Research - (2022) Volume 10, Issue 1
Management of Isolated Nasal Bone Fracture and Pretraumatic Dentoalveolar Condition
Karthik Shunmugavelu1* and Kumaravel Subramaniam2
*Correspondence: Karthik Shunmugavelu, Mercy Multispeciality Dental Centre, Thiruneermalai Main Road Chrompet Chennai, India, Email:
Abstract
The most important bone in the facial region to be involved in trauma is the nasal bone, constituting 40%. Pre and post traumatic analysis play a major role in the esthetics and functional demands. Here, we present a case reported with nasal bone fracture and dentoalveolar trauma. The treatment plan included closed reduction of fractured nasal bone under general anaesthesia and endodontic therapy followed by prosthodontic rehabilitation of discoloured maxillary central incisors. The main purpose of the article is to emphasise the importance of immediate and proper plan and execution of well-defined treatment methods in order to obtain significant esthetics and function considering the patient age, nature of the condition and socioeconomic status.
Keywords
Nasal bone fracture, Dentoalveolar trauma, Closed reduction, Endodontic therapy, Prosthodontic rehabilitation
Introduction
The most common activities resulting in facial trauma are road traffic accidents, interpersonal violence, fall, sports, and physical abuse [1]. About 40% of the injuries involve the nasal bone. Due to its prominent nature, architecture and supportive thin nasal septum, tip of the nose fractures easily. Anatomically, the nose is bounded anteriorlyinferiorly by cartilage and posteriorly – superiorly by bone. The cartilaginous framework consists of maxilla, nasal process of frontal bone and a pair of nasal bones. The nasal bone fracture is usually associated with profuse bleeding. Kiesselbach’s area which plays an important role in epistaxis provides a rich vascular network [2]. Usually, nasal packing can be done to control bleeding. In case of pack failure, arterial ligation may be needed [3,4]. The following case depicts a male patient with nasal bone fracture associated with dentoalveolar trauma involving maxillary central incisors which were treated by closed reduction and involved teeth were endodontically and prosthodontically rehabilitated.
Case Report
A 35-year-old male attended the Department with history of road traffic accident. Clinical picture included swelling, epistaxis, deviation, obliteration of nasolabial fold, crepitus, tenderness, and stuffiness in nasal region along with dentoalveolar trauma involving discoloured (discolouration was seen before trauma) maxillary central incisors. Radiological investigations such as 3D facial CT revealed displaced fracture of nasal bone. Treatment plan included closed reduction of fractured nasal bone under general anaesthesia. The patient was placed in supine position, general anaesthesia administered through endotracheal intubation. Fracture site prepared and draped. Extra oral painting done with 5% povidone-iodine solution. Intranasal cleaning with was done with betadine gauze pack and 2% xylocaine soaked in gauze was used for topical anaesthesia. Fracture site reduced with Ash septal forceps and right and left Walsham forceps. The shape and symmetry of the nose obtained. Haemostasis achieved. Nasal splint applied over the nose for stabilization and immobilization. GA recovery was uneventful. Patient was reviewed and advised about the dentoalveolar trauma to be treated within a week. Clinical examination during review revealed fractured maxillary central incisors, 21 which were already discoloured before the trauma. After oral prophylaxis, radiovisiography was taken in relation to 11, 21. Patient was advised endodontic therapy followed by prosthodontic rehabilitation which included two-unit zirconia fixed partial denture (Figures 1-6).

Figure 1. Clinical picture depicting nasal region trauma and deviation.
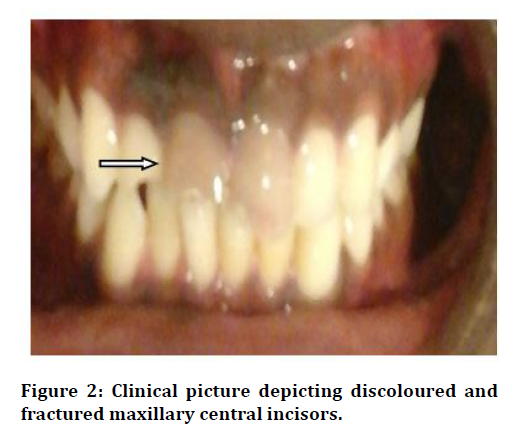
Figure 2. Clinical picture depicting discoloured and fractured maxillary central incisors.
