Research - (2022) Volume 10, Issue 7
Most Preferred Bleaching Agent for Vital and Non Vital Bleaching among Indian Dentist-Retrospective Study
Nivethitha R and Subash Sharma*
*Correspondence: Subash Sharma, Department of Conservative Dentistry, Saveetha Dental College & Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India, Email:
Abstract
Introduction: Bleaching, although not new to dentistry, has gained much popularity in recent years. It is the most preferred conservative method to lighten discolored teeth. The main goal of tooth bleaching is to whiten tooth tissues using oxidizing chemical agents that act both in enamel and dentin. Because tooth shade depends on the composition of tooth tissues, severe chemical, mechanical and biological changes can damage the esthetic equilibrium of the smile. Bleaching tooth structure is possible due to the noninvasive nature of the bleaching systems that offer treatment options capable of fulfilling expectations of the most demanding patients. The purpose of this study was to evaluate the most preferred bleaching agent for vital and non-vital agents among Indian dentists. Materials and methods: A total of 160 patients were included in the present study. Demographic details like age, gender, types of bleaching, bleaching agent of all patients were recorded. All the data was entered on the excel sheet. Data was analysed by the SPSS software version. Results: Out of 160 patients, 70% were male and 30% were females. 15-25 yrs. were the most prevalent age group reporting to hospital for bleaching treatment. 65.63% of patients preferred vital bleaching techniques among Indian dentists. 33.74% sodium perborate was the most preferred bleaching agent used among Indian dentists for non-vital bleaching. Conclusion: Within the limitation of the study, sodium perborate was the most preferred bleaching agent used for non-vital bleaching. 35% H2O2 were the most preferred bleaching agent used for vital bleaching techniques.
Keywords
Cardiovascular disease, Communicable disease, Dietary factors
Introduction
Discolored anterior teeth are often perceived as an esthetic detraction. Because of the growing need for beautiful, white teeth and the establishment of esthetic treatment methods, the bleaching of nonvital teeth has become increasingly important in recent years. In the middle of the 19th century, the first attempts were made to lighten discolored teeth using various bleaching agents. Initially, oxalic acid was used, until the toothbleaching effect of hydrogen peroxide was discovered in 1884 [1].
Discolorations can be differentiated into extrinsic or intrinsic origin. External discolorations result from the consumption of certain food, beverages or tobacco products as well as from inadequate oral hygiene or certain oral hygiene products. Furthermore, a thinning of the dental enamel during aging also darkens the tooth [2]. An intrinsic discoloration is defined as one with its origin within the pulp chamber. This includes hemorrhage, necrosis, calcification, and iatrogenic discoloration due to dental treatment. Hemorrhage of the pulp is the most common etiology of dis- coloration after trauma [3].
Bleaching is the most preferred conservative method to lighten discolored teeth [4]. Bleaching agents contain either hydrogen peroxide or carbamide peroxide. One of the popular bleaching techniques is night guard bleaching that utilizes 10% CP in a customized tray that is worn by the patient at night [5]. CP is formed from hydrogen peroxide and urea and about one-third of CP is released as hydrogen peroxide. The color change in enamel and dentin is the result of penetration of hydrogen peroxide through the enamel and break down of high molecular weight organic molecule into simpler low molecular weight molecules with lesser color reflectance [6]. However, its action is not restricted and could also contribute to protein damage and mineral loss [7].
Tooth bleaching agents are classified by the Federal Health Office of Switzerland and the Medications Institute Swiss medic as cosmetics. Hydrogen peroxide (H2O2) is an effective bleaching agent [8]. Nevertheless, high concentrations of H2O2 (30%) should be used in order to avoid increasing the risk of root resorption. Sodium perborate occurs in the form of mono-, tri- (NaBO2•H2O2• 3H2O) or tetra hydrate. Upon adding water, H2O2 is released. The bleaching effect is not weakened if sodium perborate is mixed with water instead of hydrogen peroxide [9,10].
