Research - (2020) Volume 8, Issue 3
Musculoskeletal Disorders Among Dental Students
Noor Sam Ahmad1*, Asma Alhusna Abang Abdullah1, Ooi Kee Thyng2 and Teong Ling Xin2
*Correspondence: Noor Sam Ahmad, Department of Family Dental Health, Orthodontic Unit, Faculty of Dentistry, Universiti Kebangsaan Malaysia, Malaysia, Email:
Abstract
Introduction: Dentistry is a profession that requires prolonged repetitive movement, sustained various body posture and stress that can contribute significantly to the development of musculoskeletal discrepancy (MSD), psychological stress and fatigue. MSD can occur in any part of the body, ranging from postural muscle, upper extremities and the lower extremities. If left untreated, MSD can cause severe degenerative and inflammatory disorders. The aim of this study is to determine the prevalence of musculoskeletal disorders (MSD) among dental students.
Methods: This was a descriptive cross-sectional survey involving a convenient sample of 244 undergraduate and postgraduate dental students in UKM. A previously validated self-reporting questionnaire measuring MSD prevalence, derived from the Standardized Nordic Questionnaire, was distributed to students. The questionnaire included demographic data and areas where the dental students experienced trouble (ache, pain, discomfort and numbness). Data were analyzed using SPSS 22.0. Ethics approval was obtained from UKM Research Ethics Committee. Results: The neck was the most commonly affected area among UKM dental students, followed by lower back and shoulders. Neck and lower back were the regions which showed increased pattern of pain prevalence in relation to years of working experience. Shoulder pain was reported highest in 3 years of working experience.
Conclusion: This study showed the increasing evidence that MSD could be developing in students, before the starting of a professional career. It also highlighted the need to place further emphasis on ergonomic education.
Keywords
Dental, Musculoskeletal disorders, Students
Introduction
Musculoskeletal disorders (MSD) are defined as muscular pain or injuries to the human support system that can occur after a single event or cumulative trauma, hence causing negative impact on daily activities [1]. MSD can vary from discomfort, numbness, ache, pain and it can even prevent normal daily activities. MSD can occur in any part of the body, ranging from postural muscle, upper and lower extremities.
One of the risk factor categories for MSD is work related (ergonomic) risk factors. The primary ergonomic risk factors can further be broken into three parts which are high task repetition, forceful exertions and sustained awkward postures. There are many works or tasks that are repetitive in nature which usually controlled by hourly or daily production targets. If this high task repetition combines with other risk factor, MSD can develop. There are works or tasks that put high force loads on human body. This forceful exertion requires high muscle efforts will cause fatigue which later may lead to MSD. Workers that work in an awkward posture and sustained in that posture will place an excessive force on the joints and muscles and tendons around the joints. MSD will develop if there is no adequate recovery period [2]. Individual risk factor is another category of risk factor for MSD. This risk factor comprise of poor work practices, poor overall health practices, poor rest and recovery, poor nutrition, fitness and hydration. This category is related to individual worker who has poor work practices, wrong lifting techniques, smoking, taking alcohol, obese, do not get enough rest and recovery, malnourished, frequently dehydrated and has poor level of physical fitness [2]. Individuals that have one or more of the above risk factors, they are at greater risk of developing a musculoskeletal imbalance and eventually an MSD.
Dentistry requires the dentist to keep their head, neck, shoulder and other body parts in a fixed position as a routine of daily work. In this situation, the dentists are more susceptible to have MSD, psychological stress, fatigue [3], cumulative trauma disorder and occupational health hazard [4]. The prevalence of working musculoskeletal disorders (WMSD) was found as high as 64% to 93% from a systemic review [5]. Prolonged awkward postures (rotation or forward bending of the head, neck and body to one side) will lead to the strengthening and contraction of muscle on the preferred side of bending or rotation and weakening and elongation of the antagonistic muscle. This will cause muscle imbalance [6]. The weakened and elongated muscles are under stress and susceptible to ischemia or necrosis [7].
