Review Article - (2022) Volume 10, Issue 9
Mucocele of Oral Cavity: Literature Review and Case Report
Anvika Deshpande1, Vidya Lohe1*, Ravindra Kadu2, Ravikant Sune1, Swapnil Mohod1 and Dhiran Talatule2
*Correspondence: Vidya Lohe, Department of Oral Medicine and Radiology, Sharad Pawar Dental College, Datta Meghe Institute of Medical Sciences (Deemed to be University) Sawangi (Meghe) Wardha, India, Email:
Abstract
Minor salivary gland origined mucocele, occurs when there is a disturbance in ϔ of its secretions which occurs due to accumulation of mucous secretions caused due to trauma. It most frequently occurs around the lower labial mucosa as it is more liable to trauma. Following is an article, reviewing the case of a 14 year old female patient with lip biting habit, which led to development of mucocele near the lower lip.
Keywords
Origined mucocele, Mucocele, Trauma, MucosaIntroduction
Developmental, inflammatory, ulcerative, neoplastic conditions etc. are various groups of lesions found in lips. One of the most common lesions of oral mucosa is mucocele which occurs due to build-up of mucous secretions due to trauma or lip biting habits [1]. Lower labial mucosa is the most common site of occurrence of oral mucocele as it is more likely to experience trauma [2]. Mucocele is pain free and has a high possibility of recurrence [3]. They are sub-categorised into two types: Mucous extravasation type and Mucous retention type. The mucous extravasation type occurs due to trauma for e.g. Lip biting where retention of mucous occurs due to congestion of minor salivary glands [4,5]. Leakage into the soft tissues is caused by traumatized salivary ducts surrounding the gland leading to extravasation mucocele. Surrounding the mucosa there is formation of pseudocapsule in the final stage [6]. Clinically, both extravasation and retention cyst appear similar. It is mostly clinically diagnosed due to its pathognomonic appearance [7]. Retention mucocele can be found in any part of the oral cavity; whereas extravasation mucocele are most commonly seen on the lower lip, tongue and buccal mucosa. The probabilities of mucocele to be found in the posterior region of the tongue are low [8]. Mucocele usually do not show any symptoms but can sometimes cause difficulty in chewing, swallowing or speech.
Lower labial mucosa is the most common location for occurrence of mucocele as it contains adipose, connective tissue, salivary glands, blood capillaries and nerves; any pathology which involves the above can cause mucocele on the lips [9]. Mucocele on the oral mucosa could be present deep within the connective tissue or as a fluid filled vesicle. There could be drainage of mucin from the superficial lesions which precedes the recurrence. Fibrosis could be seen in long standing lesions [10]. Diagnosis of mucocele could be confirmed based on the lesion`s colour, site, etiology and consistency. Final diagnosis could be confirmed by histological investigations. Treatment modality for mucocele includes surgical excision, cryosurgery, laser excision, laser vaporization, mar supilization and micro mar supilization [8].
Case Presentation
A fourteen years old female child came to the outpatient department of oral medicine and radiology with chief complaint of pain free swelling in lower right lip region since 2 months. The HOPI suggested that the swollen area was found labially in the in 42, 43 regions Figure 1A and 1B. For past 2 months; it was initially small in size and progressively increased to present size. She also gave history of increase or decrease in size while mastication. The patient gave history of lip biting since 2 months. The patient had no history of difficulty in mastication and speech.
Figure 1A: Intraoral appearance of the swelling.
Figure 1B: Extra-oral appearance of the swelling.
The palpatory clinical examination implied that the lesion was soft, fluctuant and tenderness was absent. The lesion was approximately 2 × 2 cm in size. It was expanding inferiorly toward the lingual vestibule. The swelling was pale pink in colour. On intra-oral examination, the other findings of occlusal caries with 36 and 46 were present. Generalized stains and calculus in lower anterior region was present.
On the basis of the clinical features and habit history of lip biting the case was diagnosed as Mucocele. Treatment planning was done and explained to the patient’s guardian. After obtaining the parents’ consent treatment was performed this included surgical excision under local anesthesia. Scaling and polishing was done. Restoration with 36 and 46 was done on the patient’s first clinical visit. Excisional biopsy was carried out and the specimen was sent for histopathological examination Figure 2.
Figure 2: Excisional biopsy specimen.
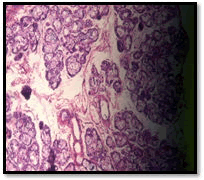
Histopathological reports were obtained before giving final diagnosis. Histopathology reports, showed mucin spillage from the salivary acini Figure 3. The lesion was confirmed as mucocele. It was surgically excised. It was done by elliptical excision. It was done under aseptic conditions and general anesthesia. The patient was instructed to visit for regular re-evaluation at 3 months interval for more than 35 months. The patient on each follow up visit was thoroughly examined. Various measures were taken into consideration to prevent recurrence. Such measures were taken as the chances of recurrence of this lesion are quite high. After monitoring the patient for 35 months no signs of recurrence of this lesion were found.
Figure 3: Histopathology shows underlying connective tissue shows spillage of mucin from the salivary acini.
Surgically, various measures are taken to prevent recurrence such as complete excision of the lesion. The sutures were placed using non absorbable silk sutures. During first few follow up visits; after a week, the sutures were successfully removed and the wound healed by formation of granulation tissue by primary intension. The patient was given post-operative instruction. The patient was asked not to touch the wounded area. Pain medications were prescribed. The patient was asked to consume pain medications if she experienced pain.
