Review Article - (2023) Volume 11, Issue 1
Management Of Uterine Fibroid
Vitthal Agrawal*, Deepika Deewani and Arpita Jaiswal Singham
*Correspondence: Vitthal Agrawal, Department of Obstetrics and Gynecology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi, Wardha, Maharashtra, India, Email:
Abstract
Fibroid of Uterus are the most prevalent tumour affecting middle aged women, causing substantial morbidity and potentially impacting fertility. The precise aetiology of uterine fibroids is unknown. fibroids may go in families and are regulated by hormone level. Obesity and consumption of meat are some of the risk factor associated with uterine fibroids. Abnormal bleeding, masses in pelvis, discomfort in pelvis, infertility, bulk symptoms, and obstetric problems are some of the clinical manifestations. Females with symptomatic fibroids who want to keep their fertility confront challenging treatment options.If there are no symptoms, treatment is usually not required. Nonsteroidal anti-inflammatory drugs (NSAIDs)are used for treatment of pain and bleeding such as ibuprofen while other drug such as acetaminophen is used for pain.Iron supplements may be required in women to treat excessive bleeding.Medications of the gonadotropin-releasing hormone agonist may reduce the size of the fibroids, but they are costly and have adverse effects.Surgical removal of fibroids may be indicated in patient if the symptoms are severe. Uterine artery embolization may also be beneficial. Fibroid cancers are extremely uncommon and are classified as leiomyosarcomas.They do not appear to be the result of benign fibroids. Number, size and location of fibroid will decide the management of uterine fibroid. Hysterectomy is the main stay treatment for symptomatic fibroids, such as those producing monthly irregularities (e.g., heavy and irregular uterine bleeding), iron deficiency anaemia, or mass symptoms (e.g pain in pelvis, obstructive symptoms). Black race was the only characteristic consistently shown to raise Uterine fibroid risk by two to thrice when compared to white race.
Keywords
Fibroids, NSAIDs, Hysterectomy, Uterine fibroids, Gonadotropin
Introduction
Uterine fibroids are the most prevalent kind of tumor in women. Clinical manifestations include abnormal bleeding, mass in pelvis, pain in pelvic region, infertility, bulk symptoms and obstetric issues [1-2]. This review article discusses the available medical and surgical options for the treatment of uterine fibroids, including oral progestogens, levonorgestrel intra uterine device, gonadotropin releasing hormone analogues and progesterone receptor modulators, as well as surgical options such as hysterectomy, myomectomy and uterine artery embolization [3].
Materials and Methods
Search strategy and selection criteria
We reviewed key papers and also undertook searches of electronic database such as PubMed, Medline, lilacs and central. We excluded non English articles, case reports and studies.
The search items for PubMed were ‘uterine fibroid’ for the past 10 years, along with ‘uterine fibroid management’, ‘hysterectomy’, ‘myomectomy’, ‘leiomyoma’s’, ‘medical management of uterine fibroid’, etc. The South Asian database of controlled clinical trials was searched by use of the term ‘uterine fibroid’. Articles were selected on the basis of their effect on uterine fibroid diagnosis and treatment. We also checked reference list of articles.
Clinical manifestation of uterine fibroid
• Menstrual disturbances: menorrhagia,
poly-menorrhagia, inter menstrual bleeding,
continuous bleeding, postmenopausal bleeding.
• Infertility.
• Pain: spasmodic dysmenorrhea, backache, pain in
abdomen.
• Mass in the abdomen or mass protruding at the
introitus.
• Pressure symptoms on adjacent organs: bladder, ureters, and rectum.
• Pregnancy losses, postpartum hemorrhage, uterine
inversion.
• Vaginal discharge.
Management
Medical management: Iron treatment for anemia, preoperatively, blood is rarely utilized. The medications used to treat menorrhagia are mirena.
If the uterus does not expand after 12 weeks the goal of medical therapy is to keep menorrhagia under control and to boost hemoglobin levels before surgery.