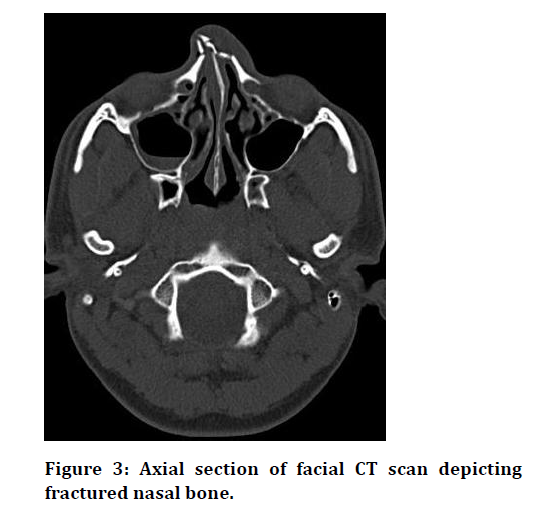
Figure 3. Axial section of facial CT scan depicting fractured nasal bone.
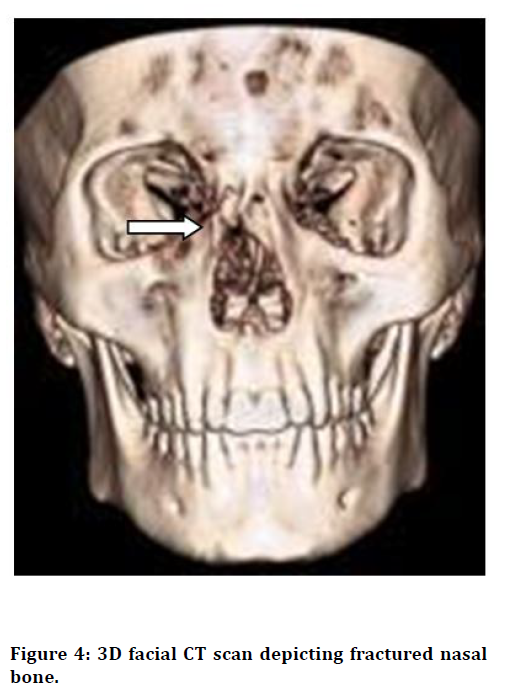
Figure 4. 3D facial CT scan depicting fractured nasal bone.

Figure 5. Post operative clinical picture
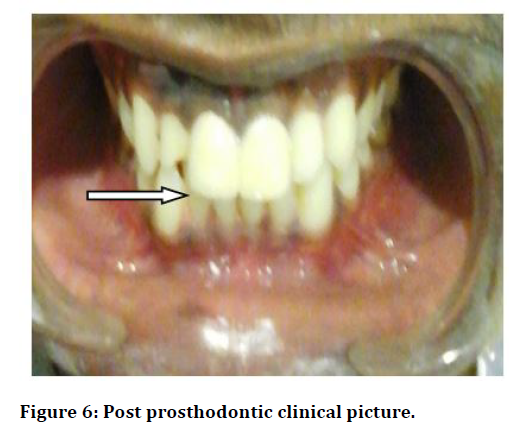
Figure 6. Post prosthodontic clinical picture
Discussion
Common events such as road traffic accidents, accidental fall, interpersonal abuse, ssand sports activities might result in facial injury [1]. The framework is constituted by nasal process, maxilla, paired nasal bones and bounded by cartilage–anteriorly, inferiorly and bone– posteriorly, superiorly. The cartilaginous nature of nasal structures is prone to injury [2]. The combination of nerves, mucous glands, soft tissues, and muscles play an important role in nasal sensation and function [5-8]. The nasal tip fractures due to thinned nasal septum. The anterior ethmoid artery is responsible for anterior epistaxis while a branch of sphenopalatine artery for posterior epistaxis. The direction of impact such as frontal results in displacement in posterior direction while lateral impact results in depression on the involved side. The rich vascular network is contributed by Kiesselbach’s area [2-4]. Detailed clinical assessment includes duration and extent of bleeding, past medical history, past surgical history, and alcohol usage. Careful examination of adjacent facial bones should be done to rule their involvement [11-14]. Even thorough and complete body examination pertaining to trauma was carried out to rule out comorbidity
Based on the pathology, nasal trauma has been classified (modified Murray classification) as follows:
• Soft tissue injury.
