Research - (2023) Volume 11, Issue 1
MATERNAL SERUM URIC ACID: A RELIABLE PROGNOSTIC INDICATOR OF PREGNANCY OUTCOME IN WOMEN WITH PREECLAMPSIA-ECLAMPSIA
Eleti Manila Reddy, Manjusha Agrawal*, Deepika Dewani and Nidhi Goyal
*Correspondence: Manjusha Agrawal, Department of Obstetrics and Gynaecology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi, Wardha, Maharastra, India, Email:
Abstract
Preeclampsia and Eclampsia is prevalent among almost one tenth of the pregnant women around the world which usually starts from persistence of high blood pressure over the course of time. After 20 weeks of pregnancy, proteinuria (>300 mg/24 h) and sudden onset hypertension (140 systolic/90 diastolic mm Hg) are signs of preeclampsia, a pregnancy-induced condition. One of the most serious factors contributing to maternal and neonatal morbidity and mortality is still preeclampsia. Preeclampsia is a condition that affects numerous organs and is marked by serious issues with the heart, lungs, kidneys, liver, and nervous system. Negative perinatal consequences for the fetus include intrauterine mortality, preterm birth, and fetal growth limitation. Pregnancy termination is the only effective treatment for preeclampsia, but many expectant mothers can be managed with blood pressure monitoring for the mother, fetal monitoring, and seizure prevention. Predicting preeclampsia and its complications is crucial to preventing maternal and fetal morbidity and mortality. Uric acid is the final substance in the process of purine metabolism. Elevated levels are considered to be an early biomarker of kidney damage in women with pre-eclampsia and also a factor in predicting fetal death. Serum uric acid fluctuates in the pregnancy levels but its correlation with the onset of preeclampsia and eclampsia offers a path forward. As majority of the severe or fatal clinical outcome in case of mother or neonates has been associated with late detection of the preeclampsia or eclampsia thus underlining the importance of the early detection of the same. Serum uric acid can offer valuable diagnostic tool to detect and start treatment as early as possible. More empirical study which covers wide spectrum of pregnant mothers all over the world is needed to concretely establish the positive correlation between uric acid and preeclampsia and eclampsia.
Keywords
Eclampsia, Preeclampsia, Pregnant women, Neonates, Hellp syndrome, Apgar score
Introduction
Pregnancy is one of the most complicated situations of the human anatomy. Various anatomical changes taking place inside the body of a woman along with a growth of a new life, with this many complications are associated with it. Gestational hypertension is the condition which is prevalent among the pregnant women especially after 20 weeks of pregnancy, but persistence of the high blood pressure can result into preeclampsia and eventually eclampsia. These disorders affect 5 to 10 percent of all pregnancies [1-4]. It is regarded as one of the leading cause for mortalities pertaining to neonates and mothers. If the condition is detected early enough then it can be controlled and harmful impact on fetus and mother can be minimized.
Maternal serum uric acid has a correlation with the condition and its increase can be considered as the onset of the feto-maternal complications. Several studies have pointed out that the uric acid measurement can be used as diagnostic test for the diagnosis of preeclampsia. The correlation has been discussed from almost a century ago and reports from as early as late 1910’s suggests that the physicians were trying to establish some sort of connection between the two. Various studies established that the threshold value of uric acid is 6 mg/dl, increased uric acid levels has been associated with various maternal complications like abruption, HELLP syndrome, pulmonary edema, intracranial hemorrhage and fetal complications like IUD, IUGR, preterm births, low birth weight. According to a report published by the world’s premier health agency, WHO, developing countries have more shares of patients of hypertensive disorders during pregnancy than their developed countries. Preeclampsia and eclampsia together accounts for 16 percent of all maternal mortalities around the world. Considering Indian context the percentage of preeclampsia patients getting admitted to the maternity ward ranges from 7 to 10 percent while 7 percentages of all maternal mortalities are caused due to complications caused by preeclampsia and eclampsia. The maternal and neonatal adverse outcomes are largely due to late diagnosis [5- 7]. Hence fluctuations in uric acid levels can be used to diagnose the preeclampsia and eclampsia and treatment can be started as soon as possible.
