Research - (2020) Volume 8, Issue 3
Lower Incisor Inclination and Bony Support in Class II Skeletal Pattern Patients-CBCT Study
Murshida Marizan Nor1*, Marhamah Manan2, Alizae Marny Mohamed1, Tanti Irawati Rosli1 and Azrul Hafiz3
*Correspondence: Murshida Marizan Nor, Faculty of Dentistry, Universiti Kebangsaan Malaysia, Jalan Raja Muda Abdul Aziz, Kuala Lumpur, Malaysia, Email:
Abstract
Aim: To Identify the dentoalveolar morphology features in relation to different inclination of the mandibular incisors in Class II skeletal pattern patients using a dental cone-beam computed tomography (CBCT).
Materials and methods: A total of 180 CBCT records were collected from subjects aged between 17 to 35 years old. The subjects were classified into its incisor inclination (procline: 91 subjects and upright: 88 subjects) according to the cephalometrics norms. The buccolingual thickness and alveolar bone height of the mandibular incisors were measured using iCAT Vision Software Interface.
Results: The upright group had significantly greater alveolar bone height compared to the proclined group (P<0.05). The alveolar bone thickness was significantly thicker at 9.13 ± 2.14mm in proclined mandibular incisors compared to the upright group 7.97 ± 1.78 mm (P<0.05). The lingual alveolar bone was significantly thicker at the mandibular lateral incisors than central incisors in both upright and proclined group. The inclination of the lower incisors has negative correlation with total bone height at the central incisors. Significant association observed between incisor inclination with the total bone thickness and labial part of total bone thickness.
Conclusion: There is a significant relationship between lower incisors inclination with alveolar bone height and thickness surrounding the mandibular symphysis.
Keywords
Incisor inclination, Alveolar morphology, Bony support, CBCT
Introduction
Successful orthodontic treatment is dependent on the detailed evaluation of treatment outcomes. The position of the lower incisors in relation to their supporting bone is an important factor in orthodontic diagnosis, treatment plan, mechanics as well as its treatment outcome. Previous studies stated that the anteroposterior thickness of the alveolar bone in the symphysis region determines the amount of orthodontic tooth movement determines the distance available for orthodontic movement of the incisors. Challenging these limits may cause undesirable effects to the periodontal tissues such as severe root resorption and bony dehiscence [1].
Treatment of Class II division 1 malocclusion includes growth modification, dental camouflage and orthognatic surgery. However, excessive proclination of the mandibular incisors can occur when camouflaging these cases. The increased usage of self-ligating system which advocates non extraction treatment also produces excessive proclination of the lower incisors. Such mechanics, depending on type and amount of tooth movement as well as its morphology of alveolar bone can decentralize teeth from the alveolar bone envelope, causing fenestrations and gingival recession, bone dehiscence [2-4]. In addition, orthodontic forces applied can increase tissue strain, hence causing reduced keratinized gingiva thickness and gingival recession [5].
Few studies have reported differences in alveolar bone height and thickness in different facial types. Gracco, et al. [6] reported that the longfaced subjects had reduced total thickness of the mandibular symphysis than short-face subjects. In addition, long face type patients had a thinner alveolar ridge and mandibular symphysis [6-8].
Yu, et al. [9] concluded that labio/lingual incisor inclination can affect the morphology of the alveolar crest in the lower central incisor. This occurs because in a labially inclined lower central incisor, the root apex was closer to the lingual alveolar crest. The inclination of the central incisor significantly associated with the labiolingual inclination of its alveolar bone and reduced labiolingual size of the alveolar process indicates that the bone supporting the mandibular incisors is thin. Hence it has higher chances of sustaining iatrogenic damage [2].
Placement of orthodontic miniscrew in the lower anterior region facilitates correction of overbite [10-12]. The stability of the orthodontic miniscrew is dependent largely on cortical bone thickness, density and height as well as miniscrew length and diameter. Thicker bone allows better primary stability [10]. Hence, detailed alveolar bone morphology in relation to incisors is important in reducing its failure rate and risk of damaging anatomical tissue.
CBCT provides radiographic images in multiple slices as well as 3D volumetric images, free from distortion. This enabled accurate display of the vertical and buccal-lingual dimensions of the mandible in actual size [13]. The accuracy of measurements taken on a CBCT image is acceptable where it is within maximum deviation of 0.3mm and a mean deviation of 0.13 ± 0.09 mm.
