Research - (2021) Volume 9, Issue 4
Multimodality Imaging Evaluation of Spinal Trauma
*Correspondence: Prabakaran M, Department of Radio Diagnosis, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email:
Abstract
The aim of the present study is to evaluate, identify and compare the imaging findings in traumatic spinal injuries using Plain radiographs, MDCT and MRI. A comparative study involving 60 patients with spinal trauma brought to the Radiology department in Sree Balaji Medical College and Hospital for plain radiographic, CT and MR imaging over a period between March 2018 and September 2019. MRI is significantly superior to CT in detecting injuries to the soft tissue and the spinal cord.
Keywords
Trauma, Radiology, Prosthetic heart valves, Soft tissue hematoma
Introduction
Spinal injuries can be devastating, especially if not promptly evaluated. Most spine injuries occur due to motor vehicle accidents, falls and also commonly in sports, falls, and sports injuries. Injuries in this region often result in neurological deficits and may even be fatal [1-3]. Imaging is essential for evaluating spinal trauma patients. Plain radiographs, were historically used in evaluating spinal injuries [4]. While it is still performed routinely in patients with less severe history of injury with no neurological deficits, they do not compare to Computed Tomography (CT) in detecting fractures. CT extremely sensitive for evaluating bony injuries. Magnetic Resonance Imaging (MRI) has gained importance for evaluating traumatic spine injuries, specifically, to assess stability of the spine, to localize the injury precisely and to detect neural element compromise. CT, although excellent in assessing osseous pathologies, cannot be used for complete clearance in cases of spinal cord and ligamentous injuries. In this scenario MRI becomes essential for evaluating spine in the setting of trauma, more so in patients with neurological symptoms with a negative CT [5-9].
Materials and Methods
A comparative study involving 60 patients with spinal trauma brought to the Radiology department in Sree Balaji Medical College and Hospital for plain radiographic, CT and MR imaging over a period between March 2018 and September 2019.
Patient Selection
Inclusion criteria
✓ Patients with recent spinal trauma.
Exclusion criteria
✓ Patients who had contraindications for MR imaging (e.g. cardiac pacemakers Prosthetic heart valves, ferromagnetic vascular clips, cochlear implants, intra ocular metallic foreign bodies)
✓ Claustrophobic patients.
✓ Pregnant women in CT and plain radiographs.
✓ Technically unsatisfactory images.
Equipment
✓ GE- 800 mA CR XRAY
✓ Siemens 16 Slice GO Series CT imaging consisted of contiguous 1 mm slices with sagittal AND coronal reformation.
✓ GE HD 1.5Tesla MRI sequences included Axial T2, Sagittal T1, Sagittal T2, T2 Selective partial Inversion Recovery (SPIR)/FAT, Coronal Proton Density (PD). Cervical spine coils were employed for imaging the cervical spine.
✓ To determine the clinical relevance of imaging in the diagnosis of trauma to the spine, the following variables were considered: Etiology, age, gender and level of injury. The following radiological findings were observed in all the patients by the different modalities in order to assess their sensitivity in comparison to the gold standard for each finding:
✓ Vertebral body fractures.
✓ Posterior element fractures (articular facets, lamina, pedicle, transverse and spinous processes, lateral mass, arch and joint capsules).
✓ Listhesis.
✓ Injury to the posterior ligamentous complex comprising the supraspinous and interspinous ligaments, ligamentum flavum.
✓ Spinal cord compression.
✓ Spinal cord contusion
✓ Disc herniation.
✓ Extradural hematoma
Results
Descriptive analysis was carried out by mean and standard deviation for quantitative variables, frequency and proportion for categorical variables. Non- normally distributed quantitative variables were summarized by median and interquartile range (IQR). Data was also represented using appropriate diagrams like bar diagram, pie diagram and box plots. All Quantitative variables had been checked for normal distribution. Each category of explanatory variable and using normality Q-Q plots and visual inspection of histograms. Shapiro-Wilk test was conducted to evaluate normal distribution. Shapiro-Wilk test p value of >0.05 was considered as normal distribution. For normally distributed Quantitative parameters the mean values were compared between study groups using Independent sample t-test (2 groups). Categorical outcomes were compared between study groups using Chi square test / Fisher's Exact test (If the overall sample size was < 20 or if the expected number in any one of the cells is <5, Fisher's exact test was used.) P value of less 0.05 was considered statistically significant. IBM SPSS version 22 was used for statistical analysis. The total no. of patients included in the study was 60. Of those 38 were male and 22 were female. The mean age of the patients included in the study were 38.2 in males and 39.6 in females (Table 1). The most common age groups in patients with spinal trauma were 31-40 years followed by 20-29 age group (Figure 1). The most common cause of spinal trauma was motor vehicle accidents (58.3 %), followed by fall (38.3%). Assault was the cause in the other cases (Table 2). The most common site of injury on presentation was the cervical region (48.3%) followed by lumbar region (23.3 %) (Figure 2).
