Review Article - (2022) Volume 10, Issue 12
âMental Health Challenges Faced by Frontline Healthcare Workers during COVID-19 Pandemicsâ
Arya Pandey* and Pramita Muntode
*Correspondence: Dr. Arya Pandey, Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed to be University), Wardha, Maharashtra, India, Email:
Abstract
The rise of COVID-19, which was announced a pandemic by WHO on March 11th, 2020 after reaching 114 countries around the world, has frightened the medical community around the world. In December 2019, the first human cases of COVID-19, caused because of a new Coronavirus later dubbed SARS-CoV-2, were identified in China. As of June 17th, 2021, roughly 3,986,701 deaths per 100,000 people had been documented due to this sickness. It causes sickness of varied degrees of severity, ranging from asymptomatic to severe discomfort and in extreme cases, death. Colds, coughs, myalgia, headaches, fevers, sore throats and anosmia are some of the most prevalent ailments. Healthcare providers have been particularly at risk for psychological distress whilst the pandemic who spent a significant time in direct contact with patients. During the epidemic, frontline personnel have faced numerous challenges, including not being able to save some patients despite their best efforts, being blamed for the crisis, being unable to manage with a restricted supply of medical equipment and so on. Also; being a crucial part of the devising and guideline providing committee, they’ve got to dig deep while analysing the situation, management and other better modalities in view of the disease process which further pushes them down the hill. In the middle of the mayhem, frontline employees have been managing patient conditions, going home with the fear of infecting their families, juggling personal and professional lives and so on. The virus has had a negative impact on human health both mentally and physically.
Keywords
Frightened, Coronavirus, Myalgia, Anosmia, Frontline employees
Introduction
The Coronavirus disease was first discovered in late January 2020 in Wuhan, China, resulting in a pandemic that defied all human efforts to contain it. People with various specialties from all over the world have been working nonstop to track down the disease's pattern and stop it from spreading. In the case of disease epidemics, health workers are known for their resiliency and serve as the first line of defence [1]. In the midst of uncertainty and turmoil, front line health personnel are tasked with the difficult task of taking care of large groups of severely unwell people [2]. Staffs faces challenges such as increased workload, dealing with new as well as frequently changing protocols and personal protective equipment, caring for patients that are very sick and fast deteriorating, and caring for co-workers that have become ill as a result of such outbreaks [3]. During this pandemic, health sector requires a multidisciplinary approach starting from nurses, doctors, helpers, lab technician etc. which depicts their varying level of exposure to the situation and thereby affecting mental health in that order. The two risk factors that are most highly predictive of long term mental health status are:
• Lack of post-trauma social support and
• Exposure to stressors during trauma recovery [4].
Most importantly, it’s the presence of relieving factors and social circle that affects the recovery of an individual exposed to such distressing situations. In addition, the extent to which HCWs have experienced social isolation is an area that has received little attention. It's made worse by their inability to hug their friends, children, and family.
Literature Review
Pathophysiology of SARS-COV-2: The SARS-CoV-2 virus primarily causes damage to the lungs, although it also affects other organs. In the first case series from Wuhan, China, signs of LRTI included fever, dry cough, and dyspnoea. There were other reports of headaches, dizziness, widespread weakness; vomiting, diarrhoea. COVID-19 symptoms are now well known to be quite broad spectrum, ranging from minor symptoms to severe hypoxia along with acute respiratory distress syndrome. The incubation period to developing ARDS is as small as 9 days, implying that the respiratory symptoms could advance rapidly. The disease has shown its potential to be fatal. A large number of patients with life threatening illnesses have died around the world. According to epidemiology, mortality rates are more in the elderly and significantly low in children. There is currently no specific therapy available, and medical management is mostly supportive.
The goal of this study is to address the psychological impact of the COVID-19 pandemic on health care professionals, with a focus on identifying which subgroups are most prone to fall prey to psychological distress, the risk and protective factors associated with mental health.