For three months, use 10–25 mg of RU 486 (mifepristone) everyday induces amenorrhea and a 50% reduction in tumor size.
Levonorgestrel intrauterine system: Progestin treats abnormal uterine bleeding.
Advantage: It decreases blood loss, operative time, recovery time.
Disadvantage: Long term management of uterine fibroid with these lead to higher cost, it shows increase recurrence risk with myomectomy.
Gonadotropin releasing hormone analogues: GnRH analogues, when taken for 6 months, decrease tumor growth by 50–80%. This therapy removes the need for surgery in premenopausal women and young women with infertility caused by corneal fibroids. It is also effective in decreasing vascularity and size prior to surgery and it restores hemoglobin levels by inducing amenorrhea or reducing menorrhagia. The fibroid shrinkage allows for a pfannenstiel incision in abdominal surgery, minimally invasive surgery or a vaginal hysterectomy instead of an abdominal hysterectomy and it significantly decreases bleeding. To avoid menopausal symptoms and osteoporosis, monthly depot injections of 3.6 mg should not be given for more than 6 months. It is important to remember that it decreases the size of tumor before surgery or women approaching menopause.
Advantage: For reducing blood loss it is most effective medical management.
Disadvantage: Irregular uterine bleeding.
• Selective progesterone receptor modulators: Drug isoprisinol if women is undergoing surgery, it is drug to be given to women prior to surgery as it decreases size of tumor.
• Oral contraceptives: Oral contraceptive treats the abnormal uterine bleeding by stabilization of endometrium.
• Tranexamic acid: Antifibronlytic therapy.
• Danazol: Is a successful therapy for shrinking fibroids and symptom control. Its usage is restricted due to severe adverse effects. Anti-estrogenic actions are considered to be the mechanism of action. Recent evidence suggests that more careful dosage might enhance safety and side effect profile [4,5].
Surgical therapies
Surgery: Conventional myomectomy and hysterectomy are performed through laparotomy or laparoscopically.
Newer less invasive treatments have been introduced successfully in recent years have been:
• Embolism of the uterine artery.
• Laser ablation guided by MRI.
• Laparoscopic myolysis is a term used to describe the removal of muscle tissue through laparos.
Hysterectomy
Uterus is removed surgically (trans abdominally, trans vaginally or laproscopically).
Hysterectomy or uterine removal is recommended in women beyond the age of 40, in multiparous women and when cancer is present.
Uncontrollable bleeding and unexpected surgical complications myomectomy may need hysterectomy as well.
Hysterectomy ensures the removal of all fibroids as well as the alleviation of symptoms.
Types of hysterectomy
• Abdominal hysterectomy.
• Vaginal hysterectomy.
• Laparoscopic hysterectomy.
Abdominal hysterectomy: The majority of hysterectomies are performed by laparotomy (abdominal incision). An incision is made in abdominal wall, incision is transverse (pfannenstiel), above pelvic bone close to hair line of lower pelvis. This method is used to remove whole reproductive system as above incision will provide most access to reproductive system. Open hysrectomy recuperation time is 4-6 weeks. Chances of having infection are most with this procedure but due to advance in medical practice it is now no worry and is well controlled. An open hysterectomy is the most efficient technique to examine the abdominal cavity and execute complex operations. Before the improvement in vaginal and laproscpically hysterectomy it was only known procedure for the treatment. However, preferred approach in most of cases is vaginal hysterectomy [6].
Vaginal hysterectomy: Vaginal hysterectomy is most preferred type of hysterectomy in most of cases. It is performed through vaginal canal, it is prefer over abdominal hysterectomy because of very few complication, hospital stay duration is very short and it faster recovery rate over abdominal hysterectomy.
