Research - (2021) Volume 9, Issue 2
Management of Intrusive Luxation of Traumatised Permanent Tooth a Decision Tree Analysis
Krisha Doshi, Ajitha P and Raghu Sandhya*
*Correspondence: Raghu Sandhya, Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences (SIMATS), Saveetha University Tamilnadu, Chennai, India, Email:
Abstract
Traumatic intrusion of permanent teeth is a relatively rare but serious dental injury. Various treatment approaches have been suggested so far, regarding management of intrusive luxation. These include an interdisciplinary approach of surgical, orthodontic and endodontic approaches. However, developments of complications such as pulp necrosis, inflammatory root desorption, replacements desorption, and ankylosis and bone loss plays an important role in selection of the treatment modality. Numerous other factors need to be considered before making a decision regarding the treatment of intruded permanent teeth. These include the age of the patient, the maturity of the tooth, the severity of intrusion, etc. the best treatment approach is the one with the least possible complications. This article aims at reviewing the existing treatment modalities and treatment approaches of intrusive luxation and formulates a decision tree after taking into consideration experimental and clinical study findings and observations from other authors.
Keywords
Decision tree, Dental trauma, Dental luxation injuries, Intrusion management, Intrusive luxation management, Permanent teeth
Introduction
Dental trauma and its various consequences are a common complaint in dental practice. Although they are more prevalent in children, adults too tend to experience dental trauma, or more commonly, delayed complications of the same. Trauma to the oral region occurs frequently and comprises 5% of all injuries for which people seek treatment. Amongst all facial injuries, dental injuries are the most common [1], of which crown fractures and luxation’s occur most frequently (15-61%) [2]. The primary etiologic factors are bicycle injury, sport accidents, falls, and fights. There are five different types of luxation injuries, Concussion, Subluxation, Extrusive luxation, Lateral luxation, and Intrusive luxation. The factors establishing the type of lesion are the force and direction of the impact of the injury [3]. Dent alveolar injuries involve fractured, displaced, or lost teeth. This could have a significant impact on the functional, esthetic, speech, and psychological wellbeing of the individual, especially children, affecting their quality of life [4]. Most of the time, these are complex injuries involving different types of tissues that require careful examination, accurate diagnosis and treatment planning. Over and above, this must happen promptly, all within a matter of minutes [5].
Intrusion or intrusive luxation is defined as the axial displacement of a tooth into its own socket. It is one of the most severe types of dental trauma due to the crushing of the periodontal ligament fibres, the neurovascular bundle and the alveolar bone [1]. Intrusive luxation of permanent teeth is most frequent in the age group 6–12 years [2]. It occurs less frequently than other types of luxations. It comprises 3% of all traumatic injuries in the permanent teeth [5] and 5–12% of dental luxations [6]. It is most often associated with maxillary teeth than mandibular teeth [5,7]. Although it is a rare form of luxation, it is considered to be the type which has the poorest prognosis [8,9]. A variety of therapeutic measures have been reported, but the optimal method of returning the tooth to its normal position remains to be determined [10,11].
Our team has numerous highly cited publications on well-designed clinical trials and lab studies [12-27]. This has provided the right platforms for us to pursue the current research. Over the years there have been numerous strategies devised for the management of intrusive luxation. Currently a comprehensive treatment involving either endodontic, orthodontic or oral surgical procedures; or a combination of all these procedures is most accepted. This paper aims at reviewing the diagnosis and management of intrusive luxations in permanent teeth. It also includes a formulated decision tree to help understand the various factors that need to be considered before making a decision for the management of intrusive luxation’s in permanent teeth.
Clinical Features and Diagnosis
Intrusive luxation is characterized by displacement of the tooth into its socket. There may be comminution of the alveolar socket and expansion of the alveolus to accommodate the malposed tooth. Patients usually report with pain and sensitivity in relation to the affected tooth. It may also be associated with soft tissue injuries. Upon percussion, the intruded tooth elicits a metallic sound similar to an ankylosis tooth. This feature distinguishes it from an unerupted tooth. The intrusion can be partial or complete. In deciduous teeth, the intrusion is usually partial and the crown is titled palatally, while permanent teeth show higher prevalence of complete intrusion with the crown titled more buccally [28]. In some situations, the intrusion may be so severe that the affected tooth appears to be entirely missing upon clinical examination [29]. Discoloration of the crown is another feature that may be evident. Radiographic examination may reveal partial or total obliteration of the periodontal ligament space. The cemento-enamel junction is located more apically as compared to the adjacent noninjured tooth. At times it may be located even apical to the marginal bone level.
