample size of 387, reported that the level of adherence with basal bolus insulin was 61.9%. and that there was no significant difference in the level of adherence between the two genders. With the highest adherence level being in the younger age groups (14-29) [10]. As there is insufficient local data our aim is to assess diabetic patients’ adherence and barriers to insulin therapy.
Patients and Methods
This is a cross-sectional study conducted among diabetic patients (type 1 and type 2) in Saudi Arabia. A selfadministered questionnaire was distributed among the targeted patients using social media platforms. The questionnaire includes basic demographic characteristics, assessment of adherence to insulin, and assessment of barriers to insulin adherence.
Statistical Analysis
The data were analyzed using Statistical Packages for Social Sciences (SPSS) version 26 Armonk, NY: IBM Corp. Adherence to insulin has been measured using 6 statements as illustrated in Figure 2, where a 5-point Likert scale type of categories as the answer options ranging from “always” coded as 1 to “never” coded as 5. The total adherence score had been calculated by adding all 6 items and a score range from 6 to 30 had been generated which means, the higher the score the higher adherence to insulin. By using 60% as a cutoff point to determine the level of adherence, patients were classified as poor adherence if the score was 60% or below while above 60% were classified as good adherence.
Continuous variables were presented using means and standard deviations while categorical were summarized using numbers and percentages. The level of adherence was compared with the socio-demographic characteristics and the barriers toward insulin adherence by using the Chi-square test. Significant results were then placed into a multivariate regression model to determine the independent predictor associated with poor adherence where the odds ratio, as well as the 95% confidence interval, was also being reported. A p-value cut-off point of 0.05 at 95% CI was used to determine statistical significance.
Results
336 diabetic patients responded to our survey. Table 1 presented the socio-demographic characteristics and the type of insulin used by the patients. The most common age group was 18 – 25 years (55.1%) with the majority being females (75.6%) and nearly 60% were university degree holders. Patients who were unmarried constituted 69%. Nearly 40% had been diagnosed with diabetes for more than 10 years. Type 1 diabetes constitutes most of the patients (92.6%). More than half (51.5%) had an HbA1c level of 7%-9%. Nearly all (88.7%) were using insulin pens with 83.3% were using fast-acting insulins including Aspart, glulisine, Lispiro (Novorapid, Humalog, Apidra), and long-acting (basal). Around 45.2% had an average injection per day of 3 – 4 injections.
| Study data | N (%) |
|---|---|
| Age group | |
| 18 – 25 years | 185 (55.1%) |
| 26 – 35 years | 93 (27.7%) |
| 36 – 45 years | 26 (07.7%) |
| >45 years | 32 (09.5%) |
| Gender | |
| Male | 82 (24.4%) |
| Female | 254 (75.6%) |
| Educational level | |
| High school or below | 138 (41.1%) |
| University degree | 189 (56.3%) |
| Master of Ph.D. degree | 09 (02.7%) |
| Marital status | |
| Unmarried | 232 (69.0%) |
| Married | (104) 31% |
| Time since diagnosed with diabetes | |
| <5 years ago | 123 (36.5%) |
| 5 – 10 years ago | 81 (24.1%) |
| >10 years ago | 132 (39.3%) |
| Type of diabetes | |
| Type 1 | 311 (92.6%) |
| Type 2 | 25 (7.4%) |
| HbA1c level | |
| <7% | 114 (33.9%) |
| 7%-9% | 173 (51.5%) |
| >9% | 49 (14.6%) |
| How do you use insulin? | |
| Insulin pump | 30 (8.9%) |
| Insulin pens | 298 (88.7%) |
| Withdrawal through a needle (syringe) and a vial | 8 (2.4%) |
| What type of insulin is used? | |
| Fast-acting insulins, such as Aspart, glulisine, Lispiro (Novorapid, Humalog, Apidra), and long-acting (basal) | 280 (83.3%) |
| Fast-acting insulin only, such as Aspart, Glulisine, Lispiro | 31 (9.2%) |
| Mixed insulin only, such as (Novomix) 70/30, 50/50, 25/75 | 17 (0.5%) |
| Basal insulin only, such as: glargine, glargine 300, detemir, degludec | 8 (2.4%) |
| What is the average injection per day? | |
| 1 – 2 injections | 41 (12.2%) |
| 3 – 4 injections | 152 (45.2%) |
| >4 injections | 115 (34.2%) |
| Rely on the pump | 28 (8.3%) |
Table 1: Socio-demographic characteristics and type of insulin used of diabetic patients (n=336).