Under normal circumstances, damaged tissues are repaired during periods of rest. However, in dentistry due to the insufficient recovery time for muscle, necrosis of muscles is prone to occur as the rate of damage exceeds the rate of repair. Currently, muscle substitution occur as the body compensates by using other parts of muscles to maintain posture and protect damaged muscle from further stress [8] and this eventually leads to development of MSDs.
Increased in MSD occurrence had caused the reduction in the amount of the productivity, early retirement and increased number of sick leave among dental practitioners. This had subsequently led to the increase of global awareness towards the MSD issue [8,9]. It has been proven that the ergonomic practices and application of ergonomic in dental instruments and facilities design can help to reduced or prevent MSD related injury [10]. Stretching exercise, operator chairs with lumbar support, dental loupes, working with elbows lower than shoulders have been encouraged to improve posture during clinical works thus reducing stress and the risk of developing MSD [11].
Few studies showed that the prevalence of MSD was in negative correlation with years of experience [11,12]. It is believed that dentists gained experience through their clinical practices and learn to adjust their work posture to avoid pain or discomfort [8]. Thus, this proposes that dental student can start showing the sign of MSD even during their early years of training. This statement was supported by research that concluded more than 70% of dental students experienced neck, shoulder and lower back pain as early as the third year of their dental training [12].
Thus, the aim of this study was to determine the prevalence of musculoskeletal disorders among dental students by measuring MSD prevalence using a selfadministered questionnaire. The objectives of this study were to determine the mostly affected area of pain among dental students and to compare the prevalence of MSD based on year of experience.
Materials and Methods
Ethics approval and study sample
The ethics approval was obtained from Universiti Kebangsaan Malaysia (UKM) Institutional Review Board for Research and Ethics (UKM PPI/111/8/ JEP-2018-440). Participants included in the study were all undergraduate students in their second year (UG2), third year (UG3), fourth year (UG4) and fifth year (UG5) of Doctor of Dental Surgery (DDS) programme and all postgraduate students (PG). Exclusion criteria was applied to the students who absent on the day of conducting research. The participants were recruited via convenience sampling as this is the most time-efficient and effective method to obtain an appropriate sample relevant to the research question.
Study design
This study was carried out as descriptive and exploratory research, using a cross-sectional approach. The study examined the prevalence of MSD in undergraduate and postgraduate dental students. A cross-sectional design was selected as this was identified as the most appropriate method to answer the research question.
The survey
The questionnaire was in Google forms. It was eight pages long and included a plain-language (English) statement explaining the study. The questionnaire was an adapted version of an original tool by Smith and Leggat [8] that has been previously validated and used among medical, dental, nursing and occupational therapy students, dental hygienists and dentists [4,13]. The questionnaires include age, gender, year of experience, working hours per week, dominant hand, locations where subject had trouble (ache, pain, discomfort, numbness) during the last 12 months and severity of lower back, neck and shoulder pain. The recruitment strategy involved the student researchers approaching students during timetabled lecture or tutorial sessions and inviting them to complete the questionnaire. Link and bar code were distributed to the subjects and they were required to enter the link or scan the bar code to access the questionnaire. We obtained a voluntary, signed informed consent from the participants before the start of the study. The students were given 10 minutes to complete the questionnaire during the session.
Data analysis
Data collected from the questionnaires were analysed using Statistical Package for the Social Science (SPSS) software version 22.0 (IBM Corporation, Armonk, NY, USA). First, descriptive analysis was performed for demographic data to have a general view of the sample’s gender, age, year of experience and working hours per week, as well as dominant hand. A chi-square test was chosen to analyse the data comparatively as the variables were nominal and consist of two or more categorical, independent groups.
Results
total of 244 questionnaires were distributed and completed. A high response rate (91.8%) was able to be attained, due to very few numbers of absentees when the research was carried out. UKM undergraduate and postgraduate dental students were predominantly made up of female students (~70% +). Data detailing the number of participants in each year was presented in Table 1. Years of working experience for UG2, UG3, UG4, UG5 students were 1, 2, 3 and 4 years and, respectively while PG students had 8.40(±1.718) years of experiences. With regards to the hours of working, UG2 students has the least working hours [13.31(± 2.222)], followed by UG3 [20.75(± 3.054)], UG4 [22.58(± 3.488)] and UG5 [25.28(± 3.483)]. PG students had the longest working hours which was 35.97(± 4.194) (Table 2).