Majority of studies reported the differences of alveolar bony support and morphology of symphysis according to different facial types [8,14,15]. In addition, the association of mandibular anterior bony support with incisor crowding and the relationship between vertical facial morphology and overjet in class II subjects have also been studied [16,17]. However, to date, there is a paucity of literature on dentoalveolar morphology surrounding each of the lower incisors of different incisor inclination. Therefore, this study aims to identify the dentoalveolar morphology features and its influence on different inclination of the lower incisors in Class II skeletal pattern patients using a dental cone-beam computed tomography.
Materials and Methods
This was a cross-sectional study where conebeam computed tomography (CBCT) was taken on patients who seek orthodontic treatment in Dental Faculty, Universiti Kebangsaan Malaysia (UKM). Ethical approval was obtained from the Ethics Committee of Universiti Kebangsaan Malaysia Medical Centre UKM, UKM 1.5.3.5/244/ DD/2012/020 (2). All CBCT examinations were performed due to clinical indications and not for the purpose of this study. Informed consent was obtained prior taking the CBCT. The inclusion criteria were class II skeletal pattern patients with ANB of >5° and lower face height of <31°, mild or no crowding, age over 18 years, no history of previous orthodontic treatment and generally acceptable oral hygiene and periodontal condition. Subjects with craniofacial malformations, increased lower face height, missing lower incisors, evidence of previous trauma, extraction, prosthesis, endodontic treatment and surgery to the stomatognathic apparatus were all excluded from this study. A total sample of 179 CBCT scans from subjects aged between 18 and 35 years (mean age of 27.45 years) who were treated at the Dental Faculty of UKM was selected.
All CBCT were obtained using iCAT® Imaging System (Hatfield, USA), and following these exposure parameters: 120 kV, 5 mA, exposure time between 6 and 6 s and voxel size 0.3mm. ICAT vision Then, the lateral cephalometric image obtained from ICAT Vision Software was exported into Vistadent OC Orthodontic imaging program for cephalometric analysis. The subjects were then classified into two groups based on its incisor inclination 1:>99° (procline), 2: 87°-99° (upright) [18,19]. The buccolingual thickness and alveolar bone height of each lower incisor obtained from the slices were measured using iCATVisionQ software which allowed linear measurement of all image views. For this study, sagittal sections which passed through the central root canal of the lower incisors were measured and analyzed. Table 1 and Figure 1 shows the reference lines used to measure each section.
| Sections | Definition |
|---|---|
| Total alveolar bone height | From prosthion to the external surface of the lingual cortex, parallel to the axis of the incisor |
| Cancellous bone height | From labial to the lingual cortex of the symphysis, parallel to the long axis of the incisor |
| Total bone thickness | Segment from external surfaces of labial to the lingual cortex, passes the apices of the root and perpendicular to the long axis of the incisor, which is further divided to labial and lingual segment |
| Cancellous bone thickness | Segment from internal surfaces of the labial to lingual cortex, passes the apices of the root and perpendicular to the long axis of the incisor, which is further divided to labial and lingual segment |
Table 1: Reference lines used in measurements.
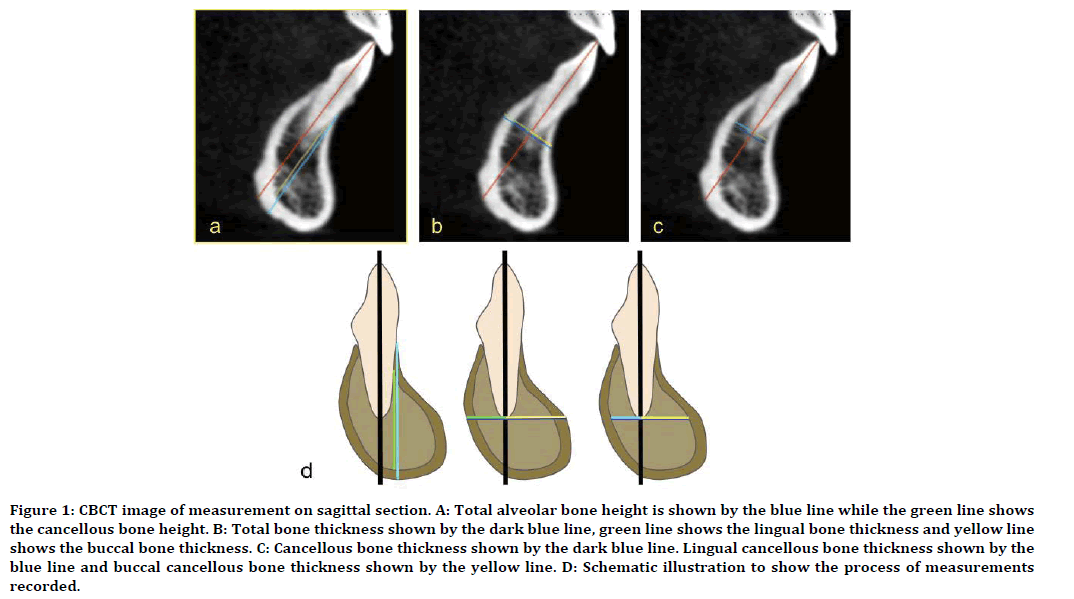
Figure 1. CBCT image of measurement on sagittal section. A: Total alveolar bone height is shown by the blue line while the green line shows the cancellous bone height. B: Total bone thickness shown by the dark blue line, green line shows the lingual bone thickness and yellow line shows the buccal bone thickness. C: Cancellous bone thickness shown by the dark blue line. Lingual cancellous bone thickness shown by the blue line and buccal cancellous bone thickness shown by the yellow line. D: Schematic illustration to show the process of measurements recorded.