The most common diabetic complication was an increase in lipid levels (10.1%) followed by hypertension (8.3%) and peripheral neuropathy (6.3%). The assessment of adherence to insulin injection has been described in Figure 2. It can be observed that 31.5% of the patients always calculate carbohydrates in food and determine the dose of insulin according to calories while only 3.9% always make plans and activities according to daily doses. About 15.8% stated that taking insulin always interferes with their physical activities while only 5.1% expressed that taking insulin always cause negative effect on social and recreational activities. Likewise, 9.9% stated that taking insulin have always cause negative effect on sex life and 3.9% expressed that taking insulin have always negative impact on work and professional development. The overall mean adherence score based on 6 statements was 19.1 (SD 4.29).
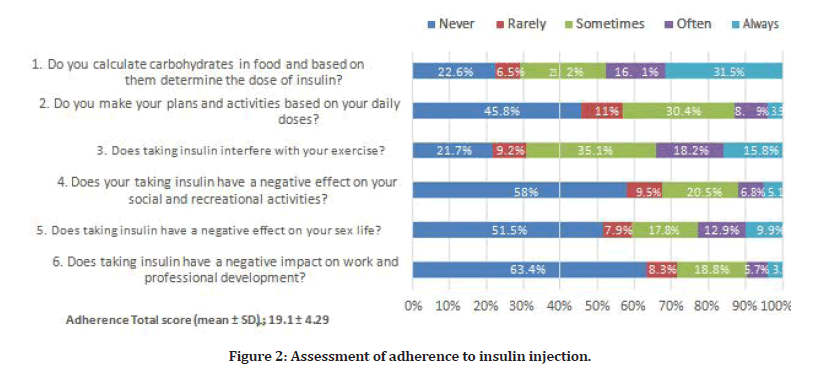
Figure 2: Assessment of adherence to insulin injection.
In Figure 3, good adherence constitutes 51% while the rest was poor (49%). In Table 2, a great proportion of patients (93.8%) knew that insulin is a necessary medication for health while 72.9% expressed worry about the occurrence of a hypoglycemic event. 64.3% believe that insulin injection causes bruising and 45.2% believe that insulin injection causes pain. Financial assistance from the family to buy insulin was declared by 39% of the patients. 29.5% believe that the injection process is the most difficult part of the treatment whereas 26.5% thought that insulin injections cause embarrassment. 22.6% declared that they have social or private medical insurance. About 20.5% were ashamed to take out the pump to take the insulin while 16.4% thought that insulin causes health problems including blindness, amputation and kidney disease. In addition, only 12.5% stopped using insulin due to financial reasons.
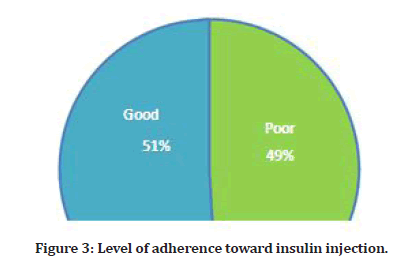
Figure 3: Level of adherence toward insulin injection.
| Statement | Yes | No |
|---|---|---|
| N (%) | N (%) | |
| Are you convinced of insulin as a necessary medication for your health? | 315 (93.8%) | 21 (06.3%) |
| Do you worry about the occurrence of a hypoglycemic episode? | 245 (72.9%) | 91 (27.1%) |
| Do insulin injections cause bruising? | 216 (64.3%) | 120 (35.7%) |
| Do insulin injections cause pain? | 152 (45.2%) | 184 (54.8%) |
| Do you receive financial support from the family to buy insulin? | 131 (39.0%) | 205 (61.0%) |
| Is the injection process the most difficult part of the treatment? | 99 (29.5%) | 237 (70.5%) |
| Do insulin injections cause embarrassment? | 89 (26.5%) | 247 (73.5%) |
| Do you have social or private health insurance? | 76 (22.6%) | 260 (77.4%) |
| Are you ashamed to take out the pump to take the insulin? | 69 (20.5%) | 267 (79.5%) |
| Do you think that insulin causes health problems, such as blindness, amputation, kidney damage? | 55 (16.4%) | 281 (83.6%) |
| Do you stop using insulin for economic reasons? | 42 (12.5%) | 294 (87.5%) |
Table 2: Assessment of barriers toward insulin adherence (n=336).