Laparoscopic hysterectomy: Laparoscopic hysterectomy is more complicated procedure than vaginal hysterectomy and has better exploration of uterus. Laparoscopic assisted vaginal hysterectomy start with laparoscopy with the complete removal of uterus but with or without removal of ovaries through vaginal canal. It is also known as total hysterectomy as cervix is also removed along with uterus. Once both cervix and uterus are removed upper part of vaginal are sutured known as vaginal cuff [7].
Hysterectomies are the surgical choice of management for women who want to maintain fertility. Trans vaginal and laparoscopic procedure associated with decrease pain, loss of blood, and recovery time contrast with trans abdominal surgery trans abdominal surgery are having higher risk as compared to other procedure (e.g. infection, pain, fever, increased blood loss and recovery time) (Figure 1).
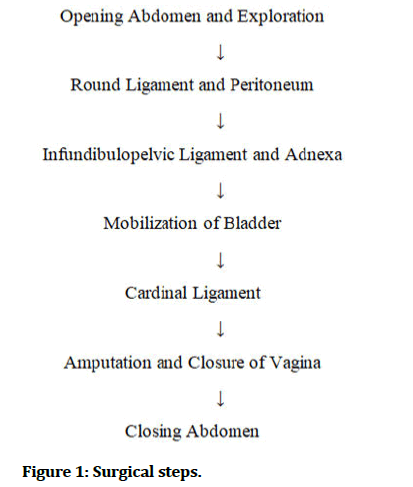
Figure 1: Surgical steps.
Myomectomy: Myomectomy is the surgical removal of fibroids while leaving the uterus intact. It is advised in infertile women or women desirous of having children wishing to keep the uterus, but they should be advised about the possibility of needing subsequent surgery [9].
Advantage: Maintain of fertility with resolve of symptoms.
Disadvantage: Depending upon size and area of tumor its recurrence rate stand slightly higher of 15% to 30% at five year.
Technique of myomectomy
• If the uterus is less than 16–20 weeks in size and movable, a transverse incision can be used to open the abdominal cavity. If complications are expected, such as a big uterus, a fixed uterus with adhesions, concomitant PID, and endometriosis, a vertical Para median incision is preferable.
• The bladder may be raised in cervical and lowlying anterior wall fibroids; care should be taken not to damage it when incising the parietal peritoneum.
• The pelvic organs should be carefully inspected and the feasibility of myomectomy confirmed.
• The preferred incision is over the anterior uterine wall because many fibroid can be removed through minimum size incision.
• The myomectomy clamp should be used to control hemorrhage. The clamp positioned from the pubic end of the abdominal incision to the circular ligaments that will encompass the uterine veins. Sponges’ forceps can be used to temporarily occlude the ovarian veins. If the myomectomy clamp cannot be used, as in the case of cervical fibroids, a rubber tourniquet will suffice.
• The fibroids are enucleated when incision is given on capsule. This will reduce bleeding while also avoiding damage to the bladder and ureter. Enucleating is aided with myomectomy screws.
• After the enucleating, cavity is removed with several catgut sutures as this will avoid scar rupture during subsequent pregnancy and labor and homeostasis is achieved.
• The clamp should be released and homeostasis confirmed [9]. To avoid postoperative adhesions, the raw visceral region should be well peritonized. Adhesions are also reduced by hydrofloation.
Following myomectomy, the uterus remains bulky and must be anteverted by placating the round ligaments with non-absorbable sutures.
Complications: Myomectomy, like any other pelvic surgery, can result in bleeding, infection, bowel blockage, adhesion development, bowel, bladder, fallopian tube, ureter injury, wound infection and wound separation. Furthermore, due to recurrence of symptoms, around 20–25 percent of patients following myomectomy require another pelvic procedure, generally hysterectomy. Recurrent myomas are prevalent, particularly in people who have numerous myomas. Patients with a single myoma had a recurrence rate of 27%, whereas those with numerous myomas have a recurrence rate of 59% [10].
Uterine artery embolization
Interventional radiologic procedure to occlude uterine arteries. Uterine artery embolization is performed to decrease vascularity and fibroid size and Symptom improvement [11].