For accurate CBCT measurements, intraexaminer test was carried prior to actual measurements, where 20 randomly selected cases were re-measured at one week apart. The results of an ICC>0.9 indicated an excellent agreement. Sample size calculation was done, and the power analysis predicted an N=64 for those groups that were statistically different. There were 88 subjects in the first group and 91 in the second group, providing enough subjects for this study. Data were analyzed using Statistical Package for Social Science 22 (SPSS Inc., Chicago, IL, USA). Student’s t-test and ANOVA were used to compare bone morphology between procline and upright lower incisors. Pearson’s correlation coefficient was used for correlation of bone morphology with different inclination of lower.
Results
More than two hundred patients were approached however consent was only obtained from 179 participants with an age range from 16 to 35 years old. The subjects consisted of 65 (36.3%) males and 114 (63.6%) females. Majority of the participants were Malays 130 (72.6%), followed by Chinese 41 (22.9%), Indians 7 (3.3%) and other ethnic 2 (1.1%) groups, respectively.
Table 2 shows the distribution of 179 subjects according to their gender and ethnic group in relation to different inclination of incisors. Generally, more females have proclined mandibular incisor (73.6%) compared to males but there was no significant association between gender and incisor inclination. When looking at different ethnicity, 78% of Malay has proclined mandibular incisor compared to 17.6% of Chinese and 1.1% of Indians. Nevertheless, there was also no association between the ethnic group and incisor inclination. In this study, Eastmen Analysis was used to subdivide the inclination of lower incisors because it is the most commonly used analysis in Malaysia for orthodontic treatment planning. The total alveolar bone height was significantly greater in upright lower incisors (ranged between 29.28±4.93 to 29.83 ± 4.96 mm) compared to proclined incisors (ranged between 27.53 ± 5.15-26.61 ± 5.13 mm) (P<0.001). The cancellous bone heights were also greater in upright lower incisors (Table 3).
| Upright Group (%) | Proclined Group (%) | p-value | ||
|---|---|---|---|---|
| Gender | Male | 41 (46.6) | 24 (26.4) | 0.06 |
| Female | 47 (53.4) | 67 (73.6) | ||
| Total | 88 | 91 | ||
| Ethnic group | Malay | 59 (67.0) | 71 (78.0) | 0.386 |
| Chinese | 25 (28.4) | 16 (17.6) | ||
| Indian | 3 (3.4) | 3 (3.3) | ||
| Others | 1 (1.1) | 1 (1.1) | ||
| Total | 88 | 91 |
Table 2: Distribution of subjects within gender and ethnic group with incisor inclination.
| Tooth | Upright | Procline | |
|---|---|---|---|
| Total alveolar bone height (mm) | 31 | 29.28 (4.93) | 26.61 (5.13) |
| 41 | 29.83 (4.96) | 27.12 (5.26) | |
| 32 | 29.36 (5.55) | 27.51 (4.97) | |
| 42 | 29.49 (5.38) | 27.53 (5.15) | |
| Cancellous bone height (mm) | 31 | 17.80 (5.31) | 15.59 (4.15) |
| 41 | 17.57 (5.48) | 15.90 (4.01) | |
| 32 | 16.78 (5.92) | 15.49 (4.45) | |
| 42 | 16.54 (5.55) | 15.77 (4.75) |
Table 3: Comparison of alveolar bone height between upright and proclined group.