Currently, there are very few studies on the use of sodium per carbonate (2Na2CO3 • H2O2). This agent was long ignored, as its stability during storage was very poor. An in vitro study found the bleaching effect of sodium per carbonate (mixed with water) to be similar to that of 30% hydrogen peroxide [11]. However, clinical studies are still lacking. Carbamide peroxide (CH4N2O • H2O2) is an organic compound containing hydrogen peroxide and urea. In an in vitro test, carbamide peroxide showed a bleaching ability equal to that of hydrogen peroxide [12]. Our team has extensive knowledge and research experience that has translate into high quality publications [13-32].
The aim of this study was to evaluate the most preferred bleaching agent for vital and non-vital agents among Indian dentists.
Materials and Methods
Study designs and study setting
The present study was conducted in a university setting [Saveetha dental college and hospitals, Chennai, India]. Thus the data available is of patients from the same geographic location and have similar ethnicity. The retrospective study was carried out with the help of digital case records of 160 patients who reported to the hospital. Ethical clearance to conduct this study was obtained from the Scientific Review Board of the hospital.
Sampling
Data of 160 patients [70 males and 30 females] were reviewed and then extracted. All patients with types of age, gender, bleaching agent, types of bleaching. Only relevant data was included to minimize sampling bias. Simple random sampling method was carried out. Cross verification of data for error was carried out. Cross verification of data for error was done by presence of additional reviewer and by photographic evaluation. Incomplete data collection was excluded from the study.
Data collection
A single calibrated examiner evaluated the digital case records of patients who reported to Saveetha Dental College from June 2020 to March 2021. For the present study, inclusion criteria were data of patients with type of bleaching. Data obtained were age, gender, type of bleaching , bleaching agent. All obtained data were tabulated into Microsoft excel documents.
Statistical analysis
The collected data was tabulated and analysed with Statistical Package for Social Sciences for Windows, version 20.0 [SPSS Inc., Vancouver style] and results were obtained. Categorical variables were expressed in frequency and percentage. Chi square test was used to test association between categorical variables. Chi square tests were carried out using age, gender and as independent variables and dependent variables. The statistical analysis was done by pearson chi square test. P value < 0.05 was considered statistically significant.
Results
Bar graph shows the frequency distribution of gender of the patients X axis denotes gender and Y axis denotes the percentage of patients participating in this study. From this study we observed that 70% were male and 30% were females (Figure 1). Bar graph shows frequency distribution of age of the patients. X axis denotes age groups and Y axis denotes the percentage of patients participating in this study. From this study we observed that (55.63% - 15 to 25 yrs.), (32.50% - 26 to 35 yrs.), (5.63% - 36 to 45 yrs.), (6.25% - 46 to 55 yrs.). 15-25 yrs. were the most prevalent age group participating in this study (Figure 2). Bar graph shows frequency distribution of type of bleaching in this study. X axis denotes types of bleaching and Y axis denotes the percentage of patients participating in this study. From this study we observed that 65.63% were vital bleaching, 34.38% were non vital bleaching. 65.63% were the most preferred vital bleaching technique among Indian dentists (Figure 3).
Figure 1: Bar graph shows frequency distribution of gender of the patients X axis denotes gender and Y axis denotes the percentage of patients participating in this study. From this study we observed that 70% were male and 30% were females.
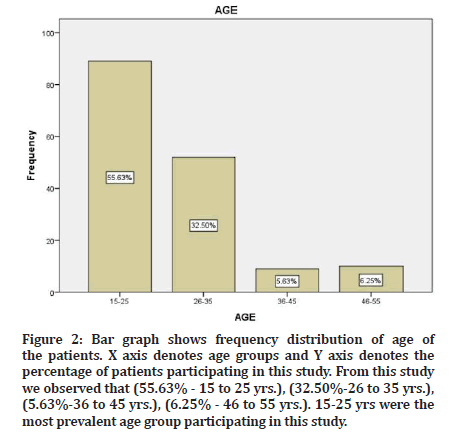
Figure 2: Bar graph shows frequency distribution of age of the patients. X axis denotes age groups and Y axis denotes the percentage of patients participating in this study. From this study we observed that (55.63% - 15 to 25 yrs.), (32.50%-26 to 35 yrs.), (5.63%-36 to 45 yrs.), (6.25% - 46 to 55 yrs.). 15-25 yrs were the most prevalent age group participating in this study.