The possible imbalance in uric acid is due to the disturbed function in the renal system and the elevated levels of uric acid can be found by dipstick test. The filtration rate is increased during the first three months of pregnancy which results into 25 to 35 percent increase in uric acid levels. On the other hand the absorption is less from proximal tube which affects the aforementioned condition. Amino acids are the essential component for fetal growth [8-12]. Uric acid prohibits the supply of amino acid to the growing fetus via placenta and thus affecting growth and development of the fetus. Increased levels of uric acid also have inflammatory impact on the blood vessels which restrict the flow of oxygen and nutrition to the growing fetus. Hence complications like intrauterine growth restrictions and so on can be seen.
Search strategy
Using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, the current comprehensive review addressed the function of serum uric acid and their relationship with the diagnosis of various clinical diseases. For works published up to June 2022, the following databases were searched: PubMed/MEDLINE, Embase, Science Direct, Cochrane Library, and clinical trials site. Studies that described their findings in English were excluded from the search results. Serum uric acid was the keyword utilized for the search strategy across different databases. Based on the criteria "serum uric acid" [MeSH Terms] OR "oxidative stress" [All Fields], PubMed/MEDLINE searched for relevant articles. The Cochrane Library, a database for systematic reviews, was searched using the keywords mentioned above (serum uric acid).
Selection criteria:
Systematic reviews, randomized and non-randomized human controlled trials, as well as retrospective and prospective cohort studies were all included in the selection criteria. In women with preeclampsia and eclampsia, uric acid has been investigated as a potential biomarker of poor maternal and perinatal outcomes. Technical reports, cadaver-based research, in vitro testing, animal testing, case studies, letters to the editor, and review articles were all disregarded (Figure 1).
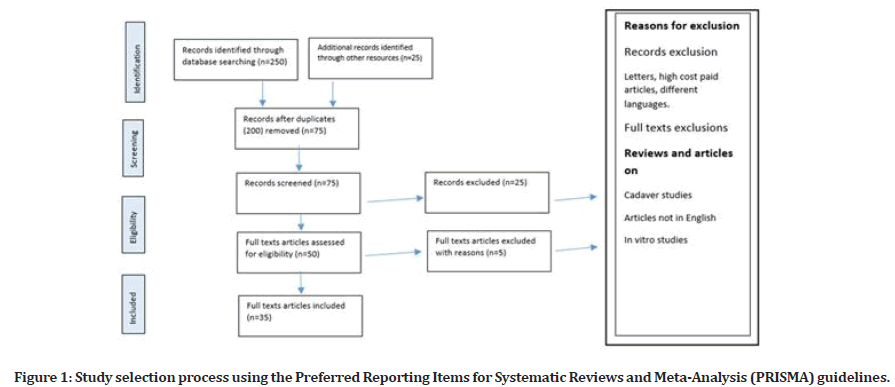
Figure 1: Study selection process using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines.
Review
Preeclampsia and eclampsia are disorders associated with pregnant women which occur with abnormalities of high blood pressure. The disorders are occurring during the pregnancy and the high blood pressure causes the shrinkage of flow of blood to the womb and fetus. Blood is the connective tissue which provides nutrients and oxygen to all parts of the body. During pregnancy, the condition is always critical as another life is budding inside the mother’s womb. For proper growth and development of the baby, it needs to be supplied with sufficient amount of nutrients and most importantly oxygen so that overall growth is ensured and outcome of pregnancy delivers healthy child. Lack of oxygen can have detrimental impact on the baby’s growth [13-15].
Eclampsia is the next stage of preeclampsia in which the symptoms become severe and pregnant women starts to develop seizures or she can go into coma. Mild hypertension during gestational period can be an occasional occurrence, but persisting condition associated with proteinuria can be termed as preeclampsia. Generally after 20 weeks, the pregnant women can develop gestational hypertension, preeclampsia and eclampsia and symptoms can dissipate in 12 weeks post pregnancy. In most of the circumstance, gestational hypertension is the common occurrence and no harmful or long term health implications can be seen on mother or fetus. During gravid condition, regular checkups for protein in urine sample can detect the preeclampsia at early stage. The reabsorption of protein fails in the kidney through glomerulus as it is damaged in the condition. Although severe and persisting hypertension can cause preterm delivery which results into several abnormalities and complications.