Coronaviruses are 30 kb enclosed positive sense SS-RNA viruses with an SS-RNA genome. They can infect a wide spectrum of hosts. Based on the genetic structure, they have been segregated into four genera. Only mammals are infected. Human Coronaviruses i.e. 229E and NL63 are the culprits in causation of the common cold and croup. On the other hand, Coronaviruses, include SARS-CoV-2, Middle East Respiratory Syndrome Coronavirus (MERS-CoV-2), and SARS-CoV-2.
• Attachment;
• Penetration;
• Biosynthesis;
• Maturity;
• Releases are the five steps in the virus's life cycle with the host.
Viruses enter host cells by ‘endocytosis after binding to host receptors. Viral RNA approaches the nucleus for its replication where its contents are released into the host cells. Viral proteins are made via viral mRNA biosynthesis. After the above; maturation, additional virus particles are synthesized and given out. ‘Spike’, ‘membrane’, ‘envelope’ and ‘nucleocapsid’ are the 04 structural proteins found in Coronaviruses. Spike is a transmembrane glycoprotein that is elevated from the viral surface and controls Coronavirus division and differentiation and host tropism. Spike is made up of 02 functional subunits: S1 that attaches itself to the host cell receptor, while S2 serves the purpose of fusion of the viral and cellular membranes. SARS-CoV-2 has a functional receptor called angiotensin converting enzyme 2.
This study, which focuses solely on the ‘psychological’ effects of the COVID-19 pandemic on HSCWs, can aid in determining where interventions regarding mental health, as well as organizational and systemic efforts to support their mental health, should be aiming in order to promote psychological wellbeing.
Materials and methods
Articles were searched, accessed and analysed on Google scholar using keywords like mental health, COVID-19, management and frontline workers.
Results
After going through approximately 15-20 articles, variable outcomes regarding the review study is labelled as follows: The very beginning of Coronavirus, it’s effect in different kinds of populations, psychosocial impacts, how it has been affecting the frontline workers. Keeping pace with the frequently changing guidelines and work schedules, hence striking a balance between both of them. Summarising on how different interventions can support and favour a positive outcome amidst a pandemic. Also, how it could have been a different situation if mental health was given a priority before actually having to diagnose and take care of rather than just preventing it as a primary measure.
Discussion
SARS-CoV-2 was declared a pandemic by the World Health Organization in March 2020, and it is currently affecting more than 200 nations [5]. Coronaviruses are members of Nidovirales order's Coronaviridae family. Corona refers to the virus's outer surface, which has crown like spikes; consequently, it was given the name Coronavirus [6]. Alpha, beta, gamma, and delta Coronaviruses are subgroups of the Coronavirus family. Acute Lung Injury (ALI) and Acute Respiratory Distress Syndrome (ARDS) are caused because of the SARS-CoV-2, H5N1 influenza A, H1N1 2009, and Middle East respiratory syndrome Coronavirus in short known to be MERS-CoV-2, which can lead to pulmonary failure and death. In the first fifty days of the pandemic, a new Coronavirus killed over 1800 of the population and infected over 70 thousand more in Wuhan, China's booming commercial centre. The infecting virus was identified as belonging to Corona virus family. Chinese researchers have given the virus the name 2019 new Coronavirus. The virus is known as SARS-CoV-2, and the sickness is known as ‘COVID-19’, according to the International Committee on Virus Taxonomy (ICTV) [7-9].