For alveolar bone thickness, a trend can be seen in which proclined incisors have greater alveolar bone thickness at all sites. The total alveolar bone and cancellous bone thickness were significantly greater in proclined lower incisors compared to the upright incisors (P<0.001). Similar findings were observed in the alveolar bone, labial to the lower incisors. The total labial bone and labial cancellous bone thickness were also significantly greater in proclined lower incisors (P<0.001). However, there was no significant difference in the total lingual bone and lingual cancellous bone thickness between both groups. In upright lower incisors, total lingual bone thickness is greater (4.17 ± 1.25 to 4.80 ± 1.33 mm) than total labial bone thickness (3.46 ± 1.17 to 3.73 ± 1.15 mm). The total labial bone thickness surrounding proclined lower incisors was like the total lingual bone thickness. The total lingual and lingual cancellous bone was similar in both groups (Table 4).
| Tooth | Upright | Procline | p-value | |
|---|---|---|---|---|
| Total bone thickness (mm) | 31 | 7.97 (1.78) | 9.13 (2.14) | 0.001* |
| 41 | 7.95 (1.74) | 8.94 (1.84) | 0.001* | |
| 32 | 8.23 (1.75) | 9.53 (2.11) | 0.001* | |
| 42 | 8.25 (1.85) | 9.29 (1.96) | 0.001* | |
| Cancellous bone thickness (mm) | 31 | 4.43 (1.44) | 5.31 (1.68) | 0.001* |
| 41 | 4.45 (1.41) | 5.17 (1.41) | 0.001* | |
| 32 | 4.28 (1.55) | 5.26 (1.61) | 0.001* | |
| 42 | 4.28 (1.62) | 5.22 (1.77) | 0.001* | |
| Total labial bone thickness (mm) | 31 | 3.73 (1.15) | 4.75 (1.75) | 0.001* |
| 41 | 3.46 (1.17) | 4.42 (1.52) | 0.001* | |
| 32 | 3.70 (1.21) | 4.73 (1.56) | 0.001* | |
| 42 | 3.48 (1.34) | 4.31 (1.52) | 0.001* | |
| Labial Cancellous bone thickness (mm) | 31 | 2.32 (1.03) | 3.01 (1.38) | 0.001* |
| 41 | 2.04 (0.92) | 2.80 (1.22) | 0.001* | |
| 32 | 2.16 (1.14) | 2.32 (0.92) | 0.001* | |
| 42 | 1.95 (1.05) | 2.67 (1.39) | 0.001* | |
| Total lingual bone thickness (mm) | 31 | 4.17 (1.25) | 4.37 (1.14) | NS |
| 41 | 4.50 (1.25) | 4.50 (1.10) | NS | |
| 32 | 4.44 (1.28) | 4.76 (1.160 | NS | |
| 42 | 4.80 (1.33) | 4.92 (1.43) | NS | |
| Lingual Cancellous bone thickness (mm) | 31 | 2.08 (1.04) | 2.2790.93) | NS |
| 41 | 2.37 (1.09) | 2.29 (0.99) | NS | |
| 32 | 2.11 (1.14) | 2.23 (0.92) | NS | |
| 42 | 2.42 (1.11) | 2.59 (1.28) | NS |
Table 4: Comparison of alveolar thickness between upright and proclined group.
When comparing the alveolar bone height and alveolar bone thickness between all the mandibular incisors, proclined mandibular incisors had similar alveolar bone height. In addition, the alveolar bone thickness surrounding the mandibular incisor in this group showed no significant difference between the teeth. However, mandibular right lateral incisor (42) had significantly greater lingual alveolar bone thickness compared to the other teeth (P<0.05). All upright lower incisors have similar total alveolar and cancellous bone height (P>0.05). Similarly, there was no significant difference in the alveolar bone thickness of all lower incisors. However, the mandibular right lateral incisor (42) had significantly greater lingual bone thickness compared to the other teeth (P<0.05) (Table 5).