Pregnant women having no history of hypertension and experiencing hypertension after 20 weeks of the pregnancy can be termed as preeclampsia. The threshold blood pressure 140/90mmHg or more than associated with proteinuria termed as preeclampsia. This can result into babies delivered before 37 weeks which is termed as pre mature delivery [16-19]. Persistence of hypertension can weaken the blood vessels especially in brain causes seizures and comatose. The next stage of the complication is slipping into HELLP syndrome in which H stands from Hemolysis where the red blood cells which carries oxygen gets destroyed, EL stands for Elevated Liver enzyme like ALT and AST which is the indicator of liver damage and LP is low levels of platelets which helps in formation of blood clots in case of low platelet counts the bleeding starts. Eclampsia is not associated with preexisting brain condition and it depends upon the severity of the preeclampsia.
A cross sectional multinational observational study highlighted some risk factors regarding development of the preeclampsia and eclampsia thereafter. If the pregnant women is 35 years or older, especially when it is her first pregnancy, any kind of diabetes mellitus or renal ailments which can have compounding impact on the gravid women, Obesity, family history, autoimmune disorders along with IVF procedures all are risk factors for development of preeclampsia and eclampsia.
Preeclampsia can be classified into two categories: mild and severe. Mild preeclampsia is delineate as systolic blood pressure between 140 and 159 mmHg and diastolic blood pressure between 90 and 109 mmHg with significant proteinuria. Severe preeclampsia is defined as systolic blood pressure more than 160 and diastolic blood pressure more than 110 mmHg with significant proteinuria. Also onset of the preeclampsia before 34 weeks is known as early onset while later it is considered as late onset.
Renal system comprises pair of kidneys, pair of ureters, urinary bladder and urethra has the function to perform waste disposal from the body. The waste is in the form of urea, uric acid and ammonia. If it is accumulated for very long time then it can even prove fatal to the person affected when renal function is not properly executed.
Uric acid is produced when the molecules of the purines are broken down. The ideal uric acid concentration for males is 2.5–7.0 mg/dl while for females it is 1.5 – 6.0 mg/dl. Building up of the excess of uric acid in joints and tissues can cause serious problems.
A raised level of the uric acid is the biomarkers of the renal damage especially among the gravid women with preeclampsia. Fetal outcome pertaining to fetus can also be affected by the rise in uric acid levels during preeclampsia. In preeclampsia not only the mother suffers from various complications, the fetus has to bear the brunt of the clinical conditions like Intrauterine growth restriction (IUGR), fetal distress, perinatal death and so on are the consequences unleashed upon fetus.
Although there is correlation between maternal uric acid levels and preeclampsia. Uric acid found in gravid mothers have not just predictive role but can influence the pathogenesis of preeclampsia [20-24]. The results are fresh and needs further validation but the strong correlation can offer vital help in forming the course of diagnosis and treatment. A study compared gravid mothers having preeclampsia with those normal uric acid levels and those with raised uric acid levels. It can help to diagnose the preeclampsia at early stage so that the treatment can started accordingly. Although certain studies questioned these trend as the increased level of maternal uric acid can be possibly due to other underlying diseases such as cardiovascular diseases, hypertension, and renal ailments and so on.
In a study conducted by Martin, et al. [25] 206 eligible women having mean age 30.6 years and differentiated as having mild preeclampsia, severe preeclampsia or eclampsia. In alignment with previous findings, maternal uric acid concentration was high among group two that is gravid women having severe preeclampsia or eclampsia. 53 out of 106 fetuses suffered from Intrauterine Growth restriction due to condition of restricted blood supply. 46 instances of preterm birth were registered. 6 Fetal deaths were also registered all linked to the condition of the preeclampsia and eclampsia. Uric acid concentration was said to be good indicator of the worsening condition of the preeclampsia. Increased hypertension was seen among the gravid women having hyperuricemia [25-27].