The guidelines of the International Association of Dental Traumatology recommend that the lack of sensibility to the thermal or electrical stimulus accompanied by another sign, such as crown discoloration or the presence of apical radiolucency indicates necrotic pulp [30]. However, dental discoloration may occur because of the rupture of small blood vessels, which release blood components that penetrate the dentinal tubules. Such a discolouration regresses eventually, restoring the translucency of the enamel [31]. In a similar way to apical radiolucency, Cohenca et al. [32] reported "transient apical breakdown," which affects 4% of luxated teeth and disappears with the reduction of posttraumatic inflammatory symptoms [33].
Complications
Intrusion in permanent teeth could potentially lead to healing complications, such as pulp necrosis, inflammatory radicular resorption, ankylosis, loss of marginal bone support, pulp canal obliteration, calcifications, paralysis or disturbance of the radicular development and gingival retraction [34]. Prevalences of complications including pulp canal obliteration, external root resorption and loss of supporting bone were reported to be 6–35%, 1–18% and 10%, respectively [35]. Stalhane et al. in a survey of 1132 mobile teeth, reported that necrosis of the pulp was the most frequent complication following trauma, pulp death occurring in 54 percent of luxated teeth and 11.6 percent of subluxated teeth [36]. Pulp necrosis may occur either due to severance of blood flow due to the trauma (coagulation necrosis) or due to pulp exposure that enables entry of bacteria (liquefaction necrosis) [37]. Age is considered an important factor in the occurrence of complication and determination of prognosis after trauma. In cases of extensive or total severance of the apical blood supply, pulpal healing is rare if the apical diameter is less than 0.5 mm, such as is found in fully formed teeth, hence causing pulpal necrosis. Pulpal necrosis and loss of pulp vitality in developing permanent teeth results in weak, fracture prone roots that may become weaker when subjected to longterm exposure to calcium hydroxide [38]. In case of these teeth, the large apices (> 0.5mm) improve the possibility of pulpal healing through revascularization [39]. Andreasen et al. used a multivariate analysis to examine the relationship between the cause of the trauma producing luxation and later appearance of complications. In the study, of 189 teeth, 52 percent became nonvital and this was related to the type of luxation and stage of apical development. 22 percent of the teeth showed pulpal obliteration and 11 percent progressive external root resorption [7]. Pulp obliteration is a common complication arising from luxation injuries. These teeth rarely require root canal treatment, unless they become non-vital and symptomatic [40]. External root resorption can be of three types- Surface resorption, inflammatory resorption and Replacement resorption (Ankylosis). Of these, inflammatory resorption and ankylosis are more concerning. Inflammatory root resorption is a very aggressive type of injury-related resorption. It is usually caused by luxation injuries that damage the cemental protection of root surfaces, allowing dentinal tubules to become pathways for bacterial toxins within the canal to trigger osteoclastic activity externally. In immature permanent teeth the resorption precedes at a faster rate because of the larger diameter dentinal tubules [37]. Ankylosis is associated with extensive trauma to the periodontal ligament resulting in loss of vitality of the cells and extensive damage to the cementum. The cementum is exposed to osteoclasts that mistake it for bone and proceed to replace the cementum and dentin with new bone, resulting in a fusing of the bone to the tooth.
In order to avoid such complications, prompt decisions regarding the management of intrusively luxated teeth must be made, especially in young permanent teeth.
Management
Intrusive luxation injuries are known to have the poorest prognosis and the most complex treatment among all tooth injuries. Moreover, the low occurrence of this injury in permanent teeth has resulted in minimal amount of data for the diagnosis and treatment planning for these teeth. Current dental literature suggests different treatment approaches for the management of intrusive luxation injuries, although there is no consensus reached on the optimal treatment of the intruded permanent teeth. The recommended treatment options include: Allowing spontaneous re-eruption of the tooth (Passive repositioning), Immediate surgical repositioning and fixation, and Orthodontic repositioning (Active repositioning) [6,35].