| Category | 31 | 32 | 41 | 42 | p-value | |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Proclined Lower Incisor Group | Total alveolar bone height (mm) | 26.61 (5.13) | 27.51 (4.97) | 27.12 (5.26) | 27.53 (5.15) | NS |
| Cancellous bone height (mm) | 15.59 (4.15) | 15.49 (4.45) | 15.90 (4.01) | 15.77 (4.75) | NS | |
| Total bone thickness (mm) | 9.13 (2.14) | 9.53 (2.10) | 8.94 (1.84) | 9.29 (1.96) | NS | |
| Labial part (mm) | 4.75 (1.75) | 4.73 (1.56) | 4.42 (1.52) | 4.31 (1.52) | NS | |
| Lingual part (mm) | 4.37 (1.14) | 4.76 (1.16) | 4.50 (1.10) | 4.92 (1.43) | 0.03* | |
| Cancellous bone thickness (mm) | 5.31 (1.68) | 5.26 (1.61) | 5.17 (1.41) | 5.22 (1.77) | NS | |
| Labial part (mm) | 3.01 (1.38) | 2.91 (1.24) | 2.80 (1.22) | 2.67 (1.39) | NS | |
| Lingual part (mm) | 2.27 (0.93) | 2.32 (0.92) | 2.29 (0.99) | 2.59 (1.28) | NS | |
| Upright Lower Incisor Group | Total alveolar bone height (mm) | 29.28 (4.93) | 29.36 (5.55) | 29.83 (4.96) | 29.49 (5.38) | NS |
| Cancellous bone height (mm) | 17.80 (5.31) | 16.78 (5.92) | 17.57 (5.48) | 16.54 (5.55) | NS | |
| Total bone thickness (mm) | 7.97 (1.78) | 8.23 (1.75) | 7.95 (1.74) | 8.25 (1.85) | NS | |
| Labial part (mm) | 3.73 (1.15) | 3.70 (1.21) | 3.46 (1.17) | 3.48 (1.34) | NS | |
| Lingual part (mm) | 4.17 (1.25) | 4.44 (1.28) | 4.50 (1.25) | 4.80 (1.33) | 0.03** | |
| Cancellous bone thickness (mm) | 4.43 (1.44) | 4.28 (1.55) | 4.45 (1.41) | 4.28 (1.62) | NS | |
| Labial part (mm) | 2.32 (1.03) | 2.16 (1.18) | 2.04 (0.92) | 1.95 (1.05) | NS | |
| Lingual part (mm) | 2.08 (1.04) | 2.11 (1.14) | 2.37 (1.09) | 2.42 (1.11) | NS |
Table 5: Comparison of all 4 mandibular incisors in proclined and upright group.
There was a significant correlation between inclination of the lower incisors with alveolar bone height, where the alveolar bone height increased with reduced inclination of lower incisors. There was also a correlation between incisor inclination with alveolar bone thickness. A positive correlation existed between total and labial labial bone thickness with incisor inclination. The total and labial labial bone thickness was greater in proclined lower incisors. No relationship was observed between incisor inclination and lingual bone thickness (Table 6).
| 31 | 32 | 41 | 42 | |||||
|---|---|---|---|---|---|---|---|---|
| r | p-value | r | p-value | r | p-value | r | p-value | |
| Total alveolar bone height | -0.236 | 0.001** | -0.114 | 0.128 | -0.221 | 0.003** | -0.109 | 0.147 |
| Cancellous bone height | -0.156 | 0.037* | -0.082 | 0.273 | -0.124 | 0.097 | -0.039 | 0.604 |
| Total bone thickness | 0.325 | 0.001** | 0.355 | 0.001** | 0.309 | 0.001** | 0.277 | 0.001** |
| Labial part | 0.359 | 0.001** | 0.353 | 0.001** | 0.39 | 0.001** | 0.278 | 0.001** |
| Lingual part | 0.118 | 0.116 | 0.194 | 0.009* | 0.015 | 0.847 | 0.07 | 0.349 |
| Cancellous bone thickness | 0.338 | 0.001** | 0.362 | 0.001** | 0.326 | 0.001** | 0.327 | 0.001** |
| Labial part | 0.335 | 0.001** | 0.302 | 0.001** | 0.36 | 0.001** | 0.288 | 0.001** |
| Lingual part | 0.12 | 0.108 | 0.193 | 0.010* | 0.041 | 0.584 | 0.16 | 0.032 |
Table 6: Correlation between incisor inclination and mandibular incisor bony support.