Figure 3: Bar graph shows frequency distribution of type of bleaching in this study. X axis denotes types of bleaching and Y axis denotes the percentage of patients participating in this study. From this study we observed that 65.63% were vital bleaching, 34.38% were non vital bleaching. 65.63% of patients preferred vital bleaching techniques among Indian dentists.
Bar graph shows frequency distribution of bleaching agents in this study. X axis denotes bleaching agent and Y axis denotes the percentage of patients participating in this study. From this study we observed that 33.74% - sodium perborate, 21.25% - sodium perborate 10% H202, 22% - 35% H202, 10.63%-Mcinnes, 8.75%-sodium perborate supercool, 3.13% - 10% H2O2, 2.50% - opalescence. 33.74% were the most preferred bleaching agent among Indian dentists (Figure 4). Bar graph showing the association between type of bleaching and bleaching agent. The X axis represents the type of bleaching and Y axis represents the bleaching agent. Sodium perborate, the most preferred bleaching agent used for non-vital bleaching. 35% H2O2 were the most preferred bleaching agent used for vital bleaching techniques. Chi-square test was done and the association between types of bleaching and bleaching agent was found to be statistically significant. Pearson’s Chi-square value=25.591, df=6, p value 0.00 (>0.05).
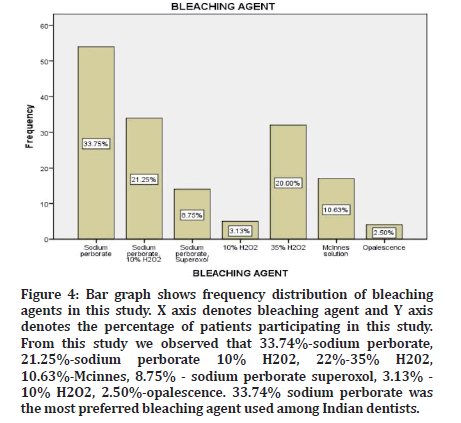
Figure 4: Bar graph shows frequency distribution of bleaching agents in this study. X axis denotes bleaching agent and Y axis denotes the percentage of patients participating in this study. From this study we observed that 33.74%-sodium perborate, 21.25%-sodium perborate 10% H202, 22%-35% H202, 10.63%-Mcinnes, 8.75% - sodium perborate superoxol, 3.13% - 10% H2O2, 2.50%-opalescence. 33.74% sodium perborate was the most preferred bleaching agent used among Indian dentists.
Discussion
The present study was conducted among 160 patients. 70% were male and 30% female. In this study, 33.74% - sodium perborate was the most preferred bleaching agent used among Indian dentists. Sodium perborate, the most preferred bleaching agent used for non-vital bleaching. 35% H2O2 were the most preferred bleaching agent used for vital bleaching techniques. Weiger reported the similar evidence that sodium perborate, which is frequently used in bleaching of non-vital teeth, decomposes in hydrogen peroxide after contact with water, releasing nascent oxygen [33].
Pearson reported the similar evidence that bleaching techniques were used for vital teeth by means of oxalic acid or pyrozone later with hydrogen peroxide, the use of concentrated hydrogen peroxide with a heating instrument was regarded as an acceptable method in dental clinics [34]. Sodium perborate release oxygen should be synergistic and more effective [35]. Rotstein, et al. [25] reported that sodium perborate with water presented similar effectiveness of bleaching compared to other bleaching materials, and also combination with 30% hydrogen peroxide or water resulted in similar esthetic results after bleaching [36].
Conclusion
Within the limitation of the study, sodium perborate was the most preferred bleaching agent used for non-vital bleaching. 35% H2O2 were the most preferred bleaching agent used for vital bleaching techniques. The limitations of the study include short sample size, single centered study and don’t represent ethnic groups or populations. The study should be carried out in larger populations.
Authors Contribution
Nivethitha R: Literature search, data collection, analysis, manuscript drafting.
