Research - (2022) Volume 10, Issue 3
Metastasis of Primary Malignant Melanoma of Cervix in Brain: A Tertiary Care Center, Maharashtra
Avadh Kishor Tyagi*, KM Hiwale and Sunita Vagha
*Correspondence: Avadh Kishor Tyagi, Department of Pathology, India, Email:
Abstract
Background: Malignant Melanoma is primarily occurs in skin, mucous membrane and choroid but Primary Malignant Melanoma of Cervix (PMMC) is extremely rare due to lack of melanocytes in cervix. That’s why metastasis of Primary Malignant Melanoma of Cervix (PMMC) is extremely uncommon condition. Case presentation: In this study, a 66-years old female came to tertiary health centers OPD with complain of occipital headache, vertigo from 4 or 5 days and history of being operated for primary malignant melanoma of cervix 2 years back. On histopathological examination, the left cerebellar lesion was notice to bemetastasis of Primary Malignant Melanoma of Cervix and the lesion had metastasized in other region of brain also. Conclusion: The Primary Malignant Melanoma of Cervix very rare condition with extremely poor prognosis. Early diagnosis, wide local surgical excision with pre and post-operative adjuvant therapy are play important role in increase of patients survival. This case report aims to improve information about uncommon tumor of cervix.
Keywords
Poor prognosis, Metastasis, Primary malignant melanoma of cervix, Brain, Immunohistochemistry
Introduction
Malignant melanoma is mainly found in the skin, choroid, mucous membrane and this disease arises from melanocytes that produce melanin [1]. It rarely develops in genital tract, mostly vulva and vagina of women. Lack of melanocytes in cervical mucous membrane and brain is the cause of its extreme rarity, with difficulty to diagnose and poor prognosis [2-4]. Ultraviolet rays from sunlight are most common cause of melanoma. Other major risk factors are fair skin, unusual mole, congenital nevi, family history and drugs like psoralen, light therapy, polyvinyl chloride and pesticide exposure [1].
There are various form of Malignant Melanoma like Superficial spreading melanoma, Acral lentiginous melanoma, Nodular melanoma, and Lentigo maligna [5].
Malignant Melanoma is 19th most prevalent cancer in the world. Incidence of it is 2.8-3.1 per 100000 [6].Genital malignant melanoma is very rare upto 3-7% of all melanoma. Incidence of Primary Malignant Melanoma of Cervix is five times lower than genital tract malignant melanoma of vulva and vagina [2-4]. It mostly spreads locally and by lymphatics. But it can metastasize to distant organ like liver, lungs and bones. Brain metastasis for Primary Malignant Melanoma of Cervix is extremely uncommon, occurring in 0.4 to 2.3% of all patients. Due to its rareness, no prospective trials studies have been conducted to examine treatment approach, prognostic factor and survival rate [7,8]. In this report, we describe one such case of metastasis of Primary Malignant Melanoma of Cervix in brain.
Case History
A 66 years old female came to a tertiary care centre in Maharashtra with chief complaint of occipital headache (on and off type), vertigo (on and off type) and generalized weakness since 5 days with history of being undergone radical hysterectomy for primary malignant melanoma of cervix one year back. Clinical examination revealed positive signs for Rombergs test and Nystagmus.
Contrast MRI finding revealed peripherally enhancing cystic lesion with small solid component in left cerebellar hemisphere, suspicious of haemorrhagic metastatic deposits. Postoperatively, the tumor was sent for histopathological examination.
Grossly, black pigmented, multiple, irregular tissue pieces, firm in consistency aggregating 2.5x1.5x1 cm were received. On cut section, homogenous jet black areas were identified.
Microscopical features show polygonal cells along with spindle cells arranged in fascicles, sheets and singly which contain round nuclei having prominent nucleoli that shifts chromatin material towards the nuclear membrane and dusty pigmented cytoplasm (Figures 1 and Figure 2).