Discussion
CBCT has an advantage of no image magnification or distortion. According to Romero-Delmastro, et al. [20], the mean error of linear measurement in CBCT is 0.1mm-0.2mm. It is also most precise in the middle of the volume and increases towards the edge, while image distortion in panoramic can go up to 20%. CBCT has sensitivity and specificity of up to 90% in detecting fenestrations and 95% specificity as well as 40% in detecting dehiscence [21]. Therefore, CBCT has enabled us to identify alveolar bone surrounding all four lower incisors which wasn’t possible previously with lateral cephalogram.
The existing literature mostly describes CBCT analysis of the maxillary vestibular cortex with few studies reporting the morphology of the mandibular alveolar bone in association to different inclination. To the best of our knowledge, there are few publications reporting on analysis of both labial and lingual mandibular bone surrounding all four lower incisors.
A thorough assessment of alveolar bone surrounding lower incisors can help orthodontic diagnosis and improve outcome. Labiolingual as well as extrusion and intrusive movement of the lower incisors to improve sagittal and vertical relationship is mandatory to achieve a more harmonious profile. The inclination of the lower incisor is greatly influenced by the amount of proclination or retroclination of the lower incisors. If incisor root apex is moved against the cortical plate of the alveolus, severe root resorption and bony dehiscence can occur [18]. Hence, the decision as to how much we can move the lower incisors and how the bone may be affected is critical during an orthodontic treatment plan.
There were no significant differences in the incidence of upright or proclined upper and lower incisors in male or female subjects, which is similar to previous study [22]. In addition, there was also no association between ethnicity and incisor of different inclination. However, this result is not in agreement with another study where they concluded that more female Singaporean Chinese had maxillary and mandibular proclination [23].
The current study found that within the same inclination group all mandibular incisors had similar alveolar bone height and thickness. However, a significant difference was observed in different inclinations of lower incisors. The alveolar bone height within the upright group was significantly greater than the proclined group. The mandibular symphysis has a complex curved round like shape, hence the apex of proclined lower incisors will most likely positioned at the shorter curves of the symphysis or between menthon and the most posterior point of posterior symphysis [24]. Therefore, where the incisor is positioned (inclination) will affect the height. In addition, the study found no association between facial type and alveolar bone height [7]. In contrast, Paula G observed that with increasing age, the alveolar bone height also increased with decreased inclination of lower incisors [25]. During overbite reduction, intrusion of an upright lower incisor is safer than proclined lower incisor because the alveolar bone height is greater. Hence, careful intrusion of proclined lower incisor is necessary because the alveolar bone height is much reduced. Furthermore, during overbite reduction, the lower incisor may become more proclined due to the play between the bracket slot and the 19x25’’ stainless steel archwire. The distance between the incisor root apex to the labial or lingual cortical alveolar bone was about 3.0 to 4.0 mm in thickness. Therefore, further proclination of a proclined lower incisors may push the apical root out of the alveolar bone supports. According to Yu, et al. [9] excessive labial and lingual tooth movements can contribute to periodontal problems such as bone dehiscence with an unfavorable mucogingival aspect as well as apical root resorption.
This study indicates that labial bone thickness was greater in proclined incisors. This could be due to the natural shape of symphysis where the concavity of mandibular symphysis was much increased in proclined lower incisor, hence increased the alveolar bone thickness. Another study suggested that when the lower incisor was proclined, the lower central incisor root apex was closer to the lingual alveolar crest, however, our study revealed that the lingual thickness is like both proclined and upright incisors [9]. Therefore, the total labial thickness in proclined group is contributed by the thicker labial bone and the apex of upright incisor is closer to the labial alveolar crest. Hence emphasis should be given when retroclining an upright lower incisor to avoid dehiscence and root resorption. This fact must be considered when planning labial or lingual inclination movements.
Alveolar height and thickness were also compared between all four lower incisors within the procline and upright group separately. In both groups, the lower incisors exhibit similar alveolar bone height and alveolar bone thickness. This occurs because the alveolar bone encapsulates the buccolingual thickness and root length of all the lower incisors was generally the same. The mean buccolingual width of all mandibular incisors was the same (6.0 mm) in normal subjects and the mean root length was 12.0mm [26].