Table 1: Demographics of the patients.
| Sex | Frequency | Percentage |
|---|---|---|
| Female | 22 | 36.7 |
| Male | 38 | 63.3 |
| Total | 60 | 100 |
Table 2: Etiology of injury.
| Etiology of injury | Frequency | Percent |
|---|---|---|
| Assault | 2 | 3.3 |
| Fall | 23 | 38.3 |
| MVC | 35 | 58.3 |
| Total | 60 | 100 |
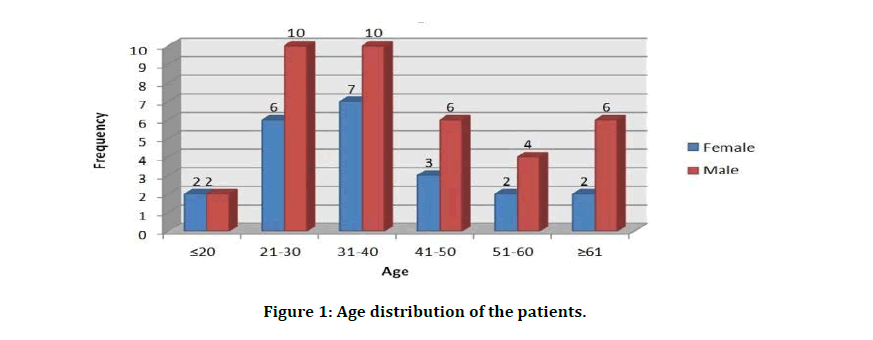
Figure 1: Age distribution of the patients.
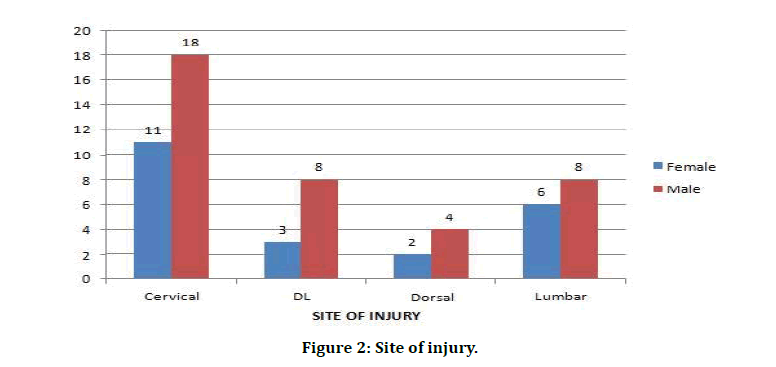
Figure 2: Site of injury.
Detection of fractures
CT being considered the gold standard, fractures was seen in 34 patients (56.7%), listhesis was seen in 16 patients (26.7%). Of the 34 patients who had fractures, 6 patients (17.6%) had fractures at multiple levels detected by CT. 3 patients among those who had fractures (8.8%) had noncontiguous spinal fractures On CT imaging 34 patients had fractures (Vertebral body fracture in 18 patients, often overlapping with posterior element fracture in 28 patients). On plain radiographs, fractures were noted in 14 patients. While in MRI fractures were seen in 30 patients. Vertebral body fractures were seen in 18 patients on CT, 18 patients on MRI and only in 10 patients on plain radiograph Posterior element fractures were seen in 28 patients on CT, 20 patients on MRI and only in 11 patients on plain radiograph. Listhesis was seen in seen in 16 patients on CT, 16 patients on MRI and in 13 patients on plain radiograph (Table 3 and Figure 3).