| UG2 | UG3 | UG4 | UG5 | PG | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||
| Gender | Male | 15 | 27.80% | 15 | 28.80% | 11 | 22.90% | 16 | 28.10% | 9 | 27.30% |
| Female | 39 | 72.70% | 37 | 71.20% | 37 | 77.10% | 41 | 71.90% | 24 | 72.70% | |
| Age | Range | 20- 22 | 21-24 | 23-25 | 23-26 | 29-38 | |||||
| Mean | 21.07(±0.381) | 22.17(±0.474) | 23.23(±0.472) | 24.37(±0.587) | 33.03(±1.723) | ||||||
Table 1: Demographic data.
| UG2 | UG2 | UG3 | UG4 | UG5 | PG | |
|---|---|---|---|---|---|---|
| Years of working experience(n) | - | 1 | 2 | 3 | 4 | 10-May |
| Mean | - | - | - | - | 8.40(±1.718) | |
| Hours of working (n) | - | 10-16 | 17-26 | 18-27 | 20-30 | 30-40 |
| Mean | 13.31(±2.222) | 20.75(±3.054) | 22.58(±3.488) | 25.28(±3.483) | 35.97(±4.194) |
Table 2: Years of working experience and hours of working.
The consistently reported body regions with high rates of MSD for all participants were the neck (65.6%), the lower back (56.6%) and the shoulder (52.9%) (Figure 1). Elbow pain was the least commonly reported region of MSD among students, with only 7.8% of them were affected (Figure 1).
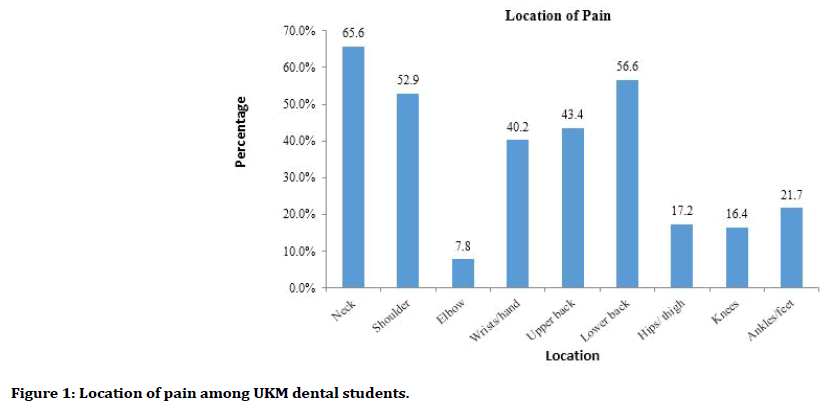
Figure 1. Location of pain among UKM dental students.
The prevalence of MSDs by body region for all postgraduate programmes was presented in Figure 2. Students studying paediatric had the highest prevalence of MSD, with 80.0% of them were suffered from neck, shoulder and lower back pain. In contrast, students studying oral and maxillofacial surgery (OMFS) had the least prevalence of MSD, with only 50.0% suffered from lower back pain and none of them (0.0%) had neck and shoulder pain. Endodontic and periodontic students reported the highest prevalence of neck pain (83.3%). Shoulder pain was most developed in paediatric students (80.0%). Most of the postgraduate programmes showed high prevalence in lower back pain (83.3%, 80.0% and 80.0% of periodontic students, paediatric students and orthodontic students, respectively).
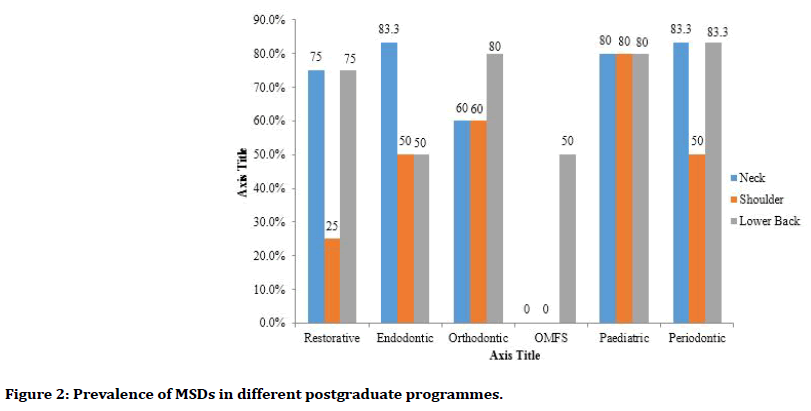
Figure 2. Prevalence of MSDs in different postgraduate programmes.