Discussion
The percentage of prevalence of mucocele in general population is 0.4 to 0.9% [11]. Mucocele has no gender predilection. Traditionally, elliptical incision procedure is used to treat mucocele. Entire adjacent glandular acini should be excised till the muscle layer. Recurrence could be avoided by preventing injury to the adjacent glands during suturing [12].
In the present case the patient had habit of lip biting and the mucocele was present on lower lip. The most frequent location of mucocele is lower lip and mostly the cause is trauma or habit of lip biting [14]. Due to injury from lip biting retention of mucous occurs due to congestion of minor salivary glands [4,5].
On the basis of the clinical features and habit history of lip biting the case was diagnosed as Mucocele. Diagnosis of mucocele could be confirmed based on the lesion`s colour, site, etiology and consistency. In this case as the size of the lesion was small excisional biopsy was performed and the tissue sample was sent for microscopic examination to confirm the clinical diagnosis. Final diagnosis could be confirmed by histological investigations. It showed mucin spillage from salivary acini. Treatment modalities for mucocele include surgical excision, cryosurgery, laser excision, laser vaporization, marsupilization and micromarsupilization [8].
After the successful management of mucocele in this 14 years female a long term follow-up was carried out to keep a check for recurrence. Mucocele on the oral mucosa could be present deep within the connective tissue or as a fluid filled vesicle. There could be drainage of mucin from the superficial lesions which precedes the recurrence. Fibrosis could be seen in long standing lesions [10,14]. This case was diagnosed as extravasation mucocele as it had a history of trauma and it is apparent from various studies that extravasation mucocele is more frequently found on lower lip. Similar successful studies were carried out in my institute and successful results were yielded by it.
Conclusion
The lips are a common site for trauma, resulting in injury to the minor salivary glands of the lips, which can lead to mucocele formation. The diagnosis is typically guided by the history of trauma and clinical appearance. It is difficult to remove mucocele surgically as there are high chances of injury to the adjacent salivary glands as well as chances of recurrence. Fibrosis could be seen in long standing lesions.
References
- Nallasivam KU, Sudha BR. Oral mucocele: Review of literature and a case report. J Pharm Bioallied Sci 2015; 7:S731-S733.
- Gonsalves WC, Chi AC, Neville BW. Common oral lesions: Part II. Masses and neoplasia. Am Fam Physician 2007; 75:509–512.
- Bermejo A, Aguirre JM, Lopez P, et al. Superficial mucocele: report of 4 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 88:469-472.
- Baurmash HD. Mucoceles and ranulas. J Oral Maxillofac Surg 2003; 61:369–378.
- Muhammad H, Soni A. Mucocele and ranula. StatPearls publishing
- Ata-Ali J, Carrillo C, Bonet C, et al. Oral mucocele: Review of literature. J Clin Exp Dent 2010; 2:18-21.
- Chaitanya P, Praveen D, Reddy M. Mucocele on lower lip: A case series. Indian Dermatol Online J 2017; 8:205-207.
- Sukhtankar LV, Mahajan B, Agarwal P. Treatment of lower lip Mucocele with Diode Laser – A Novel Approach. Ann Dent Res 2013; 2:102-108.
- Lohe VK, Degwekar SS, Bhowate RR, et al. Rapidly maturing juvenile ossifying fibroma: a case report. Dentomaxillofacial Radiology 2011; 40:195-198.
- Oral mucocele: Review of literature and a case report
- Laller S, Saini RS, Malik M, et al. An Appraisal of Oral Mucous Extravasation cyst case with Mini Review. J Adv Med Dent Sci Res 2014; 2:166-170.
- Rao PK, Hegde D, Shetty SR, et al. Oral Mucocele – Diagnosis and Management. J Dent Med Sci 2012; 2:26-30.
- Pooja Dhole, Lohe VK, Ravindra P Kadu, et al. A case series on Mucocele. Med Sci, 2020; 24:2877-2882.
- Gupta SV, Lohe VK, Bhowate RR. Lip abscess due to insect bite: A case report. J Oral Med Surg 2017; 1:27-29.
Author Info
Anvika Deshpande1, Vidya Lohe1*, Ravindra Kadu2, Ravikant Sune1, Swapnil Mohod1 and Dhiran Talatule2
1Department of Oral Medicine and Radiology, Sharad Pawar Dental College, Datta Meghe Institute of Medical Sciences (Deemed to be University) Sawangi (Meghe) Wardha, India2Department of General Pathology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences (Deemed to be University) Sawangi (Meghe) Wardha, India
Citation: Anvika Deshpande, Vidya Lohe, Ravindra Kadu, Ravikant Sune, Swapnil Mohod, Dhiran Talatule, Mucocele of Oral Cavity: Literature Review and Case Report, J Res Med Dent Sci, 2022, 10 (9): 000-000.
Received: 30-Jun-2022, Manuscript No. JRMDS-22-47356; , Pre QC No. JRMDS-22-47356; Editor assigned: 01-Jul-2022, Pre QC No. JRMDS-22-47356; Reviewed: 15-Jul-2022, QC No. JRMDS-22-47356; Revised: 30-Aug-2022, Manuscript No. JRMDS-22-47356; Published: 05-Sep-2022