Coronavirus emergence and spread: A comparative examination
In Guangdong province, the population of China got infected with a virus that caused Severe Acute Respiratory Syndrome (SARS) earlier in 2003. Acute respiratory distress syndrome emerged in infected patients, who experienced pneumonia like symptoms as well as widespread alveolar destruction (ARDS). SARS began in Guangdong, China that swiftly reached the entire world, sickening over 8000 persons. Later, in 2012, two nationals of Saudi Arabia were diagnosed with the Middle East respiratory syndrome Coronavirus, a new Coronavirus that was identified as a Coronavirus and given the name Middle East Respiratory Syndrome Coronavirus (MERS-CoV-2). MERS Coronavirus caused infection in more than 2428 people, resulting in 838 deaths, according to the World Health Organization [10]. MERS-CoV-2 belongs to the ‘beta’ Coronavirus subgroup that is phylogenetically distinct from other human Coronaviruses. MERS-CoV-2 infection begins with a mild upper respiratory damage and progresses to severe form of the disease. Similar to SARS Coronavirus, patients who got infected with MERS Coronavirus developed pneumonia, which led to ARDS and renal failure. On 12 January 2020, the national health commission of china gave out further details about the epidemic, suggested viral pneumonia [11]. Furthermore, the viral infection was confirmed by the genomic sequencing. Patients with Wuhan Coronavirus induced pneumonia were initially considered to have had visited a seafood market place where live animals were sold, or had eaten contaminated animal. However, additional examination indicated that some people became infected even if they had no history of visiting a fish market. These findings revealed the virus's potential to transmit from person to person, and it was later detected in around 100 nations all around the world. The virus spreads from person to person by close contact with an individual having the infection and is exposed to coughing, sneezing, respiratory droplets/ aerosols that can permeate the human body (lungs) via inhalation.
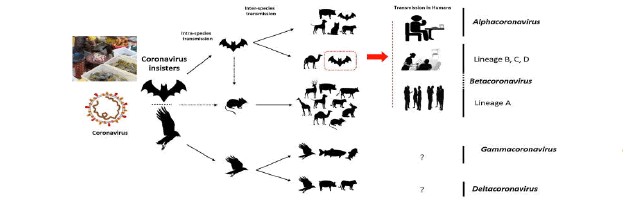
Figure 1: The key reservoirs and mode of transmission of Coronaviruses (suspected reservoirs of SARS-CoV-2 are red encircled); only α and β Coronaviruses have the ability to infect humans, the consumption of infected animal as a source of food is the major cause of animal to human transmission of the virus and due to close contact with an infected person, the virus is further transmitted to healthy persons. Dotted black arrow shows the possibility of viral transfer from bat whereas the solid black arrow represents the confirmed transfer.
The mental health challenges faced by doctors during the COVID-19 situation
Healthcare services are overburdened during health emergencies, making work life even more stressful than usual [12]. When a pandemic occurs, the number of patients in need of medical care increases dramatically, putting a strain on healthcare system and frontline doctors as well. Furthermore; doctors and nurses are at a greater risk to themselves as a result of their exposure to the sickest patients, bringing additional stress to their personal and professional lives. Another finding of the study revealed that HCWs with fewer years of work experience were more likely to have PTSD and depressive symptoms [13]. This conclusion shows that the more experienced the HCWs are, the fewer mentally upsetting incidents they report; past research backs this up [14]. It could be interpreted as the product of years of work leading to the development of resilience and adaptive coping mechanisms [15]. The risk of psychological harm is not limited to frontline HCWs; in fact, most HCWs, regardless of specialisation, have likely faced significant challenges ever since the pandemic began, which essentially includes changes in their work routines and, at times, being unable to provide the level of care they would have normally provided [16].
In order to understand the topic, some factors contributing to the mental health of the frontline workers during a pandemic are stated below:
• Biological factors: Early age, mood disorders, or any sick family member that they must care for on top of their regular duties predisposes to having additional mental burdens.
• Psychological factors: The personality qualities of healthcare providers are one of the most critical determinants of developing mental health difficulties during a pandemic. HCWs afraid of scrutiny, nervous avoidant personality traits, and avoidant coping methods are all examples of avoidant personality traits. Are more likely to develop mental health problems, whereas those with hardiness personality traits indirectly improve and directly mediate excellent mental health of the individual by lowering their stress levels. To name a few, there are social and environmental elements.