• Simple unilateral nondisplaced.
• Simple bilateral nondisplaced.
• Simple displaced.
• Closed comminuted.
• Open comminuted.
Clinical findings of nasal bone fracture include swelling, epistaxis, ecchymosis, deformity, indentation, irregularity. 3D facial CT plays an important role in assessment of nasal bone fracture5,8. Irrigation and debridement might be needed in case of open wound. Two instruments such as Walsham and Ash forceps are used for reduction of displaced septum and impacted nasal structures [6-8]. Saddle nose deformity might result. To achieve proper shape, external splint can be applied for one week. The factors such as bone process, facial size and bone elasticity determine the difference in incidence of nasal trauma between a paediatric and adult. Structural integrity of the nose should be assessed 6 to 12 weeks post operatively. Postoperative complications such as septal haematoma, epistaxis, adhesions can be minimized by nasal packing [9-14]. Non-comminuted and simple fractures can be managed by closed reduction. Management of nasal trauma depends upon various factors such as age, time elapsed, necessity, anaesthesia and treatment plan.
Conclusion
Hereby we conclude that all the nasal bone fracture wouldn’t be an isolated one. Hence the comorbidities should be assessed prior to the treatment. In our case, we experienced the above mentioned circumstances, a previous comorbid condition of dental trauma which was planned and treated in the post op follow up.
References
- Smith JA. Nasal emergencies and sinusitis. In: Tinitinalli JE, Ruiz E, Krome RL, et al. Emergency medicine: A comprehensive study guide. 4th Edn. New York: McGraw-Hill, 1996; 1097-90.
- Hester TO, Campbell JP. Diagnosis and management of nasal trauma for primary care physicians. J Ky Med Assoc 1997; 95:386-92.
- Cummings CW. Otolaryngology-head & neck surgery. 3rd Edn. St. Louis: Mosby 1998; 871.
- Bailey BJ. Head and neck surgery-otolaryngology. Philadelphia: Lippincott 1993; 996.
- Higuera S, Lee EI, Cole P, et al. Nasal trauma and the deviated nose. Plast Reconstr Surg 2007; 120:64S-75S.
- Sargent LA, Rogers GF. Nasoethmoid orbital fractures: Diagnosis and management. J Craniomaxillofac Traum 1999; 5:19-27.
- Rhea JT, Rao PM, Novelline RA. Helical CT and three-dimensional CT of facial and orbital injury. Radiol Clin North Am 1999; 37:489-513.
- Cox AJ. Nasal fractures-the details. Facial Plast Surg 2000; 16:87-94.
- Repanos C, Mc Donald SE, Sadr AH. A survey of postoperative nasal packing among UK ENT surgeons. Eur Arch Otorhinolaryngol 2009; 266:1575-577.
- Fairbanks DN. Complications of nasal packing. Otolaryngol Head Neck Surg 1986; 94:412-415.
- Stucker FJ, Ansel DG. A case against nasal packing. Laryngoscope 1978; 88:1314-1317.
- Kucik CJ, Clenney TL, Phelan J. Management of acute nasal fractures. Am Family Physician 2004; 70:1315-20.
- Bartkiw TP, Pynn BR, Brown DH. Diagnosis and management of nasal fractures. Int J Trauma Nurs 1995; 1:11-8.
- Ellis E III, Scott K. Assessment of patients with facial fractures. Emerg Med Clin North Am 2000; 18:411-48.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Karthik Shunmugavelu1* and Kumaravel Subramaniam2
1Mercy Multispeciality Dental Centre, Thiruneermalai Main Road Chrompet Chennai, Tamil Nadu, India2SPMM Multispeciality Hospital, Salem, Tamilnadu, India
Citation: Karthik Shunmugavelu, Kumaravel Subramaniam, Management of Isolated Nasal Bone Fracture and Pretraumatic Dentoalveolar Condition, J Res Med Dent Sci, 2022, 10(1): 219-222
Received: 23-Dec-2021, Manuscript No. JRMDS-21-42892; , Pre QC No. JRMDS-21-42892 (PQ); Editor assigned: 27-Dec-2021, Pre QC No. JRMDS-21-42892 (PQ); Reviewed: 10-Jan-2022, QC No. JRMDS-21-42892; Revised: 13-Jan-2022, Manuscript No. JRMDS-21-42892 (R); Published: 20-Jan-2022