Table 3: Bony injuries.
| Injury | Plain | CT | MRI |
|---|---|---|---|
| radiograph | |||
| Any fracture | 14 | 34 | 30 |
| Vertebral body | 10 | 18 | 18 |
| fracture | |||
| Posterior element | 11 | 28 | 20 |
| fracture | |||
| Listhesis | 13 | 16 | 16 |
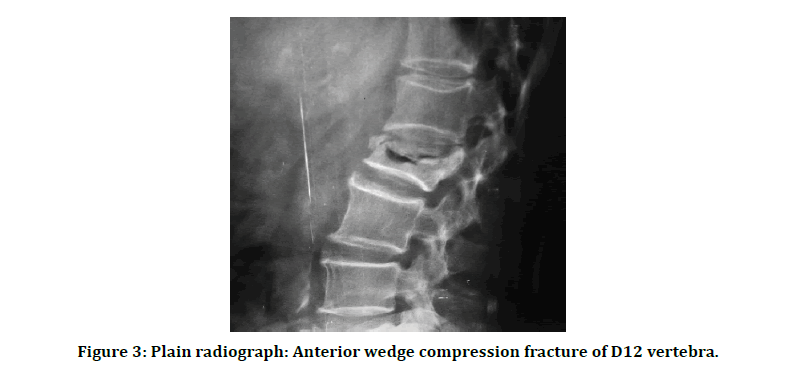
Figure 3: Plain radiograph: Anterior wedge compression fracture of D12 vertebra.
Detection of non-osseous injuries was done on MRI and CT. On MRI, 18 patients (30%) presenting with injury to the spine had ligamentous injury. Disc herniation was seen in 14 patients (23.3%), extradural hematoma in 13 patients (21.7%), spinal cord involvement was seen in 18 patients (30% )with spinal cord contusion in 6 patients (10%) and soft tissue hematoma in 9 patients (15%) whereas on CT ligamentous injury was seen in 4 patients (6.7%), disc herniation was seen in 8 patients (13.3%), extradural hematoma in 6 patients (10%), spinal cord involvement was seen in 8 patients (13.3%) with spinal cord contusion in none of the patients and soft tissue hematoma in 5 patients (8.3%) (Table 4 and Figure 4). Sensitivity= 55.1% Specificity=100.0% Positive predictive value=100.0% Negative predictive value= 92.7% (Table 5 and Figure 5).
Table 4: Non osseous injuries.
| Injury | CT | MRI |
|---|---|---|
| Ligamentous injury | 4 | 18 |
| Disc herniation | 8 | 14 |
| Extradural hematoma | 6 | 13 |
| Spinal cord compression | 8 | 18 |
| Spinal cord contusion | 0 | 6 |
| Soft tissue hematoma | 5 | 9 |
Table 5: Soft tissue hematoma – MRI vs CT.
| MRI | |||
|---|---|---|---|
| CT | Yes | No | Total |
| Yes | 5 | 0 | 5 |
| No | 4 | 51 | 55 |
| Total | 9 | 51 | 60 |
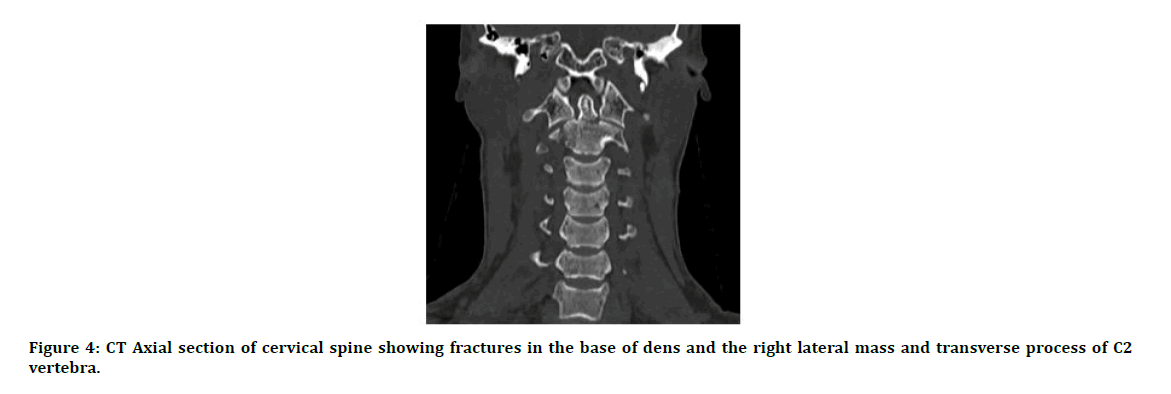
Figure 4: CT Axial section of cervical spine showing fractures in the base of dens and the right lateral mass and transverse process of C2 vertebra.