We used Chi-square test in Table 3, to determine the relationship between the level of adherence to insulin among the socio-demographic characteristics, the type of insulin used, and the barriers to insulin adherence. It was revealed that the prevalence of poor adherence was more common among the age ≤ 25 years (p=0.002), unmarried (p<0.001), type 1 diabetic patients (p=0.002), patients who thought that insulin injection caused bruising (p=0.024), can cause embarrassment (p=0.022) and those who received financial support from the family to buy insulin (p=0.017) while the prevalence of good adherence was more common among those with having social or private health insurance (p=0.015).
| Factor | Poor N (%) (n=165) | Good N (%) (n=171) |
P-value § |
|---|---|---|---|
| Age group | |||
| ≤ 25 years | 105 (63.6%) | 80 (46.8%) | 0.002 ** |
| >25 years | 60 (36.4%) | 91 (53.2%) | |
| Gender | |||
| Male | 36 (21.8%) | 46 (26.9%) | 0.278 |
| Female | 129 (78.2%) | 125 (73.1%) | |
| Educational level | |||
| High school or below | 61 (37.0%) | 77 (45.0%) | 0.133 |
| University or higher | 104 (63.0%) | 94 (55.0%) | |
| Marital status | |||
| Unmarried | 138 (83.6%) | 94 (55.0%) | <0.001 ** |
| Married | 27 (16.4%) | 77 (45.0%) | |
| Time since diagnosed with diabetes | |||
| <5 years ago | 67 (40.6%) | 56 (32.7%) | 0.29 |
| 5–10 years ago | 39 (23.6%) | 42 (24.6%) | |
| >10 years ago | 59 (35.8%) | 73 (42.7%) | |
| Type of diabetes | |||
| Type 1 | 160 (97.0%) | 151 (88.3%) | 0.002 ** |
| Type 2 | 05 (03.0%) | 20 (11.7%) | |
| HbA1c level | |||
| <7% | 65 (39.4%) | 49 (28.7%) | 0.11 |
| 7%-9% | 77 (46.7%) | 96 (56.1%) | |
| >9% | 23 (13.9%) | 26 (15.2%) | |
| Chronic disease or diabetic complication | |||
| Yes | 32 (19.4%) | 43 (25.1%) | 0.206 |
| No | 133 (80.6%) | 128 (74.9%) | |
| Barriers toward insulin injection * | |||
| Injection process is the most difficult part of the treatment | 51 (30.9%) | 48 (28.1%) | 0.568 |
| Ashamed to take out the pump to take the insulin | 36 (21.8%) | 33 (19.3%) | 0.568 |
| Insulin injections caused pain | 78 (47.3%) | 74 (43.3%) | 0.462 |
| Insulin injections caused bruising | 116 (70.3%) | 100 (58.5%) | 0.024 ** |
| Insulin injections caused embarrassment | 53 (32.1%) | 36 (21.1%) | 0.022 ** |
| Worried about the occurrence of a hypoglycemic episode | 126 (76.4%) | 119 (69.6%) | 0.163 |
| Stopped using insulin for economic reasons | 25 (15.2%) | 17 (09.9%) | 0.149 |
| Received financial support from the family to buy insulin | 75 (45.5%) | 56 (32.7%) | 0.017 ** |
| Having social or private health insurance | 28 (17.0%) | 48 (28.1%) | 0.015 ** |
| Convinced of insulin as a necessary medication | 157 (95.2%) | 158 (92.4%) | 0.297 |
| Thought insulin causes health problems | 23 (13.9%) | 32 (18.7%) | 0.237 |
| *Variable with multiple responses. | |||
| § P-value has been calculated using Chi-square test. | |||
| **Significant at p<0.05 level. | |||
Table 3: Relationship between adherence to insulin among the socio-demographic characteristics, type of insulin used and the barriers to insulin adherence of diabetic patients (n=336).