Figure 3 showed prevalence of MSD based on years of working experience. The prevalence of neck pain increased based on years of experience. Students with 1 year of working experience had the least neck pain (59.6%) while students with more than 5 years of working experience had the most neck pain (72.2%). Lower back pain had a direct correlation with years of experience too. Lower back pain affected student with 1 year of working experience was the least (40.5%) while affected students with more than 5 years of experience was the most (71.8%). Both neck and lower back pain showed an increasing pattern of pain based on years of experience. However, the prevalence of shoulder pain was the highest in students with 3 years of working experience (70.5%). The pattern of MSD in shoulder pain was increased from 1 to 3 years of working experience, followed by decreased from 3 to more than 5 years of working experience.
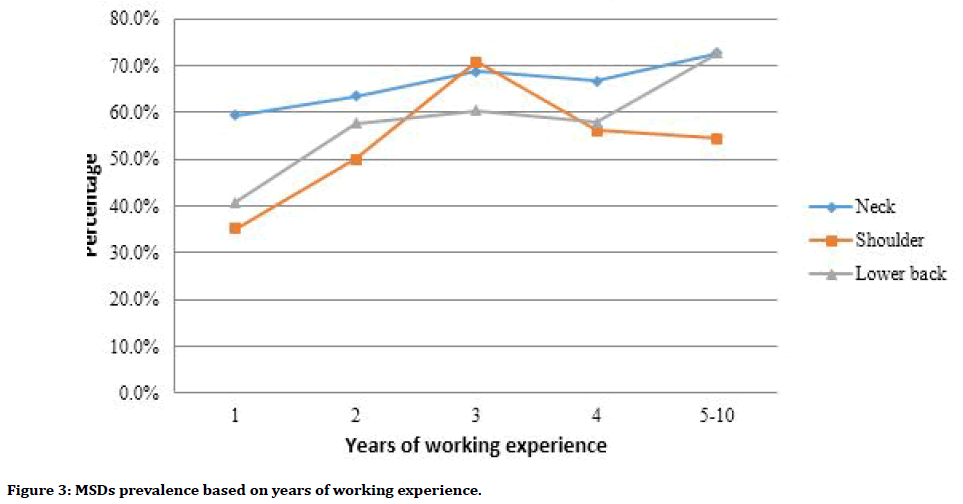
Figure 3. MSDs prevalence based on years of working experience.
The changes in MSD prevalence in neck, shoulder and lower back, in comparison of different cohorts studied shown changes either increasing or decreasing. However, all the changes were insignificant as all their P values obtained through data analysis were less than 0.05.
Discussion
The incidence of musculoskeletal problems, especially work-related is increasing. One of the occupations that are encountering with these problems are dentists [14,15]. In current study, it was found that most of the dental students had symptoms of MSDs. Similar studies conducted by different researchers have shown similar results [16]. It was found that 86.6% of all students surveyed suffered from MSD associated with clinical requirements of their training. Movahhed et al. reported that 82% of undergraduate students and 90% of postgraduate students reported pain in at least one body region [17]. This finding suggests that oral health professionals may have an increased risk of developing MSD even before the starting of a professional career.
Cross-sectional studies measure exposures and outcomes at a single point in time, and, as such, are useful for yielding prevalence estimates. This study design is efficient in terms of cost and time, as it allows several factors to be studied; given that this project is required to be completed in less than 12 months, a cross-sectional approach was considered the most appropriate choice.
Majority of the participants in this study were females. Since the proportions of male students were small in our study, it was not appropriate to determine the differences in musculoskeletal pain prevalence rates by gender. This was since the intake of dental students of UKM was dominated by females.