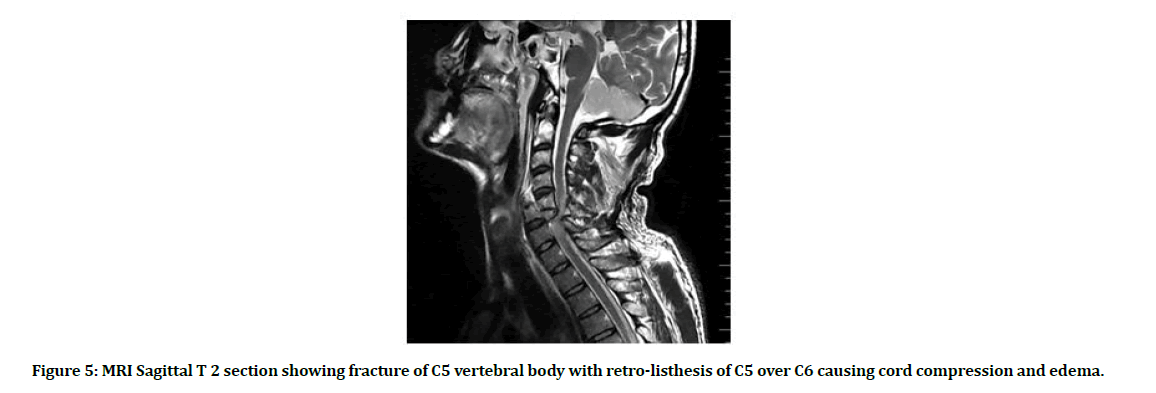
Figure 5: MRI Sagittal T 2 section showing fracture of C5 vertebral body with retro-listhesis of C5 over C6 causing cord compression and edema.
Discussion
In our study motor vehicle accidents (58.3%) were the most common cause for spine trauma followed by falls (38.3%). This correlates with a meta-analysis done by at Kumar et al71 where road traffic accidents and falls were the leading causes of traumatic spinal injury. (39.5%, SD ± 16.6 and 38.8%, SD ± 17.7) Gender: Regarding gender, in our study males (63.3%) were more commonly involved than females (37.7%). In a study done by Sidon et al spinal trauma was found to be more commonly occurring in males (69.4%) compared to females (30.6%) [10]. The mean age of the patients in our study was 38.7 (38.2 in males and 39.6 in females). The most commonly affected age groups were 31- 40 years (28.3%) and 21-30 years (26.6%). This distribution was similar to one found in a study done by Shrestha et al where 30.4% belonged to the 21-30 years age group and 23.1% belonged to the 31-40 years age group. In our study the most commonly affected fracture level was L1 (20%) followed by C2, C5 and D12 vertebra (12.5%, 10% and 10% respectively). In an observational study by Hongwei et al the most common fracture levels encountered were L1 (19.2%) and D12 (11.3%) followed by C2 (8.3%) [11]. In our study, 3 patients (8.8%) of the patients with fractures had noncontiguous spinal injuries. In a study done by Kanna et al. noncontiguous spinal injuries were seen in 19.6 % of spinal injury patients. In our study 6 out of the 34 patients (17.6%) had involvement of more than one vertebra. In a study done by Leucht et al, 21.3% of patients had fracture in a second vertebra. For detection of fractures, CT has been the gold standard. A study by Woodring et al showed that 61% of fractures and 36 % of subluxations were unnoticed on plain radiographs. In our study, CT detected fractures in 56.6% and listhesis in 26.7% in of the patients, whereas plainradiograph [12]. detected fractures only in 25 % and listhesis in 21.7% of the patients in our study. Plain radiograph failed to detect 55.8 % of the fractures identified on CT and 18 % of listhesis identified on CT. MRI had 100% sensitivity in detecting vertebral body fractures. However when it came to detection of posterior element fractures, MRI had a sensitivity of 71.4 % on comparison with CT. The sensitivity of MRI is lower than CT for detecting fractures of the posterior elements due to edema associated with avulsion injuries and to fractures in the craniocervical region [13]. The utility of MRI when it comes to spinal trauma is its ability to identify soft tissue injuries and injuries to the ligaments and spinal cord. In our study ligamentous injuries were seen in 30% of the patients imaged. CT was able to detect this finding in only 4 patients (Sensitivity–22.2%) out of the 18 patients who had ligamentous injury detected on MRI. In our study, herniation of disc was seen in 14 patients on MRI while CT was able to help diagnose disc herniation in 8 patients (57.1 % sensitivity) In a study done by Preethi et al, CT detected 83% of disc herniations seen on MRI. In our study, of the 24 patients with a negative CT, 3 patients had abnormal findings on MRI (12.5%) [14]. In a study by James et al MRI detected abnormalities 16.6% of patients with a negative CT. Another study by Maung et al. found that cervical spine MRI was abnormal in 23.6% of all patients who had a negative CT. However the MRI findings did not alter the management of these patients as was the case in our study.