In a multivariate regression model, married patients were significantly more likely to be associated with good insulin adherence (AOR=0.200; 95% CI=0.100–0.397; p<0.001). Patients who thought that insulin injection can cause bruising were 1.8 times higher of having poor insulin adherence (AOR=1.798; 95% CI=1.084–2.985; p=0.023). Patients who thought that insulin injection can cause embarrassment were 2.2 times higher of having poor insulin adherence (AOR=2.195; 95% CI=1.261-3.820; p=0.005). On the other hand, patients with having social or private medical insurance were significantly more likely to being associated with good insulin adherence (AOR=0.502; 95% CI=0.280–0.900; p=0.021) while age group and the type of diabetes did not significantly influence the level of adherence after adjustments to regression model (Table 4).
| Factor | AOR | 95% CI | P-value |
|---|---|---|---|
| Age group | |||
| ≤ 25 years | Ref | ||
| >25 years | 1.225 | 0.680 – 2.206 | 0.499 |
| Marital status | |||
| Unmarried | Ref | ||
| Married | 0.2 | 0.100 – 0.397 | <0.001** |
| Type of diabetes | |||
| Type 1 | Ref | ||
| Type 2 | 0.477 | 0.151 – 1.507 | 0.207 |
| Barriers toward insulin injection* | |||
| Insulin injections caused bruising | 1.798 | 1.084 – 2.985 | 0.023** |
| Insulin injections caused embarrassment | 2.195 | 1.261 – 3.820 | 0.005** |
| Received financial support from the family to buy insulin | 1.553 | 0.963 – 2.504 | 0.071 |
| Having social or private health insurance | 0.502 | 0.280 – 0.900 | 0.021** |
| AOR – Adjusted Odds Ratio; CI – Confidence Interval. | |||
| *Variable with multiple responses. | |||
| **Significant at p<0.05 level. | |||
Table 4: Multivariate regression analysis to determine the independent significant factor associated with poor insulin adherence (n=336).
Discussion
This study is carried out to determine the insulin adherence and barriers of the patients with diabetes. The findings of this study revealed that more than half (51%) had good adherence to insulin regimens and the rest were poor (49%). These findings are strikingly similar to the study of Almeda-Valdes et al. [11] accordingly, they found out that 49.1% of the diabetic patients were nonadherent to insulin therapy while 50.9% were adherent. Similarly, Alsayed et al. [10] documented that 61.9% of the patients were in adherence to basal-bolus insulin therapy. In a multinational study conducted by Peyrot et al. [9] they reported that 33.2% of the diabetic patients were non-adherent to basal insulin therapy for at least 1 day during the previous month with an average of 3.3 days, however, they raised a concern about glucose control as it is insufficient among insulin-treated patients which could be due to insulin omission and the deficiency of dose adjustment. Another published study conducted by Abdu El-Aal et al. [12] indicated that fair adherent to diabetic diet was found in more than half of the patients and more than two-third had adequate adherent to medication. Incidentally in Sri Lanka [13], adherence among diabetic patients was lacking, only 42.5% of the patients were following insulin regimens and 57.5% were non-adherence. The author further explained that adherence to insulin therapy is less due to a gap in patients’ awareness. Poor adherence to insulin therapy had also been reported by Mariye et al. [14] They explained that the disparities with adherence could be due to lifestyle, sample size, time gap and utilization of health service.