Our finding showed that there was no significant difference in the total and cancellous bone height in both proclined and upright group. This is in contrast with reports by Gracco, et al. [6] where the total and cancellous bone heights were greater at the central incisors than at the lateral incisors in all various facial types. However, our results agree with another study which reported no significant difference in alveolar bone height and thickness within all the mandibular incisors [16]. The labial cancellous bone thickness was thicker in proclined lower incisors and this coincides with another study [5]. The same study also noted that the more proclined the lower incisors, the greater the cancellous and total lingual thickness. However, the authors’ study found similar thickness of cancellous and total lingual thickness in both upright and proclined incisors [5]
The distance between the incisor root apex to the labial or lingual cortical alveolar bone are within 3.0 to 4.0 mm. This suggests that one should limit tooth movement during orthodontic treatment within this margin. Our study found that the average total alveolar thickness at the apex was 8.1mm in upright lower incisors and 9.2 mm in proclined lower incisors. Hence, using miniscrew of 6mm and 8mm length would be ideal and safe in the lower labial segment especially in proclined lower incisor. This is in agreement with study by Kuroda who suggested miniscrews length should be enough to allow 5mm to 6mm of bone support to prevent any perforations and failure of miniscrew [27]. Placement of miniscrew for overbite reduction or canting correction is much safer in upright lower incisors as the bone height is greater than proclined lower incisors. Miniscrew of 6mm or 8mm would be idle to avoid any damages. This would compensate for the use of smaller diameter miniscrew as the interradicular spaces between lower incisors are smaller.
Lower incisor inclination may influence the surrounding alveolar bone. There was a significant negative association between lower incisor inclination and total alveolar and cancellous bone height. A positive association was also observed between inclination of incisors and thickness of alveolar bone. When the lower incisor was proclined, the alveolar bone height reduced whilst the thickness increased. This agrees with study by Quan et al. [28] where they show significant positive correlations between the lower central incisor inclination and the morphological contour of the alveolar bone. The thicker alveolar thickness at apex level may have allowed greater movement of the lower incisors in patients who had not undergone orthodontic treatment. However, there was no correlation between incisor inclination and the thickness of lingual part of the alveolar bone.
Nevertheless, our evaluation was a one-time retrospective, and it would be advantageous to observe the dynamics of changes in bone volume during orthodontic treatment. It would also be interesting to see any racial variation in the morphology of the alveolar bone surrounding lower incisors especially in proclined lower incisors. In addition, we examined generally healthy patients. The results would probably be different in patients with systemic diseases which has an impact on the bone.
Conclusion
It was observed that lower incisor inclinations influenced bone limits of the lower incisor in the mandibular symphysis. The normally inclined lower incisors have significantly greater total bone height than proclined lower incisors. Proclined lower incisors have greater total bone thickness, labial and cancellous bone thickness compared to the upright lower incisors. There is a significant relationship between the incisor inclination and the alveolar bone height and alveolar bone thickness.
Acknowledgments
This research was supported by Fundamental Research Grant Scheme, Ministry of Higher Education Malaysia (FRGS/1/2011/SKK/ UKM/03/14).
References
- Yamada C, Kitai N, Kakimoto N, et al. Spatial relationship between the mandibular central incisor and associated alveolar bone in adults with mandibular prognathism. Angle Orthod 2007; 77:766–772.
- Apajalahti S, Peltola JS . Apical root resorption after orthodontic treatment: A retrospective study. Eur J Orthod 2007; 29:408–412.
- Handelman S. The anterior alveolus: Its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod 1996; 66:95-110.
- Enhos S, Uysal T, Yagci A, et al. Dehiscence and fenestration in patients with different vertical growth patterns assessed with cone-beam computed tomography. Angle Orthod 2012; 82:868–874.
- Srebrzyńska-Witek A, Koszowski R, Różyło-Kalinowska I. Relationship between anterior mandibular bone thickness and the angulation of incisors and canine: A CBCT study. 2018; 22:1567-1578.
- Gracco A, Luca L, Bongiorno MC, et al. Computed tomography evaluation of mandibular incisor bony support in untreated patients. Am J Orthod and Dentofacial Orthop 2010; 138:179-87.
- Türk T, Elekdag-Türk S, Dinçer M. Clinical evaluation of the centre of resistance of the upper incisors during retraction. Eur J Orthod 2005; 27:196–201.
- Molina-Berlanga N, Llopis-Perez J, Flores-Mir C, et al. Lower incisor dentoalveolar compensation and symphysis dimensions among class I and III malocclusion patients with different facial vertical skeletal patterns. Angle Orthod 2013; 83:948–955.
- Yu Q, Pan X, Ji G, et al. Lower incisal inclination and morphology of the supporting alveolar bone. Int J Oral Sci 2009; 1:217–223.