Conclusion
In the setting of trauma to the spine, plain radiographs cannot reliably rule out vertebral fracture and further imaging is warranted especially in case of severe trauma. MDCT while excellent in detecting fractures cannot rule out soft tissue injuries and a negative CT should not prevent further imaging with MRI if clinically indicated. MRI is significantly superior to CT in detecting injuries to the soft tissue and the spinal cord. MRI should be performed if there is any suspicion of spinal cord injury.
Acknowledgement
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Van Goethem JW, Maes M, Özsarlak Ö, et al . Imaging in spinal trauma. Eur Radiol 2005; 15:582-90.
- Kang Y, Ding H, Zhou H, et al. Epidemiology of worldwide spinal cord injury: A literature review. J Neurorestoratol 2017; 6:1-9.
- Hoffman JR, Schriger DL, Mower W, et al. Low-risk criteria for cervical-spine radiography in blunt trauma: a prospective study. Annals Emergency Med 1992; 21:1454-60.
- Deliganis AV, Baxter AB, Hanson JA, et al. Radiologic spectrum of craniocervical distraction injuries. Radiographics 2000; 20:S237-50.
- Junewick JJ. Pediatric craniocervical junction injuries. AJR Am J Roentgenol 1996; 201:1003–10.
- Hadley MN, Browner C, Sonntag VK. Axis fractures: A comprehensive review of management and treatment in 107 cases. Neurosurg 1985; 17:281-90.
- Yang SY, Boniello AJ, Poorman CE, et al. A review of the diagnosis and treatment of atlantoaxial dislocations. Global Spine J 2014; 4:197-210.
- Crook TB, Eynon C. Traumatic atlantoaxial rotatory subluxation. Emergency Med J 2005; 22:671.
- Penning L. Prevertebral hematoma in cervical spine injury: incidence and etiologic significance. Am J Roentgenol 1981; 136:553-561.
- Shen H, Tang Y, Huang L, et al. Applications of diffusion-weighted MRI in thoracic spinal cord injury without radiographic abnormality. Int Orthop 2007; 31:375-83.
- Frankel HL, Rozycki GS, Ochsner MG, et al. Indications for obtaining surveillance thoracic and lumbar spine radiographs. J Trauma 1994; 37:673-676.
- Crim JR, Moore K, Brodke D. Clearance of the cervical spine in multitrauma patients: the role of advanced imaging. InSeminars in Ultrasound, CT and MRI 2001; 283-305.
- Woodring JH, Lee C. Limitations of cervical radiography in the evaluation of acute cervical trauma. J Trauma 1993; 34:32-9.
- Ito Z, Harada A, Matsui Y, et al. Can you diagnose for vertebral fracture correctly by plain X-ray?. Osteoporosis Int 2006; 17:1584-91.
Author Info
Department of Radio Diagnosis, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Adarsh M, Prabakaran M, Multimodality Imaging Evaluation Of Spinal Trauma, J Res Med Dent Sci, 2021, 9 (3):237-242.
Received: 20-Mar-2021 Accepted: 06-Apr-2021