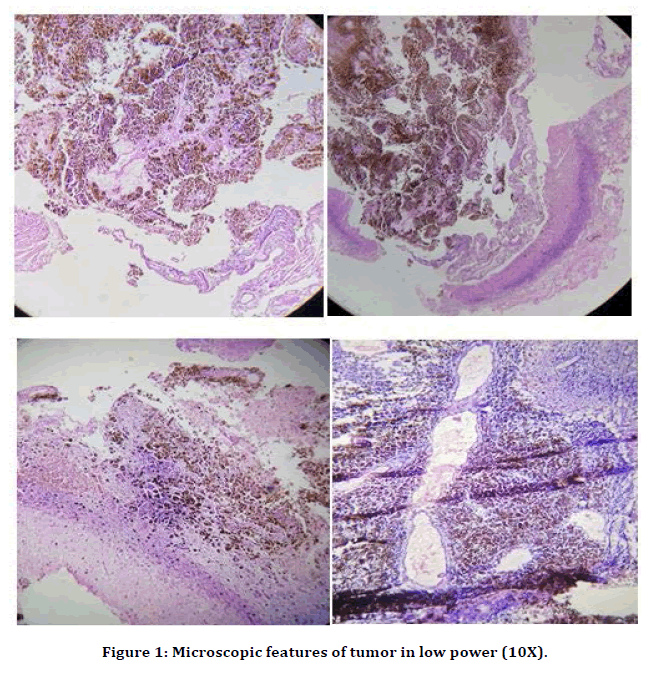
Figure 1. Microscopic features of tumor in low power (10X).
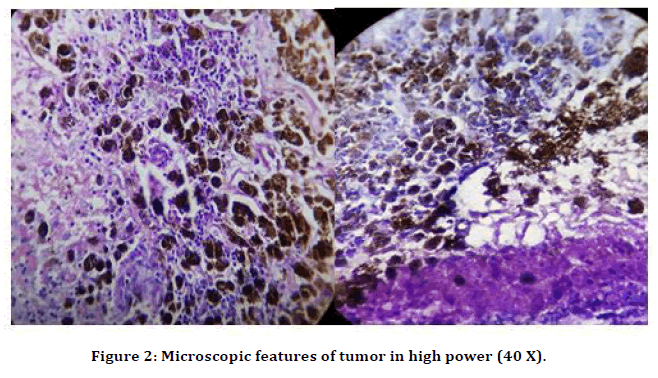
Figure 2. Microscopic features of tumor in high power (40 X).
Final Diagnosis
Deposits of primary malignant melanoma of cervix in left cerebellar hemisphere.
Discussion
Melanoma is extremely malignant tumor which originates from melanocytes. Incidence of melanoma has increased in the previous decade. It is primarily occurs in skin, mucous membrane and choroid but it may be occur any other site in body. Primary malignant melanoma of genital region is very uncommon, with3 to 7%incidence of entire melanoma cases [9,10]. Incidence of Primary Malignant Melanoma of cervix is five times lower than genital melanoma. So furthermore, metastasis of primary malignant melanoma in brain is extremely rare entity [2-4].
The definitive causative factor of melanoma remains anonymous but sun light (ultraviolet radiation) is acknowledge as a main cause [1]. It is mostly metastasizes locally to lymph nodes. It can be metastasize by hematogenous route, to distant organ like liver, lungs, bone and brain [7,8]. Histopathology (H & E stain), Immunohistochemistry and electron microscopy are considered as standard diagnostic tools for melanoma. Important diagnostic features of melanoma are : i) Pleomorphism of tumor cells ii) Nuclear atypia iii) Melanin pigment granules, scattered intracellular (approximately 6 to 10% cases of melanoma does not show melanin pigment granules, known as amelanotic melanoma) [11] iv) HMB-45, Melan A and S-100 IHC markers are positive for melanoma v) On electron microscopy, melanosomes are seen [13]. Sometimes on basis of histopathology, diagnoses are very challenging and feel necessity for IHC markers. S-100 positive result is a good indicator for melanoma and it should confirm by Melan-A & HMB-45 markers. In our study, primary symptoms were occipital headache, vertigo and generalized weakness with previous history of hysterectomy for primary malignant melanoma of cervix. After the clinical examination and histopathological examination, it was found that the female had metastatic deposits of primary malignant melanoma of cervix in brain. Main treatment is surgical excision (wide local) with a combo of radiotherapy, chemotherapy and immune therapy [8,14]. Chemotherapy (cisplatin, dacabazine, taxol and temozolomide) is commonly as pre and post-operative adjuvant therapy. When lesions are unremovable than radiotherapy may be used [15,16]. It is observed that chemotherapy with immunotherapy may boost efficacy of patients treatment [17,18].