Spontaneous re-eruption is the most conservative approach in the management of intrusive luxation. It was initially recommended by Ellis in 1940 as the treatment of choice for intrusive luxation injuries to prevent further damage to the apical and marginal periodontal tissues [41]. Since then numerous authors have recommended this approach. Spontaneous reeruption has most frequently been used for the treatment of immature teeth since they normally will re-erupt spontaneously because of their high potential for eruption and for pulp and periodontal repair [42]. Some authors have also demonstrated favorable outcomes by using this approach for mature permanent teeth [43]. On the other hand, some authors have criticized the term spontaneous re-eruption, which according to them is unpredictable and pathological rather than developmental, like in normal eruption [44,45]. An important point to be noted while using this approach is that it is time consuming and it may take several months for the tooth to spontaneously re-erupt to its original position. Hence, the clinician must regularly perform vitality tests to keep a check on the vitality of the pulp. In case at any point, the tooth turns nonvital, endodontic therapy must be initiated and surgical or orthodontic approach may be used for repositioning.
Some authors recommend immediate surgical repositioning served as a better alternative to spontaneous eruption in most cases [9,46]. This approach is usually recommended for mature teeth with more severe intrusions that are unlikely to respond to spontaneous eruption. In this approach, the intruded tooth is carefully luxated using an elevator and then brought to its original position using forceps. Immediate splinting of the tooth in this position is done using flexible splints and maintained for 4 weeks. Surgical extrusion of teeth has been strongly opposed by some authors because it may increase the risk of external root resorption, sequestration and loss of marginal bone support [47].
Orthodontic repositioning has been suggested as a possible alternative which allows for remodeling of bone and the periodontal apparatus [48]. It is a more biological approach for the repositioning of an intruded tooth. It helps break the bone bridges of ankylosis that begin to form after trauma as well as allows early endodontic intervention in case of mature teeth which prevents inflammatory resorption [49]. This approach is usually recommended for mature and immature teeth with mild to moderate intrusions. It can also be used for non-vital teeth. Successful outcomes have been obtained by authors using this approach [50]. In spite of this many authors have discouraged the use of orthodontic forces for repositioning of intruded teeth. Turley et al concluded from his research on intruded dog teeth that orthodontic forces had little effect on repositioning intruded teeth and rather resulted in movement of the anchorage teeth [51]. Kenny and Humphrey et al stated that the forces used to move intruded teeth exceed those of conventional orthodontic treatment, and severely intruded teeth do not have a functional and healthy periodontal ligament which plays an important role in orthodontic movement [44,45]. This paper also formulates a decision tree analysis for the management of intrusive luxations in permanent teeth (Figure 1).
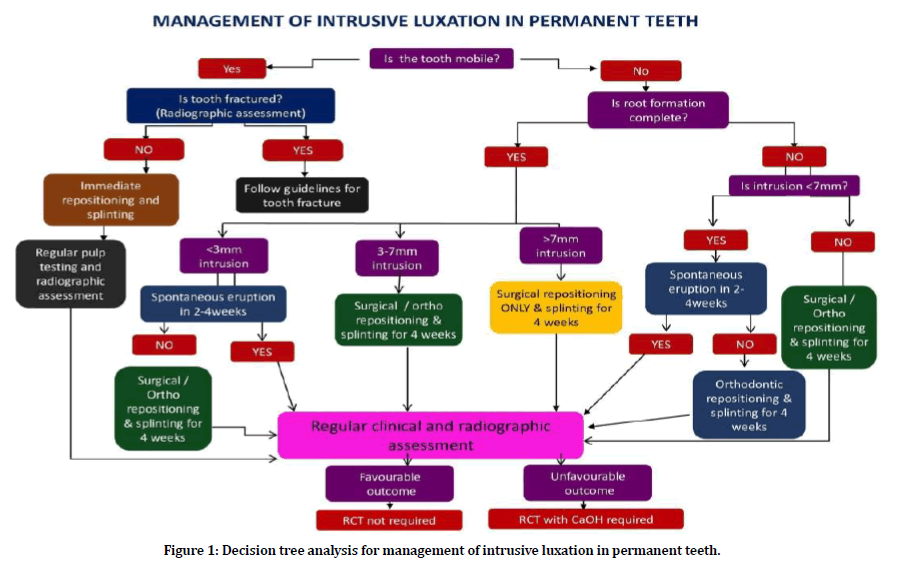
Figure 1. Decision tree analysis for management of intrusive luxation in permanent teeth.