Alsayed et al. [10] found out that age and a higher level of education have a positive relationship with adherence which were consistent with the paper of Abdu El-Aal et al. [12] as well as Weerakoon et al. [13] In our study, age was a factor of adherence to insulin where younger age group (age ≤25 years) exhibited poor adherence, however, the level of adherence between high school or below and university or higher degree were not significantly different which did not coincide with previous reports. We also found out that being
married and having social or private health insurance were the predictors of good adherence while believing insulin injections can cause embarrassment and bruising were both predictors of poor adherence, however, the occurrence of a hypoglycemic episode and stopping insulin due to economic reasons were not the relevant factors of adherence. These findings are not in accordance with the paper of Almeda-Valdes et al. [11] according to their reports, insulin non-adherence was significantly associated with fear of hypoglycemia and economic reasons. Another study conducted by Mariye et al. [14] noted that good knowledge and favorable attitude toward insulin injection, free-cost insulin therapy, and having a glucometer at home were found to be significant predictors of adherence to insulin therapy. They emphasized that access to free-cost insulin therapy may be related to a poor economic status which shows a challenge among diabetic patients.
Even though most of the patients do not have private health insurance (77.4%), which is necessary for continuing medication? Albeit, this did not pose a barrier among the patients. About 87.5% of the patients would still continue insulin regimen even with economic concerns and while 93.8% saw insulin as a necessary medication to improve health, however, most of the patients have concerns with hypoglycemic events with nearly two-thirds (64.3%) worried about insulin injections that can cause bruising or pain (45.2%). On the other hand, many of them (83.6%) did not seem to agree that insulin causes health problems including blindness, amputation and kidney damage. In a multinational study conducted by Peyrot et al. [9] they found out that many patients treated with insulin do have sufficient glucose control (87.6%) and that they would treat more assertively if not for concerns about hypoglycemia, concluding that the majority of patients see insulin treatment as having positive than negative impact on their lives. In a qualitative study of Mirahmadizadeh et al. [15] they learned that lack of trust in the medical team and each patient’s unique experiences and challenges in everyday life are the barriers to adherence to treatment in patients with type 2 diabetes. Diabetic complications could also influence insulin adherence. In this study, 23.3% of the patients were having associated complications including an increase in lipid levels, hypertension and peripheral neuropathy. In Makkah, Saudi Arabia [16], a higher proportion (57.9%) of diabetic patients had complications with acidosis as the most common complication. In Riyadh, Saudi Arabia [9], hypercholesteremia (51.6%) and hypertension (40.8%) were the most common complication of diabetes which were not consistent with our reports.
It is important to note that insulin pen was the most commonly used insulin (88.7%) and fast-acting insulins such as Aspart, glulisine, Lispiro (Novorapid, Humalog, Apidra), and long-acting (basal) was the most commonly used type (83.3%) with 3–4 injections per day (45.2%). This is consistent with the paper of Alsayet et al. [10], based on their account, 39.8% of the patients had 4 daily injections and 61.9% had never missed this routine while in a paper published by Alhazmi et al. [16], 30.7% of the patients had once or twice (30%) insulin injections per day.
Conclusion
About half of the diabetic patients were adherent to insulin therapy. Being married and having medical insurance are likely to have better adherence than the other patients while believing that insulin injections can cause bruising and embarrassment negatively affected their adherence to insulin therapeutic regimen. The education and positive perception about insulin are necessary to adherence, apart from these, they need continuous counseling and monitoring as the disease might cause a psychological effect that is detrimental to their health condition. A regular visit to the diabetic clinic is equally important to make sure that the insulin regimens are effective and that patient has a good perception of it. Addressing the concerns of patients along with appropriate counseling could definitely improve patients’ adherence to insulin regimens.
Availability of Data and Materials
The dataset generated and analysed to support this study's findings was present within the study results.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-forprofit sectors.
Author’s contribution
All authors contributed equally to data collection, writing and analyzing the results. The final draft of the manuscript has been approved by all authors.
Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This publication was supported by the Deanship of Scientific Research, Prince Sattam bin Abdulaziz University, Al-Kharj, Saudi Arabia.
References
- American Diabetes Association. Classification and diagnosis of diabetes: Standards of Medical care in diabetes-2020. Diabetes Care 2020; 43:S14-31.
- Al Dawish MA, Robert AA, Braham R, et al. Diabetes mellitus in Saudi Arabia: A review of the recent literature.Curr Diabetes Rev 2016; 12:359-368.