Conclusion
Metastasis of the Primary Malignant Melanoma of Cervix in brain is a extremely uncommon condition, with poor prognosis. Although surgery is treatment of choice, but management may differ with different individual symptoms. Proper wide local surgical excision with pre and post adjuvant therapy (chemotherapy and radiotherapy) have play very important role in survival of patient and pathological confirmation.
References
- HE Y, Mou J, Luo D, et al. Primary malignant melanoma of the breast: A case report and review of the literature. Oncol Letters 2014; 8:238-240.
- Gupta S, Sodhani P, Jain S. Primary malignant melanoma of uterine cervix: A rare entity diagnosed on fine needle aspiration cytology: Report of a case. Cytopathol 2003; 14:153-6.
- Chang AE, Karnell LH, Menck HR. The national cancer data base report on cutaneous and noncutaneous melanoma: A summary of 84,836 cases from the past decade. Cancer 1998; 83:1664-1678.
- McLaughlin CC, Wu XC, Jemal A, et al. Incidence of noncutaneous melanomas in the U.S. Cancer 2005; 103:1000-7.
- https://www.elsevier.com/books/rosai-and-ackermans-surgical-pathology-10e/rosai/978-81-312-2984-2
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127:2893-917.
- Lefkowitz D, Asconape J, Biller J. Intracranial metastases from carcinoma of the cervix. Southern Med J 1983; 76:519-21.
- Amita M, Sudeep G, Rekha W, et al. Brain metastasis from cervical carcinoma--a case report. Med Gen Med 2005; 7:26.
- Kurul S, Taş F, Büyükbabani N, et al. Different manifestations of malignant melanoma in the breast: a report of 12 cases and a review of the literature. Jap J Clin Oncol 2005; 35:202-206.
- Alzaraa A, Sharma N. Primary cutaneous melanoma of the breast: A case report. Cases J 2008; 1:1-3.
- Duggal R, Srinivasan R. Primary amelanotic melanoma of the cervix: Case report with review of literature. J Gynecol Oncol 2010; 21:199-202.
- Bonetti F, Pea M, Martignoni G, et al. False-positive immunostaining of normal epithelia and carcinomas with ascites fluid preparations of antimelanoma monoclonal antibody HMB45. Am J Clin Pathol 1991; 95:454-459.
- Taatjes DJ, Arendash-Durand B, Von Turkovich M, et al. HMB-45 antibody demonstrates melanosome specificity by immunoelectron microscopy. Arch Pathol Labora Med 1993; 117:264-268.
- Lee AH. Use of immunohistochemistry in the diagnosis of problematic breast lesions. J Clin Pathol 2013; 66:471-477.
- Lee RJ, Gibbs JF, Proulx GM, et al. Nodal basin recurrence following lymph node dissection for melanoma: implications for adjuvant radiotherapy. Int J Radiat Oncol Biol Phys 2000; 46:467-474.
- Calabro A, Singletary SE, Balch CM. Patterns of relapse in 1001 consecutive patients with melanoma nodal metastases. Arch Surg 1989; 124:1051-5.
- Thompson JF, Scolyer RA, Kefford RF. Cutaneous melanoma. Lancet 2005; 365:687-701.
- Hauschild A, Weichenthal M, Rass K, et al. Efficacy of low-dose interferon α2a 18 versus 60 months of treatment in patients with primary melanoma of >=1.5 mm tumor thickness: Results of a randomized phase III DeCOG trial. J Clin Oncol 2010; 28:841-846.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Avadh Kishor Tyagi*, KM Hiwale and Sunita Vagha
Department of Pathology, JNMC (DMIMS), Sawangi, Maharashtra, IndiaReceived: 10-Feb-2022, Manuscript No. JRMDS-22-54082; , Pre QC No. JRMDS-22-54082 (PQ); Editor assigned: 11-Feb-2022, Pre QC No. JRMDS-22-54082 (PQ); Reviewed: 25-Feb-2022, QC No. JRMDS-22-54082; Revised: 04-Mar-2022, Manuscript No. JRMDS-22-54082 (R); Published: 11-Mar-2022