The management of intrusive luxation is dependent on three basic factors- 1) Mobility of the tooth; 2) The completion of root formation; and 3) the severity of intrusion. In case of a mobile fractured tooth, the intruded tooth is immediately and easily repositioned and splinted using a flexible splint for 4 weeks. Regular clinical and radiographic assessment is done at 2, 4, 6-8 week intervals followed by 6 months and 1 year intervals and once every year for 5 years [52]. In case of an unfavourable outcome (nonvital tooth, apical periodontitis, root resorption, etc.) at any of the follow up appointments, endodontic therapy must be initiated immediately. The next factor to be assessed is the maturity of the tooth based on completion of root development. In case of an imobile, immature tooth, the degree of intrusion is evaluated. For a mild to moderate intrusion (<7mm), the first choice of treatment must be spontaneous eruption for 2-4 weeks. If the tooth fails to erupt spontaneously even after 4 weeks, orthodontic repositioning or surgical repositioning of the tooth followed by splinting for 4 weeks, can be done. In case of severe intrusions (>7mm), orthodontic repositioning or immediate surgical repositioning followed by splinting for 4 weeks must be done. In case of immobile mature teeth, again, the severity of intrusion is assessed. For mild intrusions (<3mm), the tooth can be allowed to spontaneously erupt for 2-4 weeks. If the tooth fails to erupt spontaneously, orthodontic or surgical repositioning followed by splinting for 4 weeks is done. In case of moderate intrusion (3- 7mm), spontaneous eruption is not attempted. Immediate surgical repositioning of the tooth followed by splinting for 4 weeks or orthodontic repositioning of the tooth is done. In case of severe intrusions (>7mm), immediate surgical repositioning followed by splinting for 4 weeks is the only choice of treatment.
For all intruded teeth, clinical and radiographic assessment must be done at regular intervals of 2, 4, 6-8 week intervals followed by 6 months and 1 year intervals and once every year for 5 years. In case of an unfavorable outcome (nonvital tooth, apical periodontitis, root resorption, etc) at any of the follow up appointments, endodontic therapy must be initiated immediately.
Conclusion
Intrusive luxation, although rare, is a complex trauma in permanent teeth. Numerous factors need to be considered before formulating a treatment plan in these teeth. The most important factors include the mobility of the tooth, the maturity of the tooth and the severity of intrusion. A comprehensive assessment of all these factors will allow the clinician to narrow down to a particular treatment plan. Of the three modalities of treatment for intrusive luxation, allowing the tooth to spontaneously erupt is the most conservative and safest option. It shows the least complications. Hence, as far as possible, this line of treatment must be attempted. Surgical repositioning followed by splinting and orthodontic repositioning have also shown successful outcomes in management of intruded permanent teeth. A lot more case reports and clinical trials must be performed by clinicians and researchers so that a definitive treatment planning for each case of intrusive luxation can be made.
Conflict of Interest
The authors deny any conflicts of interest related to this review paper.
Acknowledgement
The authors would like to acknowledge the institution and faculty of the Department of Conservative Dentistry and Endodontics for their support while writing this paper.
References
- Addo ME. Textbook and color atlas of traumatic injuries to the teeth. 4th Edn Br Dent J 2007.
- Glendor U, Halling A, Andersson L, et al. Incidence of traumatic tooth injuries in children and adolescents in the county of Vastmanland, Sweden. Swedish Dent J 1996; 20:15–28.
- Brandt RS. Textbook and colour atlas of traumatic injuries to the teeth. 3rd Edn J Dent 1995.
- Ilma de Souza Cortes M, Marcenes W, Sheiham A. Impact of traumatic injuries to the permanent teeth on the oral health‐related quality of life in 12–14‐year‐old children. Community Dent Oral Epidemiol 2002; 30:193-198.
- Andreasen JO. Pulp and periodontal tissue repair‐regeneration or tissue metaplasia after dental trauma. A review. Dent Traumatol 2012; 28:19-24.
- Zerman N, Cavalleri G. Traumatic injuries to permanent incisors. Endodont Dent Traumatol 1993; 9:61–64.
- Andreasen JO. Etiology and pathogenesis of traumatic dental injuries. A clinical study of 1,298 cases. Scandinavian J Dent Res 1970; 78:329–342.
- Skiellkr V. The prognosis for young teeth loosened after mechanical injuries. Acta Odont Scandinavica 1960; 18:171–181.