Subash Sharma: Data verification, manuscript drafting.
Acknowledgement
The authors would thank all the participants for their valuable support and authors thank the dental institution for the support to conduct.
Conflict of Interest
All the authors declare that there was no conflict of interest in present study.
Source of Funding
The present project is supported/funding/sponsored by the
✔ Saveetha Institute of Medical and Technical Sciences, Saveetha Dental College and Hospitals, Saveetha University, India.
✔Pavithra Harvesters and Earth Movers.
References
- Agarwal M, Narang A, Awadhiya S, et al. Nonvital bleaching: A case series on whitening procedure for discolored endodontically treated teeth. Int J Prosthod Restorative Dent 2018; 8:28–31.
- Burgt TP van der, van der Burgt TP, Plasschaert AJM. Tooth discoloration induced by dental materials. Oral Surg Oral Med Oral Pathol 1985; 60:666–669.
- Watts A, Addy M. Tooth discolouration and staining: A review of the literature. Br Dent J 2001; 190:309–316.
- Leonard RH. Nightguard vital bleaching. Tooth Whitening Techniques 2017; 285–294.
- Poyser NJ, Kelleher MGD, Briggs PFA. Managing discolored non-vital teeth: The inside/outside bleaching technique. Dent Update 2004; 31:204–214.
- Garber DA. Dentist-monitored bleaching: A discussion of combination and laser bleaching. J Am Dent Assoc 1997; 128:26S-30S.
- Rotstein I, Dankner E, Goldman A, et al. Histochemical analysis of dental hard tissues following bleaching. J Endod 1996; 22:23–25.
- Attin T, Paqué F, Ajam F, et al. Review of the current status of tooth whitening with the walking bleach technique. Int Endod J 2003; 36:313–329.
- Arı H, Üngör M. In vitro comparison of different types of sodium perborate used for intracoronal bleaching of discolored teeth. Int Endod J 2002; 35:433-436.
- Rotstein I, Mor C, Friedman S. Prognosis of intracoronal bleaching with sodium perborate preparations in vitro: 1-year study. J Endod 1993; 19:10-12.
- Kim ST, Abbott PV, McGinley P. The effects of Ledermix paste on discolouration of mature teeth. Int Endod J 2000; 33:227–232.
- Lim MY, Lum SOY, Poh RSC, et al. An in vitro comparison of the bleaching efficacy of 35% carbamide peroxide with established intracoronal bleaching agents. Int Endod J 2004; 37:483–488.
- Muthukrishnan L. Imminent antimicrobial bioink deploying cellulose, alginate, EPS and synthetic polymers for 3D bioprinting of tissue constructs. Carbohydr Polym 2021; 260:117774.
- Pradeep Kumar AR, Shemesh H, Nivedhitha MS, et al. Diagnosis of vertical root fractures by cone-beam computed tomography in root-filled teeth with confirmation by direct visualization: A systematic review and meta-analysis. J Endod 2021; 47:1198–1214.
- Chakraborty T, Jamal RF, Battineni G, et al. A review of prolonged post-COVID-19 symptoms and their implications on dental management. Int J Environ Res Public Health 2021; 18.
- Muthukrishnan L. Nanotechnology for cleaner leather production: A review. Environ Chem Lett 2021; 19:2527–2549.
- Teja KV, Ramesh S. Is a filled lateral canal: A sign of superiority? J Dent Sci 2020; 15:562.
- Narendran K, Jayalakshmi, Sarvanan A, et al. Synthesis, characterization, free radical scavenging and cytotoxic activities of phenylvilangin, a substituted dimer of embelin. Indian J Pharm Sci 2020; 82.
- Reddy P, Krithikadatta J, Srinivasan V, et al. Dental caries profile and associated risk factors among adolescent school children in an urban south-Indian city. Oral Health Prev Dent 2020; 18:379–386.
- Sawant K, Pawar AM, Banga KS, et al. Dentinal microcracks after root canal instrumentation using instruments manufactured with different NiTi alloys and the SAF system: A systematic review. Adv Sci Inst Ser E Appl Sci 2021; 11:4984.