Menorrhagia was alleviated in 80–90% of cases, pressure sensations in 40–70% of cases, at the end of three months, the volume had dropped by half by 60% after six months and 75% at the end of a year. Thus, this method is presently effectively used in selective cases.
Technique: Bilateral uterine artery embolization is addressed under local anesthesia through percutaneous femoral catheterization. It is accomplished by the use of Polyvinyl Alcohol (PVA), gel foam particles or a combination of the two coils of metal embolization decreases vascularity and the size of the vessel.
Complications
• Pyrexia and infection.
• Discharge from vagina and discharge from bleeding (5%).
• Ischemic pain suggests successful therapy, but can be unbearable and requires analgesia.
• Pulmonary embolism.
• Ovarian vessel blockage (up to 30%).
• Fertility rate is reduced due to adhesions.
• Failure due to inadequate embolization.
• Expulsion of a fibroid into the peritoneal cavity (10%).
• Allergic reaction and contrast induced renal failure.
• Radiation exposure.
• Hematomas at the femoral site.
• Extrusion of a sub-serous fibroid into the peritoneal cavity which requires retrieval.
• Intra peritoneal adhesions.
Laparoscopic myolysis
This is an optional surgery using ND: YAG laser, cryoprobe or diathermy to coagulate a sub-serous fibroid.
MRI guided focused ultrasound
This is a non-invasive procedure that employs a high intensity focused ultrasound beam to heat and destroy fibrous tissue. MRI is used to provide guidance in directing the beam route to the fibroid. A big fibromyoma can be treated in two sessions, or it can be treated in three sessions (Table 1 and Figure 2).
| Treatment | Description | Advantages | Disadvantages | Fertility preserved? |
|---|---|---|---|---|
| Medical therapies Gonadotropin releasing hormone agonists | Preoperative treatment to decrease size of tumours before surgery or in women approaching menopause | Decrease blood loss, operative time, and recovery time | Long-term treatment associated with higher cost, menopausal symptoms, and bone loss; increased recurrence risk with myomectomy | Depends on subsequent procedure |
| Levonorgestrel releasing intrauterine system (mirena) | Treats abnormal uterine bleeding likely by stabilization of endometrium | Most effective medical treatment for reducing blood loss; decreases fibroid volume | Irregular uterine bleeding, increased risk of device expulsion | Yes, if discontinued after resolution of symptoms |
| Non-steroidal anti-inflammatory drugs | Anti-inflammatories and prostaglandin inhibitors | Reduce pain and blood loss from fibroids | Do not decrease fibroid volume; gastrointestinal adverse effects | Yes |
| Oral contraceptives | Treat abnormal uterine bleeding likely by stabilization of endometrium | Reduce blood loss from fibroids ease of conversion to alternate therapy if not successful | Do not decrease fibroid volume | Yes, if discontinued after resolution of symptoms |
| Selective progesterone receptor modulators | Preoperative treatment to decrease size of tumours before surgery or in women approaching menopause | Decrease blood loss operative time, and recovery time; not associated with hypo-estrogenic adverse effects | Headache and breast tenderness progesterone receptor modulator-associated endometrial changes; increased recurrence risk with myornectomy | Depends on subsequent procedure |
| Tranexamic acid (cyklokapron) | Anti-fibrinolytic therapy | Reduces blood loss from fibroids ease of conversion to alternate therapy | Does not decrease fibroid volume; medical contraindications | Yes |
| Surgical therapies Hysterectomy" | Surgical removal of the uterus (trans-abdominally, trans-vaginally, or laparoscopically) | Definitive treatment for women who do not wish to preserve fertility, trans-vaginal and laparoscopic approach associated with decreased pain, blood loss, and recovery time compared with trans-abdominal surgery | Surgical risks higher with trans-abdominal surgery (e.g. infection, pain, fever, increased blood loss and recovery time); morcellation with laparoscopic approach increases risk of iatrogenic dissemination of tissue | No |
| Magnetic resonance guided focused ultrasound surgery | in situ destruction by high intensity ultrasound waves | Non-invasive approach shorter recovery time with modest symptom improvement | Heavy menses pain from sciatic nerve irritation higher re-intervention rate | Unknown |
| Myomectomy | Surgical or endoscopic excision of tumours | Resolution of symptoms with preservation of fertility | Recurrence rate of 15% to 30% at five years, depending on size and extent of tumours | Yes |
| Uterine artery embolization | Interventional radiologic procedure to occlude uterine arteries | Minimally invasive; avoids surgery short hospitalization | Recurrence rate >17% at 30 months post embolization syndrome | Unknown |
Table 1: Comparison of recommended therapies for uterine fibroids.