A comparative analysis among normotensive and gravid women having hypertension was done to check the validity of the uric acid as the diagnostic tool to predict the worsening condition of the preeclampsia or eclampsia. It has been found that the uric acid concentration increases with successive trimesters and reaching the levels of 6.3 mg/dl or more after third trimester in gravid women having hypertension.
A study carried by Ugwuanyi, et al. total of 220 gravid mothers who have completed 34 weeks of pregnancy among which 110 were having normal blood pressure and other half were having hypertensive condition [28- 30]. Gestational hypertension precedes the preeclampsia condition. Interestingly the higher levels of uric acid of neonatal outcome were low birth weight of less than 2.5 kg was observed among the gravid mothers having hypertensive condition. The study confirmed the usage of the uric acid test among the hypertensive as well as preeclampsia and eclampsia patients is to be indicative test and early diagnosis and treatment can have positive outcomes with respect to mother as well as neonates.
A study carried by Koopmans CM et al[33] 120 participants were eligible to participate [31-33]. 44 of them have maternal uric acid greater than 5.5 mg/ dl likely to develop HELLP syndrome and eclampsia. Although in patients having serum uric acid levels less than 5.5 but hovering around 5.5 levels also had to face certain complications like HELLP syndrome and eclampsia. The production of the vasoconstrictors and stimulation of the inflammatory response by uric acid is yet another addition in the long list.
In a study conducted by Weerasekera DS et al[35] pregnant women having the serum uric acid levels greater than 6 mg/dl have 6 times more risk of developing severe preeclampsia which can eventually progress in to eclampsia. Preeclampsia patients have an average serum uric acid level that is higher than patients with normal blood pressure in nonproteinuric mothers. Serum uric acid levels in preeclampsia patients are related with severity of the disease [34,35].
In a study conducted by Ryu, et al. [11], In total, 140 people participated in the study; 65 preeclampsia patients and 75 women with normal pregnancies. Proteinuria, serum creatinine levels, and systolic blood pressure all showed positive correlations with serum uric acid levels in preeclamptic patients, but not platelet count. In comparison to individuals with full-term labour and normal birth weight, serum uric acid levels were significantly higher in patients with preterm labour and low birth weight.
In a study conducted by Ngeri, et al. [8], 190 women participated in the trial, 95 of whom were preeclamptic and 95 of whom were normotensive in the third trimester (28-36 weeks GA). Acute renal damage and blood uric acid levels at recruitment are significantly correlated. In comparison to preeclamptic women with normal blood uric acid levels, those who were hyperuricaemic had a greater percentage of AKI. Additionally, AKI was 3.24 times more common in preeclamptic women with hyperuricaemia compared to preeclamptic women with normal serum uric acid. AKI and mean blood uric acid levels at recruitment were statistically significantly correlated. Compared to preeclamptic women without AKI, preeclamptic women with AKI exhibited higher serum uric acid levels.
Conclusion
All the studies more or less conclude that the uric acid is effective in detection of the preeclampsia and eclampsia at early stage so that the treatment course can be initiated early. However mild to moderate preeclampsia can be falsely considered as occasional gestational hypertensive disorder and can be ignored. From the first trimester, the elevated levels of the uric acid start to show up due to maternal anatomical activity and constant monitoring is needed along with pairing of symptoms with it. The focus must be on to prohibit the preeclampsia to develop into eclampsia which can be quite difficult to manage. The fall out impact can be hazardous for both, mother as well as neonates. Other bio indicators such as low level of calcium or hypocalcemia, low APGAR score, detection of HELLP syndrome can be matched with the hyperuricemia and diagnosis can be made. The maternal and neonatal fatal clinical outcome is majorly due to the late detection and delayed treatment of preeclampsia and eclampsia which gives less room to maneuver for the health care professionals.