- Bhavikatti SK, Karobari MI, Zainuddin SLA, et al. Investigating the antioxidant and cytocompatibility of Mimusops elengi Linn extract over human gingival fibroblast cells. Int J Environ Res Public Health 2021; 18.
- Karobari MI, Basheer SN, Sayed FR, et al. An in vitro stereomicroscopic evaluation of bioactivity between Neo MTA Plus, pro root MTA, biodentine & glass ionomer cement using dye penetration method. Materials 2021; 14.
- Rohit Singh T, Ezhilarasan D. Ethanolic extract of Lagerstroemia speciosa (L.) pers., induces apoptosis and cell cycle arrest in HepG2 cells. Nutr Cancer 2020; 72:146–156.
- Ezhilarasan D. MicroRNA interplay between hepatic stellate cell quiescence and activation. Eur J Pharmacol 2020; 885:173507.
- Romera A, Peredpaya S, Shparyk Y, et al. Bevacizumab biosimilar BEVZ92 versus reference bevacizumab in combination with FOLFOX or FOLFIRI as first-line treatment for metastatic colorectal cancer: A multicentre, open-label, randomized controlled trial. Lancet Gastroenterol Hepatol 2018; 3:845–855.
- Raj RK. β-Sitosterol-assisted silver nanoparticles activates Nrf2 and triggers mitochondrial apoptosis via oxidative stress in human hepatocellular cancer cell line. J Biomed Mater Res 2020; 108:1899–1908.
- Vijayashree Priyadharsini J. In silico validation of the non-antibiotic drugs acetaminophen and ibuprofen as antibacterial agents against red complex pathogens. J Periodontol 2019; 90:1441–1448.
- Priyadharsini JV, Vijayashree Priyadharsini J, Smiline Girija AS, et al. In silico analysis of virulence genes in an emerging dental pathogen A. baumannii and related species. Arch Oral Biol 2018; 94:93–98.
- Uma Maheswari TN, Nivedhitha MS, Ramani P. Expression profile of salivary micro RNA-21 and 31 in oral potentially malignant disorders. Braz Oral Res 2020; 34:e002.
- Gudipaneni RK, Alam MK, Patil SR, et al. Measurement of the maximum occlusal bite force and its relation to the caries spectrum of first permanent molars in early permanent dentition. J Clin Pediatr Dent 2020; 44:423–428.
- Chaturvedula BB, Muthukrishnan A, Bhuvaraghan A, et al. Dens invaginatus: A review and orthodontic implications. Br Dent J 2021; 230:345–350.
- Kanniah P, Radhamani J, Chelliah P, et al. Green synthesis of multifaceted silver nanoparticles using the flower extract of Aerva lanata and evaluation of its biological and environmental applications. Chem Select 2020; 5:2322–2331.
- Weiger R, Kuhn A, Löst C. Radicular penetration of hydrogen peroxide during intra‐coronal bleaching with various forms of sodium perborate. Int Endod J 1994; 27:313-317.
- Pearson NL. Nothing to smile about: Drug-induced tooth discolouration. Canadian Pharm J 2007; 140:263.
- Feiz A, Khoroushi M, Gheisarifar M. Bond strength of composite resin to bleached dentin: Effect of using antioxidant versus buffering agent. J Dent 2011; 8:60–66.
- Rotstein I, Zalkind M, Mor C, et al. In vitro efficacy of sodium perborate preparations used for intracoronal bleaching of discolored non-vital teeth. Endod Dent Traumatol 1991; 7:177–180.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Nivethitha R and Subash Sharma*
Department of Conservative Dentistry, Saveetha Dental College & Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, IndiaReceived: 08-Jun-2022, Manuscript No. JRMDS-22-69495; , Pre QC No. JRMDS-22-69495 (PQ); Editor assigned: 10-Jun-2022, Pre QC No. JRMDS-22-69495 (PQ); Reviewed: 24-Jun-2022, QC No. JRMDS-22-69495; Revised: 29-Jun-2022, Manuscript No. JRMDS-22-69495 (R); Published: 06-Jul-2022