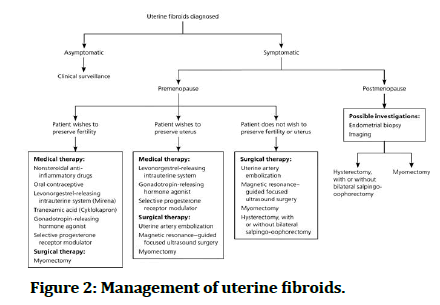
Figure 2: Management of uterine fibroids.
Monthly GnRH injections for fibroid reduction 3–4 months before therapy.
Side effects are:
• Skin burn.
• Pain.
• Nerve damage (rare).
Advantages
• Non-invasive technique.
• Local anesthesia takes 1 to 2 hours to do.
• No hospitalization.
• No scar.
• Quick recovery.
• Fertility preservation technique.
Contraindications
• Calcified fibroid.
• Degenerated fibroid.
Discussion
Uterine fibroids are usually benign neoplasms of the uterus that afflict 5-20% of women of reproductive age.
It may be present without symptoms. However, depending on their size and location, they may contribute to menstrual irregularities, dysmenorrhea and infertility, pain in the abdomen, abdominal fullness, pressure symptoms and complications during pregnancy.
Ultrasonography, laparoscopy and hysteroscopy help in establishing the diagnosis of uterine fibroids. They are also useful to determine the number, location and size of the tumors. This helps in planning treatment.
Asymptomatic tumors often do not require treatment but follow up is recommended. Symptomatic fibroids require treatment.
Myomectomy is recommended for younger women who want to keep their reproductive function, whereas hysterectomy is recommended for older people.
Except for menorrhagia relief, medical therapy does not cure fibroids. When a large fibroid or numerous fibroids are discovered, they are used as adjuvants to surgery. They decrease blood loss after surgery by shrinking the fibroids.
Endoscopic procedures enable the removal of moderate sized myomas. Hysterectomy is advised in elderly and multiparous women [14-19].
Conclusion
Minimally invasive surgery such as laparoscopy, hysteroscopy and arterial embolization has reduced the frequency of abdominal surgeries in women with uterine fibroids. It is now possible to do MRI guided high frequency ultrasonic imaging.
Because of pelvic adhesions and the danger of scar rupture during pregnancy or labor, laparoscopic myomectomy and uterine artery embolization are not indicated in infertile women. Location, size and number of fibroids decide the route of operation.