- https://www.jendodon.com/article/S0099-2399(07)00750-9/pdf
- Bruszt P. Secondary eruption of teeth intruded into the maxilla by a blow. Oral Surg Oral Med Oral Pathol 1958; 11:146–149.
- Azeem RA, Sureshbabu NM. Clinical performance of direct versus indirect composite restorations in posterior teeth: A systematic review. J Conservative Dent 2018; 21:2–9.
- Govindaraju L, Neelakantan P, Gutmann JL. Effect of root canal irrigating solutions on the compressive strength of tricalcium silicate cements. Clin Oral Investigations 2017; 21:567–571.
- Janani K, Sandhya R. A survey on skills for cone beam computed tomography interpretation among endodontists for endodontic treatment procedure. Indian J Dent Res 2019; 30:834–838.
- Jenarthanan S, Subbarao C. Comparative evaluation of the efficacy of diclofenac sodium administered using different delivery routes in the management of endodontic pain: A randomized controlled clinical trial. J Conservative Dent 2018; 21:297–301.
- Khandelwal A, Palanivelu A. Correlation between dental caries and salivary albumin in adult population in Chennai: An In Vivo study. Bra Dent Sci 2019; 22:228–233.
- Malli Sureshbabu N, Selvarasu K, Nandakumar M, et al. Concentrated growth factors as an ingenious biomaterial in regeneration of bony defects after periapical surgery: A report of two cases. Case Reports Dent 2019; 2019.
- Manohar MP, Sharma S. A survey of the knowledge, attitude, and awareness about the principal choice of intracanal medicaments among the general dental practitioners and nonendodontic specialists. Indian J Dent Res 2018; 29:716–720.
- Nandakumar M, Nasim I. Comparative evaluation of grape seed and cranberry extracts in preventing enamel erosion: An optical emission spectrometric analysis. J Conservative Dent 2018; 21:516–520.
- Poorni S, Srinivasan MR, Nivedhitha MS. Probiotic strains in caries prevention: A systematic review. J Conservative Dent 2019; 22:123–128.
- Rajakeerthi R, Ms N. Natural Product as the Storage medium for an avulsed tooth–A systematic review. Cumhuriyet Dent J 2019; 22:249–256.
- Rajendran R, Kunjusankaran RN, Sandhya R, et al. Comparative evaluation of remineralizing potential of a paste containing bioactive glass and a topical cream containing casein phosphopeptide-amorphous calcium phosphate: An in vitro study. Pesquisa Br Odont Clin Integrada 2019; 19:1–10.
- Ramarao S, Sathyanarayanan U. CRA grid-A preliminary development and calibration of a paper-based objectivization of caries risk assessment in undergraduate dental education. J Conservative Dent 2019; 22:185–190.
- Siddique R, Nivedhitha MS. Effectiveness of rotary and reciprocating systems on microbial reduction: A systematic review. J Conservative Dent 2019; 22:114–122.
- Siddique R, Sureshbabu NM, Somasundaram J, et al. Qualitative and quantitative analysis of precipitate formation following interaction of chlorhexidine with sodium hypochlorite, neem, and tulsi. J Conservative Dent 2019; 22:40–47.
- Siddique R, Nivedhitha MS, Jacob B. Quantitative analysis for detection of toxiC elements in various irrigants, their combination (precipitate), and para-chloroaniline: An inductively coupled plasma mass spectrometry study. J Conservative Dent 2019; 22:344–350.
- Teja KV, Ramesh S, Priya V. Regulation of matrix metalloproteinase-3 gene expression in inflammation: A molecular study. J Conservative Dent 2018; 21:592–596.
- Soares TR, Silva LP, Salazar SL, et al. Profile of intrusive luxation and healing complications in deciduous and permanent teeth–A retrospective study. Acta Odontologica Scandinavica 2018; 76:567-571.
- Spalding PM, Fields HW, Torney D, et al. The changing role of endodontics and orthodontics in the management of traumatically intruded permanent incisors. Pediatr Dent 1985; 7:104–110.
- DiAngelis AJ, Andreasen JO, Ebeleseder KA, et al. International association of dental traumatology guidelines for the management of traumatic dental injuries: Fractures and luxations of permanent teeth. Dent Traumatol 2012; 28:2-12.
- Casula L, Vigano L, Casula L. Does post-traumatic transient discoloration indicate a good pro-gnosis? Case report with 2 years of follow-up. Int J Appl Dent Sci 2018; 4:193-196.