References
- Talaulikar VS, Shehata H. Uric acid: Is it time to give up routine testing in management of pre-eclampsia? Obstet Med 2012; 5:119-23.
- Mador ES, Pam IC, Isichei CO. Uric acid: A hypothetical cause of preeclampsia-eclampsia. Niger J Med 2013; 54:362.
- Kang DH, Finch J, Nakagawa T, et al. Uric acid, endothelial dysfunction and pre-eclampsia: searching for a pathogenetic link. J Clin Hypertens 2004; 22:229-35.
- Bainbridge SA, Roberts JM. Uric acid as a pathogenic factor in preeclampsia. Placenta 2008; 29:67-72.
- Livingston JR, Payne B, Brown M, et al. Uric acid as a predictor of adverse maternal and perinatal outcomes in women hospitalized with preeclampsia. J Obstet Gynaecol Can 2014; 36:870-877.
- Bellos I, Pergialiotis V, Loutradis D, et al. The prognostic role of serum uric acid levels in preeclampsia: A meta‐analysis. J Clin Hypertens 2020; 22:826-834.
- Akahori Y, Masuyama H, Hiramatsu Y. The correlation of maternal uric acid concentration with small-for-gestational-age fetuses in normotensive pregnant women. Gynecol Obstet 2012; 73:162-167.
- Ngeri B, Awoyesuku PA, Ohaka C, et al. Serum uric acid as a prognostic marker for preeclampsia at a tertiary hospital in Port Harcourt, Nigeria. Int J Reprod Contracept Obstet Gynecol 2022; 11:1862.
- Bellomo G. Serum uric acid and pre-eclampsia: An update. Expert Rev Cardiovasc Ther 2012; 10:701-705.
- Madaan S, Jaiswal A, Acharya N, et al. Role of salivary uric acid versus serum uric acid in predicting maternal complications of pre-eclampsia in a rural hospital in central india: a two-year, cross-sectional study. Cureus 2022; 14.
- Ryu A, Cho NJ, Kim YS, et al. Predictive value of serum uric acid levels for adverse perinatal outcomes in preeclampsia. Medicine 2019; 98.
- Pecoraro V, Trenti T. Predictive value of serum uric acid levels for adverse maternal and perinatal outcomes in pregnant women with high blood pressure. A systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol 2020; 252:447-454.
- Di X, Mai H, Zheng Z, et al. Neuroimaging findings in women who develop neurologic symptoms in severe preeclampsia with or without eclampsia. J Hypertens 2018; 41:598-604.
- Ayankunle OM, Adeniyi AA, Adewara OE, et al. Maternal serum uric acid: A reliable prognostic indicator of foetal outcome among pre-eclamptic patients in a low resource setting. J Matern Fetal Neonatal Med 2022; 35:7695-700.
- Fischer RL, Bianculli KW, Hediger ML, et al. Maternal serum uric acid levels in twin gestations. Ob Gyn 1995; 85:60-64.
- Asgharnia M, Mirblouk F, Kazemi S, et al. Maternal serum uric acid level and maternal and neonatal complications in preeclamptic women: A cross-sectional study. Int J Reprod Biomed 2017; 15:583.
- Zhao J, Zheng DY, Yang JM, et al. Maternal serum uric acid concentration is associated with the expression of tumour necrosis factor-α and intercellular adhesion molecule-1 in patients with preeclampsia. J Hum Hypertens 2016; 30:456-462.
- Le TM, Nguyen LH, Phan NL, et al. Maternal serum uric acid concentration and pregnancy outcomes in women with pre‐eclampsia/eclampsia. Int J Gynaecol Obstet 2019; 144:21-26.
- Kumar N, Singh AK. Maternal serum uric acid and calcium as predictors of hypertensive disorder of pregnancy: a case control study. Taiwan J Obstet Gynecol 2019; 58:244-250.
- Pasyar S, Wilson LM, Pudwell J, et al. Investigating the diagnostic capacity of uric acid in the occurrence of preeclampsia. Pregnancy Hypertension 2020; 19:106-111.