References
- Laberge PY, Murji A, Vilos GA, et al. Guideline No. 389 medical management of symptomatic uterine leiomyoma an addendum. J Obstet Gynaecol Can 2019; 41:1521–1524. [Crossref][Googlescholar][Indexed]
- Donnez J, Dolmans MM. Uterine fibroid management: From the present to the future. Hum Reprod Update 2016; 22:665–686. [Crossref][Googlescholar][Indexed]
- Faustino F, Martinho M, Reis J, et al. Update on medical treatment of uterine fibroids. Eur J Obstet Gynecol Reprod Biol 2017; 216:61–68. [Crossref][Googlescholar][Indexed]
- Sankaran S, Manyonda IT. "Medical management of fibroids".Best Pract Res Clin Obstet Gynaecol 2008; 22:655–676.[Crossref][Googlescholar][Indexed]
- Vilos GA, Allaire C, Laberge PY, et al. The management of uterine leiomyoma. J Obstet Gynaecol Can 2015; 37:157–178. [Crossref][Googlescholar][Indexed]
- Thomas B, Magos A. "Subtotal hysterectomy and myomectomy-vaginally".Best Pract Res Clin Obstet Gynaecol 2011; 25:133–152. [Crossref][Googlescholar][Indexed]
- Ahluwalia PK. "Total laparoscopic hysterectomy". J Am Assoc Gynecol Laparosc 1996; 3:1–2. [Crossref][Googlescholar][Indexed]
- Konishi I. Basic principle and step by step procedure of abdominal hysterectomy: Part 2. Surg J (N Y) 2018; 5:S11-S21. [Crossref][Indexed]
- Stewart EA, Cookson CL, Gandolfo RA, et al. Epidemiology of uterine fibroids: A systematic review. BJOG Int J Obstet Gynaecol 2017; 124:1501–1512. [Crossref][Googlescholar][Indexed]
- Grifo J, Nassari. Myomectomy. Glob libr women's med 2008. [Crossref]
- Kumar S, Shaw textbook of gynecology 17th edition. Elsevier, 2018.
- Laberge PY, Murji A, Vilos GA, et al. Guideline No. 389-medical management of symptomatic uterine leiomyoma-An addendum. J Obstet Gynecol Can 2019; 41:1521–1524. [Crossref][Googlescholar][Indexed]
- Daga, Rajendra S, Phatak VS. “Ultrasound evaluation of uterine leiomyoma in peri-menopausal females with histopathological correlation.” J Evol Med Dent Sci 2020; 9:562–565. [Googlescholar]
- Khandelwal, Smriti, Surekha Atul Tayade, et al. “Complete uterine septum as an incidental finding as a cause of post-partum haemorrhage and role of balloon tamponade.” J Evol Med Dent Sci 2020; 9:3700–3702. [Crossref][Googlescholar]
- Kolli, Nayana, Manjusha Agrawal, et al. “Correlation of thyroid disorders with Abnormal Uterine Bleeding (AUB).” J Evol Med Dent Sci 2020; 9:398–401. [Googlescholar]
- Pottala, Mounika, Jajoo SS. “Multiple uterine fibroids in a young unmarried woman.” J Evol Med Dent Sci 2020; 1110–1112. [Googlescholar]
- Shelke, Vijay U, Acharya S, et al. “Co-existence of chronic lymphocytic leukemia and malignancy of uterine cervix J Evol Med Dent Sci 2020; 9:1522–1524. [Crossref][Googlescholar]
- Khan, Anam, Acharya N, et al. “Uterine artery embolization: A boon for a near miss case of pseudo aneurysm.” J Clin Diagnostic Res 2020; 14:QD1–3. [Crossref]
- Prasad, Rajnandini, Mariam Khan, et al. “Tuberculosis of uterine cervix presenting with recurrent leucorrhoea in guise of carcinoma of cervix.” J Clin Diagnostic Res 2019; 13:QD06–8. [Crossref][Googlescholar]
Author Info
Vitthal Agrawal*, Deepika Deewani and Arpita Jaiswal Singham
Department of Obstetrics and Gynecology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi, Wardha, Maharashtra, IndiaReceived: 01-Nov-2022, Manuscript No. JRMDS-22-77328; , Pre QC No. JRMDS-22-77328; Editor assigned: 03-Nov-2022, Pre QC No. JRMDS-22-77328; Reviewed: 15-Nov-2022, QC No. JRMDS-22-77328; Revised: 02-Jan-2023, Manuscript No. JRMDS-22-77328; Published: 09-Jan-2023