- Chen CH, Nakano H, Liou EJW, et al. A cone-beam next term computed tomographic study of corticol bone thickness in different Class II facial pattern. Orthodontic Waves 2010; 69:131-137.
- Aydogdu E, Ozsoy OP. Effects of mandibular incisor intrusion obtained using a conventional utility arch vs bone anchorage. Angle Orthod 2012; 82:868–874.
- Park HK. 3-D FEA on the intrusion of mandibular anterior segment using orthodontic miniscrews. Korean J Orthod 2011; 41:384
- Gahleitner A, Watzek G, Imhof H. Dental CT: Imaging technique, anatomy, and pathologic conditions of the jaws. Eur Radiol 2003; 13:366–377.
- Gracco A, Lombardoa L, Mancuso G, et al. Upper incisor position and bony support in untreated patients as seen on CBCT Angle Orthod 2009; 79:692-702.
- Gama A, Vedovello S, Filho MV, et al. Evaluation of the alveolar process of mandibular incisor in Class I, II and III individuals with different facial patterns. Cient Ciênc Biol Saúde 2011; 14:95-98.
- Uysal T, Yagci A, Ozer T, et al. Mandibular anterior bony support and incisor crowding: Is there a relationship?. Am J Orthod Dentofacial Orthop 2012; 142:645-653.
- Saltaji H, Flores-Mir C, Major PW, et al. The relationship between vertical facial morphology and overjet in untreated class II subjects. Angle Orthod 2012; 82:432–440.
- Macallister MJ, Rock WP. The eastman standard incisor angulations: Are they still appropriate? British J Orthod 1992; 19:55-58.
- Mohammad HA, Abu Hassan MI, Hussain SF. Cephalometric evaluation for Malaysian Malay by Steiner analysis. Scientific Res Essays 2011; 6:627-634.
- Romero-Delmastro A, Kadioglu O, Currier GF, et al. Digital tooth-based superimposition method for assessment of alveolar bone levels on cone-beam computed tomography images. Am J Orthod Dentofac Orthop 2014; 146:255–263.
- Leung CC, Palomo L, Griffith R, et al. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofac Orthop 2010; 137:109–119.
- Panchez H, Zieber K, Hoyer B. Cephalometric characteristics of Class II division 1 and Class II division 2 malocclusion: A comparative study in children. Angle Orthod 1997; 67:111-120.
- Yeong P, Huggare J. Morphology of Singapore Chinese. Eur J Orthod 2004; 26:605-612.
- Ulaş Ö. The differences of symphysis morphology in class II malocclusions with different vertical growth pattern. Clin Dent Res 2013; 37:3-12.
- Paula G, Mariana M, Mauricio BM, et al. Tomographic Evaluation of the lower incisor’s bone limit in mandibular symphis of orthodontically untreated adults. BioMed Res Int 2017; 2017:1-6.
- Walker SC, Mattick CR, Hobson RS, et al. Abnormal tooth size and morphology in subjects with cleft lip and/or palate in the North of England. Eur J Orthod 2009; 31:68-75.
- Kuroda S, Sugawara Y, Deguchi T, et al. Clinical use of miniscrew implants as orthodontic anchorage: Success rates and postoperative. Am J Orthod Dentofacial Orthop 2007; 131:9-15.
- Quan Yu, Xiao-gang Pan, Guo-ping Ji, et al. Lower incisal inclination and morphology of the supporting alveolar bone. Int J Oral Sci 2009; 1:217–223.
Author Info
Murshida Marizan Nor1*, Marhamah Manan2, Alizae Marny Mohamed1, Tanti Irawati Rosli1 and Azrul Hafiz3
1Faculty of Dentistry, Universiti Kebangsaan Malaysia, Jalan Raja Muda Abdul Aziz, Kuala Lumpur, Malaysia2Ministry of Health, Johor, Malaysia
3Faculty of Dentistry, Universiti Sains Islam Malaysia (USIM), Kuala Lumpur, Malaysia
Citation: Murshida Marizan Nor, Marhamah Manan, Alizae Marny Mohamed, Tanti Irawati Rosli, Azrul Hafiz, Lower Incisor Inclination and Bony Support in Class II Skeletal Pattern Patients-CBCT Study, J Res Med Dent Sci, 2020, 8 (3):85-93.
Received: 16-Apr-2020 Accepted: 30-Apr-2020