- Khaliq OP, Konoshita T, Moodely J, et al. Gene polymorphisms of uric acid are associated with pre-eclampsia in South Africans of African ancestry. Hypertension in Pregnancy 2020; 39:103-116.
- Jummaat F, Adnan AS, Ab Hamid SA, et al. Foetal and maternal outcomes in hyperuricaemia pre-eclampsia patients in Hospital Universiti Sains Malaysia. J Obstet Gynaecol 2021; 41:38-43.
- Laughon SK, Catov J, Powers RW, et al. First trimester uric acid and adverse pregnancy outcomes. Am J Hypertens 2011; 24:489-495.
- Cohen SB, Kreiser D, Erez I, et al. Effect of fetal number on maternal serum uric acid concentration. Am J Perinatol 2002; 19:291-296.
- Martin AC, Brown MA. Could uric acid have a pathogenic role in pre-eclampsia? Nat Rev Nephrol 2010; 6:744-748.
- Rothenbacher D, Braig S, Logan CA, et al. Association of maternal uric acid and cystatin C serum concentrations with maternal and neonatal cardiovascular risk markers and neonatal body composition: The Ulm SPATZ Health Study. Plos One 2018; 13:0200470.
- Agarwal V, Gupta BK, Vishnu A, et al. Association of lipid profile and uric acid with pre-eclampsia of third trimester in nullipara women. J Clin Diagnostic Res 2014; 8:CC04.
- Pereira KN, Knoppka CK, Da Silva JE. Association between uric acid and severity of pre-eclampsia. Clin Lab 2014; 60:309-314.
- Ugwuanyi RU, Chiege IM, Agwu FE, et al. Association between serum uric acid levels and perinatal outcome in women with preeclampsia. Obstet Gynecol Int 2021.
- Nori W, Hamed RM, Roomi AB, et al. Alpha-1antitrypsin in pre-eclampsia; from a clinical perspective. J Pak Med Assoc 2021; 71.
- Thangaratinam S, Ismail KM, Sharp S, et al. Accuracy of serum uric acid in predicting complications of pre‐eclampsia: A systematic review. Int J Obstet Gynaecol 2006; 113:369-378.
- Cnossen JS, de Ruyter-Hanhijärvi H, van der Post JA, et al. Accuracy of serum uric acid determination in predicting pre-eclampsia: A systematic review3-33. Acta Obstet Gynecol Scand 2006; 85:519-525.
- Koopmans CM, van Pampus MG, Groen H, et al. Accuracy of serum uric acid as a predictive test for maternal complications in pre-eclampsia: Bivariate meta-analysis and decision analysis. Eur J Obstet Gynecol Reprod Biol 2009; 146:8-14.
- Pasaoglu H, Bulduk G, Ogus E, et al. Nitric oxide, lipid peroxides, and uric acid levels in pre-eclampsia and eclampsia. Tohoku J Exp Med 2004; 202:87-92.
- Weerasekera DS, Peiris H. The significance of serum uric acid, creatinine and urinary microprotein levels in predicting pre-eclampsia. J Obstet Gynaecol 2003; 23:17-19.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Eleti Manila Reddy, Manjusha Agrawal*, Deepika Dewani and Nidhi Goyal
Department of Obstetrics and Gynaecology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi, Wardha, Maharastra, IndiaCitation: Eleti Manila Reddy, Manjusha Agrawal, Deepika Dewani, Nidhi Goyal, Maternal Serum Uric Acid: A Reliable Prognostic Indicator of Pregnancy Outcome in Women with Preeclampsia-Eclampsia, J Res Med Dent Sci, 2023, 11 (1):61-66.
Received: 29-Dec-2022, Manuscript No. jrmds-22-78619; , Pre QC No. jrmds-22-78619(PQ); Editor assigned: 30-Dec-2022, Pre QC No. jrmds-22-78619(PQ); Reviewed: 13-Jan-2023, QC No. jrmds-22-78619(Q); Revised: 14-Jan-2023, Manuscript No. jrmds-22-78619(R); Published: 24-Jan-2023