• Lack of information and insufficient communication: Lacking sufficient amount of communication with higher authorities to frontline HCWs may result in non-predictability, apprehension, a lack of information, and a sense of uncontrollability over the situation, as well as quickly changing infection control guidelines. The possibility of contracting an infection: HCWs working in high exposure locations, such as ICU isolation units, are afraid of infecting their families and loved ones.
• Social distancing: As important and crucial it is to maintain social distancing, be it a workplace or not, it has deprived the frontline warriors of the emotional support and a sense of security from their family members, colleagues and loved ones which is further decreased the threshold for keeping oneself sane amidst the pandemic.
• Job stress/occupational stress: As daunting as it already is, reduction in the number of team members; either in quarantine or in isolation that got infected while on duty, adds up to the stress. Due to the said situation, long working hours, messed up sleep cycle, frequently changing schedules, guidelines and an uncertain outcome to every decision poses a threat to mental well-being.
• Personal protective equipment related issue: Inadequate supply of PPE which being the only reliable physical barrier between the healthcare worker and patient proved to be a major hindrance in proper communication with one another and with time led to significant burnout.
• Lack of support from the company and coworkers: HCWs, particularly those who are compelled to work from home, according to the literature [17], frequently suffer from job related concerns. Furthermore, junior healthcare workers, particularly nurses and paramedics, may believe that they will be scrutinised by their superiors and chastised for any errors; that they will be scrutinised by their superiors and blamed for any and every error/mishap; and that they will require handholding and role modelling by their superiors at work.
• Misinformation and crowd behaviour: According to the literature, a pandemic caused by an unknown agent could occur and could trigger widespread fear and panic. This is frequently exacerbated by misinformation/rumour spread on social media, resulting in a panic situation in the community a "pandemic.” Many rumours and disinformation are spread on social media during the pandemic, especially in the early stages, exacerbating anxiety, sadness, and anguish among healthcare workers on the front lines.
• Being an only child: In Wuhan, this was found to be connected with sleep disruption in paediatric HCWs. Being an only child also found to be linked to higher levels of stress. In a large multicentre trial located in India and Singapore, a substantial link between somatic symptoms and poor psychological results also depicted an association. It's unclear if this was due to somatization or organic sickness, but the authors believe there was a bi-directional interaction between physical and psychological symptoms.
Managing the stress of doctors at the corporate level during an outbreak
The pandemic of COVID-19 may present a chance to improve mental health policies and services. Different national governments have implemented emergency measures, for e.g. Lockdowns, school closures, self-isolation, and limiting the number of people in public locations and at occasions such as marriage functions and funerals to avoid communal transmission of COVID-19. The guidelines, which limit human interaction and combine it with fear of infection and social media misinformation, raise false confusion along with stress/tensions among various communities.
Supporting interventions: Support high up from the government down to the family, from equipment such as PPE, mass etc. to emotional connect, a variety of input and feedback channels, and the implementation of health related choices of the society as a whole all contribute to the enhancement of mental health amongst frontline workers.
Conclusion
Although the pandemic had shaken the world thoroughly, some of the measures can help out to mitigate the impact of pandemic positively. These include encouragement and motivation intervention, recognising the health care workers efforts by the hospital managers, the government and the society, practise relaxing techniques such as meditation and yoga, provision of adequate and effective protective equipment, addressing frontline workers physical needs; for example access to healthy meals and hydration, regular rest breaks etc. can prove to be a helpful tool in boosting up the mental health of HCWs. Online webinars and workshops emphasising on how to manage physical, mental and emotional wellbeing along with a hectic and tiring schedule could be conducted. Yoga has remained the cornerstone for increasing well-being, disease risk reduction and mental and physical health despite limited public health intervention options. Yoga is a disciplined way of living that includes asanas, pranayama’s, and meditation. It makes a person aware of his or her own body, mind, thoughts, and soul. Yama (restraints) and Niyama (observances) are the foundations of Yogic doctrine. Nonviolence, truthfulness, non-stealing, moderation, and non-hoarding are among Yama's teachings, while cleanliness, contentment, self-discipline, self-study, and healthiness are among Niyama's. Patients are advised not to travel or visit a hospital during the COVID-19 pandemic unless it is an emergency or for the treatment of COVID-19 disease. As a result, the severity of the disease increases and it becomes a cumbersome task for the doctors to manage such patients. In light of this, the ministry of health and family welfare, in collaboration with NITI Aayog, released telemedicine rules in the country, granting telemedicine statutory status. This resulted in the creation of "Tele-psychiatry Operational Guidelines (TOG) 2020," which can be used for providing Tele-psychiatric services in various settings.