Site of MSD in the current study was mostly neck, followed by lower back and shoulders and this is supported by other study [18]. Study conducted by Rehman et al. also reported that lower back (57.8%), neck (37.5%) and shoulders (29.6%) were the three commonly affected sites of dental practitioners [19]. In another studied also found that neck (69%) was the predominant site of pain followed by shoulders (51%), upper back (51%) and lower back (39%) [20]. The results of study by Gupta et al. shows the neck pain with the most prevalence rate (57.5%) and back pain with moderate prevalence rate (53.7%) [21].The variations in reported prevalence may be due to issues such as various measurement methods, cultural differences and the individual’s tasks. High level of incidence in this group may be related to ergonomic problems such as unsuitable repetitive movements [22], using vibrating instruments, bending forward at an angle of 15° or sometimes up to 30° for a long time (in 86% of the working time) with keeping up shoulder that caused a lot of pressure on the neck and shoulder [8].
The distribution of pain was different in postgraduate students (PG) from different specialized field in dentistry. In our studies, students studying paedodontics had the highest prevalence of MSD. This result also supported by other study which reported paedodontists seemed to be at the most risk of developing musculoskeletal disorder with 91% of them reporting some work-related pain [23]. Aghahi et al. stated that musculoskeletal pain in pedodontists might be due to not placing children in a proper position, the lack of a special unit for children, lack of good vision, lack of patient cooperation and striving for greater control [24]. In our study, OMFS students had the lowest prevalence of MSDs. However, this may due to a very small sample size of OMFS students which was only two students. In orthodontics, 80% of students reported pain in lower back region. In endodontic students, the neck region was reported to be a major area of pain. In restorative students and periodontics students, pain in the neck and lower back was the most reported MSD. Such differences in the prevalence of various MSDs among dentists from different specialties have been observed in previous studies [25] and can be accounted for by the difference in nature of the duties they perform and whether they have direct patient contact or not.
Figure 3 showed the prevalence of MSD in neck, shoulder and lower back based on years of working experience as these areas were most reported areas of pain in correlates with other studies. A study showed that the most prevalent MSD in dentist during the previous 12 months were reported at the neck (57.5%), lower back (53.7 %) and shoulder (53.3%) [8]. Neck and lower back showed the highest prevalence of MSD in subjects with 5 to 10 years of experience doing work, which was the postgraduate cohort, as detailed in Figure 3. In comparison with PG, UG2 (1 year of working experience) had the lowest prevalence of MSD in neck and lower back. Khan et al. reported there was an increase in pain prevalence with the number of years spent in the dental school and this was more related to students which were in clinical years, acquiring clinical skills and doing the routine dental procedures [13].
The gradual increases of prevalence of MSD in neck, shoulder and lower back from UG2 to UG4 can be hypothesized that it was due to the changes in nature of work, practicing pattern and working hours based on the timetable and curriculum of respective cohorts. UG2 students had the lowest MSD prevalence as they did not have any clinical session of treating patients yet and were only started to be introduced towards simulation practice on dummy and prosthetic laboratory work. The least prevalence of MSD in UG2 can also due to the ergonomics subject that was taught in their curriculum and the supervisor that kept on emphasized more on their posture during the simulation practices. UG3 (2 years of working experience) was the year they start to have their clinical session and start to treat real life patient. Hence, their prevalence of MSD increased, and this was probably due to their difficulty in adaptation towards changes from doing simulation practice on dummy and clinical work on actual patient. The prevalence of MSD in shoulder for UG3 showed a drastic increase in comparison with neck and lower back. This may be due to the introduction of Prosthodontic clinical work, which required the student to work with arms above the shoulder and forceful arm movements.
Regarding UG4 (3 years of working experience), the prevalence of MSD continues to increase as they were introduced to more different and various clinical works and practices such as Periodontology, Orthodontic, Paediatric, Oral surgery and Oral Pathology and Medicine and also increase in working hours. Interestingly, the prevalence of MSD in neck, shoulder and lower back among UG5 (4 years working experience) decreased in compare to the UG4. This might be due changes and adaptation in work posture to avoid problem or muscle pain/ache aided by the experiences gaining through clinical work.