- Cohenca N, Karni S and Rotstein I. Transient apical breakdown following tooth luxation. Dental Traumatol ; 19:289–291.
- Ersahan S, Sabuncuoglu FA, Oktay EA. The efficacy of laser doppler flowmetry, electric pulp test and cold test in diagnosing revascularization of extrusively luxated immature maxillary incisors. Pakistan J Med Sci Quarterly 2018; 34:787–793.
- Gomes GB, Da Costa CT, Bonow MLM. Traumatic intrusion of permanent teeth: 10 years follow-up of 2 cases. Dent Traumatol 2013; 29:165–169.
- Andreasen JO, Andreasen FM, Andersson L. Textbook and color atlas of traumatic dental injuries to the teeth. Copenhagen: Munksgaard 1994; 366–370.
- Stalhåne J, Hedegård B. Traumatised teeth in children aged 7--15 years. Part II. Swedish Dent J 1975; 68:157–169.
- Bakland LK, Andreasen JO. Dental traumatology: Essential diagnosis and treatment planning. Endodontic Topics 2004; 7:14-34.
- Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol 2002; 18:134–137.
- Andreasen FM, Zhijie Y, Thomsen BL. Relationship between pulp dimensions and development of pulp necrosis after luxation injuries in the permanent dentition. Endodont Dent Traumatol 1986; 2:90–98.
- Andreasen JO. Luxation of permanent teeth due to trauma a clinical and radiographic follow‐up study of 189 injured teeth. Eur J Oral Sci 1970; 78:273-86.
- Jacobsen I, Kerekes K. Long-term prognosis of traumatized permanent anterior teeth showing calcifying processes in the pulp cavity. Eur J Oral Sci 1977; 85:588–598.
- Chan AW, Cheung GS, Ho MW. Different treatment outcomes of two intruded permanent incisors--a case report. Dent Traumatol 2001; 17:275–280.
- Shapira J, Regev L and Liebfeld H. Re-eruption of completely intruded immature permanent incisors. Dent Traumatol 1986; 2:113–116.
- Faria G, Silva RAB, Júnior MF, et al. Re-eruption of traumatically intruded mature permanent incisor: case report. Dent Traumatol 2004; 20:229–232.
- Humphrey JM, Kenny DJ, Barrett EJ. Clinical outcomes for permanent incisor luxations in a pediatric population. Intrusions. Dent Traumatol 2003; 19:266-273.
- Kenny DJ, Barrett EJ, Casas MJ. Avulsions and intrusions: the controversial displacement injuries. J Canadian Dent Assoc 2003; 69:308-313.
- Kinirons MJ, Sutcliffe J. Traumatically intruded permanent incisors: A study of treatment and outcome. Br Dent J 1991; 170:144–146.
- Andreasen FM, Pedersen BV. Prognosis of luxated permanent teeth—the development of pulp necrosis. Dent Traumatol 1985; 1:207–220.
- Perez B, Becker A, Chosack A. The repositioning of a traumatically intruded mature, rooted permanent incisor with a removable orthodontic appliance. J Pedodont 1982; 6:343–354.
- Biederman W. Etiology and treatment of tooth ankylosis. American journal of orthodontics 1962; 48:670–684.
- Calasans-Maia J de A, Calasans-Maia, Matta ENR da, et al. Orthodontic movement in traumatically intruded teeth: A case report. Dent Traumatol 2003; 19:292–295.
- Turley PK, Joiner MW, Hellstrom S. The effect of orthodontic extrusion on traumatically intruded teeth. Am J Orthodont 1984; 85:47-56.
- Di Angeles A, Andreasen J, Ebeleseder K, et al. IADT Guidelines for the management of traumatic dental injuries: 1—Luxation injuries to permanent teeth. Dent Traumatol 2012; 28:2–12.
Author Info
Krisha Doshi, Ajitha P and Raghu Sandhya*
Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences (SIMATS), Saveetha University Tamilnadu, Chennai, IndiaCitation: Krisha Doshi, Ajitha P, Raghu Sandhya, Management of Intrusive Luxation of Traumatised Permanent Tooth a Decision Tree Analysis, J Res Med Dent Sci, 2021, 9 (2): 258-264.
Received: 23-Sep-2020 Accepted: 12-Feb-2021