- www.IDF.org/our-activities/care-prevention/ cardiovascular-disease/cvd-report. Accessed 24 July 2018. https://www.idf.org/our-activities/care-prevention/cardiovascular-disease/cvd-report
- Simó R, Hernández C. Treatment of diabetes mellitus: general goals, and clinical practice management. Rev Esp Cardiol 2002; 55:845-860.
- Johnson EL, Feldman H, Butts A, et al. Standards of medical care in diabetes—2020 abridged for primary care providers. Clin Diabetes 2020; 38:10-38.
- Ahmad K. Insulin sources and types: A review of insulin in terms of its mode on diabetes mellitus. J Tradit Chin Med 2014; 34:234-237.
- Danne T, Phillip M, Buckingham BA, et al. ISPAD Clinical practice consensus guidelines 2018: Insulin treatment in children and adolescents with diabetes. Pediatr Diabetes 2018; 19:115-135.
- Shah RB, Patel M, Maahs DM, et al. Insulin delivery methods: Past, present and future. Int J Pharm Investig 2016; 6:1-9.
- Peyrot M, Barnett AH, Meneghini LF, et al. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabet Med 2012; 29:682-689.
- Alsayed KA, Ghoraba MK. Assessment of diabetic patients' adherence to insulin injections on basal-bolus regimen in diabetic care center in Saudi Arabia 2018: Cross sectional survey. J Family Med Prim Care 2019; 8:1964-1970.
- Almeda-Valdes P, Ríofrio JP, Coronado KW, et al. Factors associated with insulin nonadherence in type 1 diabetes mellitus patients in mexico. Int J Diabetes Metabol 2019; 25:139.
- Abdu EL-Aal HE, Mohamed MA, Saad AY. Adherence of patients with insulin-dependent diabetes to therapeutic regimen. Egyptian J Hospital Med 2019; 77:5784-94.
- Weerakoon LN, Amarasekara TD, Jayasekara R. Factors affecting adherence to insulin therapy among patients with type 2 diabetes mellitus in a selected teaching hospital, Sri Lanka. Biomed J Scien Tech Res 2020; 30:23608.
- Mariye T, Girmay A, Birhanu T, et al. Adherence to insulin therapy and associated factors among patients with diabetes mellitus in public hospitals of Central Zone of Tigray, Ethiopia, 2018: A cross-sectional study. Pan African Med J 2019; 33.
- Mirahmadizadeh A, Delam H, Seif M, et al. Factors affecting insulin compliance in patients 6with type 2 diabetes in South Iran, 2017: We are faced with insulin phobia. Iranian J Med Sci 2019; 44:204.
- Alhazmi GA, Balubaid RN, Sajiny S, et al. Assessment of insulin injection technique among diabetic patients in Makkah region in Saudi Arabia. Cureus 2020; 12.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Mohammed Saad Alqahtani*, Mohammed Mesfer Alqahtani, Talal Zaidan Alruwaili, Sultan M Alkahtani, Abdulmajeed M Alshaikhi, Abdulaziz A Basalem, Turki M Bin Saqyan, Khalid A lkhudhairi and Abdullah A Twair
Department of Internal Medicine, Prince Sattam Bin Abdulaziz University, Saudi ArabiaCitation: Mohammed Saad Alqahtani, Mohammed Mesfer Alqahtani, Talal Zaidan Alruwaili, Sultan M Alkahtani, Abdulmajeed M Alshaikhi, Abdulaziz A Basalem, Turki M Bin Saqyan, Khalid A lkhudhairi, Abdullah A Twair,, Insulin Adherence and Barriers among Patients with Diabetes in Saudi Arabia, J Res Med Dent Sci, 2022, 10 (6):01-08.
Received: 18-May-2022, Manuscript No. JRMDS-22-64103; , Pre QC No. JRMDS-22-64103 (PQ); Editor assigned: 20-May-2022, Pre QC No. JRMDS-22-64103 (PQ); Reviewed: 03-Jun-2022, QC No. JRMDS-22-64103; Revised: 06-Jun-2022, Manuscript No. JRMDS-22-64103 (R); Published: 13-Jun-2022