References
- Otu A, Charles CH, Yaya S. Mental health and psychosocial well-being during the COVID-19 pandemic: The invisible elephant in the room. Int J of Mental Health Syst 2020; 14:1-5.
- Liu S, Yang L, Zhang C, et al. Gender differences in mental health problems of healthcare workers during the Coronavirus disease 2019 outbreak. J Psychiatr Res 2021; 137:393-400.
- Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care 2020; 9:241-247.
- Greenberg N. Mental health of health care workers in the COVID-19 era. Nat Rev Nephrol 2020; 16:425-426.
- Shereen MA, Khan S, Kazmi A, et al. COVID‑19 infection: Emergence, transmission and characteristics of human Coronaviruses. J Adv Res 2020; 24:91-98.
- Cui J, Li F, Shi ZL. Origin and evolution of pathogenic Coronaviruses. Nat Rev Microbiol 2019; 17:181-192.
- Lai CC, Shih TP, Ko WC, et al. Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-CoV-2) and Corona Virus Disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents 2020; 55:105924.
- World Health Organization (WHO). Laboratory testing for Coronavirus disease 2019 (COVID-19) in suspected human cases: Interim guidance, 2 March 2020. 2020.
- Rahman A, Sarkar A. Risk factors for fatal Middle East respiratory syndrome coronavirus infections in Saudi Arabia: Analysis of the WHO line list, 2013–2018. Am J Public Health 2019; 109:1288-1293.
- Wang C, Horby PW, Hayden FG, et al. A novel Coronavirus outbreak of global health concern. Lancet 2020; 395:470-473.
- Tam CWT, Pang EP, Lam LC, et al. Severe Acute Respiratory Syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers. Psychol Med 2004; 34:1197-1204.
- Chatzittofis A, Karanikola M, Michailidou K, et al. Impact of the COVID-19 pandemic on the mental health of healthcare workers. Int J Environ Res Public Health 2021; 18:1435.
- Carmassi C, Foghi C, Cordone A, et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID-19 pandemic. Psychiatry Res 2020; 292:113312.
- Nickell LA, Crighton EJ, Tracy CS, et al. Psychosocial effects of SARS on hospital staff: Survey of a large tertiary care institution. CMAJ 2004; 170:793–798.
- De Kock J, Latham H, Leslie S, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health 2021; 21:1-8.
- National Institute of Mental Health and Neurosciences (NIMHNS). Guidelines of managing mental illness in hospital settings during COVID-19. Ministry of health and family welfare, India, 2020.
Author Info
Arya Pandey* and Pramita Muntode
Department of Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed to be University), Wardha, Maharashtra, IndiaCitation: Arya Pandey, Pramita Muntode, “Mental Health Challenges Faced by Frontline Healthcare Workers during COVID-19 Pandemics”, J Res Med Dent Sci, 2022, 10 (12): 072-076.
Received: 20-Sep-2022, Manuscript No. JRMDS-22-77325 ; , Pre QC No. JRMDS-22-77325(PQ) ; Editor assigned: 23-Oct-2022, Pre QC No. JRMDS-22-77325(PQ) ; Reviewed: 07-Oct-2022, QC No. JRMDS-22-77325 ; Revised: 12-Dec-2022, Manuscript No. JRMDS-22-77325(R); Published: 19-Dec-2022