In comparison to UG5, PG (5 to 10 years of experience doing work) showed higher MSD prevalence in neck and lower back region with the lower back region having more steeply increases. This correlated with other study which stated that MSDs were most commonly reported in the neck (66 to 68%) and lower back (61 to 68%), with a marked increase in reported lower back pain by the final year of study [14]. This was most probably due to PG having longer hours doing clinical practice and the nature of clinical work of PG were more complicated and require more precise handling of instruments. These factors might contribute to compromised ergonomics such as bending/ twisting of neck, unsupported lower back, and prolong awkward posture. A prolonged static postures with increased disk pressures and spinal hypomobility, may lead to degenerative changes within the lumbar spine and low back pain or injury [6]. In addition, the lack of awareness and education regarding importance of practicing correct ergonomics might also lead to this finding. A study showed that 58% of the students indicated that ergonomics had not been a taught subject in their curriculum while 93% of students had never attended a workshop on preventing MSD at their dental school [5].
However, it was interesting to find that PG showed a decrease in prevalence of MSD in shoulder in comparison to UG5 although the neck and lower back show increased prevalence. A study showed that the neck and lower back were most prevalence for MSD while the shoulder was less likely affected as the pain usually more concentrated in lower back and spread to shoulder because the lower back provided the basis for work in sitting position [26]. For all the comparison among different cohorts in various body parts as in Figure 3, the changes obtained were all insignificant. This might be due to the provision of ergonomics as a subject in curriculum during undergraduate studies. It can also because of there is no significant difference in working hours among the cohorts. Therefore, further research on influence of ergonomics education including early monitoring and teaching of correct posture towards MSD, and research on other risk factors of MSD should be carry out in future.
Conclusion
Dental students were reporting MSD at rates on par with professional dental practitioner, suggesting that MSD could be developed well before the beginning of a professional dental career. The high prevalence of MSD among dental students highlighted the need for further emphasis to be placed on ergonomic education throughout their undergraduate and postgraduate studies.
References
- Gupta A, Manohar Bhat TM, Bansal N, et al. Ergonomics in dentistry. Int J Clin Pediatr Dent 2014; 7:30-34.
- Punnett L, Wegman DH. Work-related musculoskeletal disorders: The epidemiologic evidence and the debate. J Electromyography Kinesio 2004; 14:13-23.
- Kumar SP, Kumar V, Baliga M. Work-related musculoskeletal disorders among dental professionals: An evidence-based update. Indian J Dent Educ 2012; 5:5-12.
- Hayes MJ, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hygiene 2009; 7:159-165.
- Khan SA, Chew KY. Effect of working characteristics and taught ergonomics on the prevalence of musculoskeletal disorders amongst dental students. BMC Musculoskeletal Disorders 2013; 14:118.
- Valachi B, Valachi K. Mechanisms leading to musculoskeletal disorders in dentistry. J Am Dent Assoc 2003; 134:1344-1350.
- Cailliet R. Soft tissue pain and disability. 3rd Edn. Philadelphia; 1996.
- Leggat PA, Kedjarune U, Smith DR. Occupational health problems in modern dentistry: A review. Industrial Health 2007; 45:611-621.
- Al-Ali K, Hashim R. Occupational health problems of dentists in the United Arab Emirates. Int Dent J 2012; 62:52-56.
- Morse T, Bruneau H, Dussetschleger J. Musculoskeletal disorders of the neck and shoulder in the dental professions. IOS Press 2010; 35:419-429.
- Chowanadisai S, Kukiattrakoon B, Yapong B, et al. Occupational health problems of dentists in southern Thailand. Int Dent J 2000; 50:36-40.
- Rising DW, Bennett BC, Hursh K, et al. Reports of body pain in a dental student population. J Am Dent Assoc 2005; 136:81-86.
- Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders and symptom severity among Australian dental hygienists. BMC Res Notes 2013; 6:250.
- Ebrahimian H, Hokmabadi R, Shoja E. Evaluation of ergonomic postures of dental professions by rapid entire body assessment (REBA) in North Khorasan, Iran. J North Khorasan 2014; 5:961-967.
- Droeze EH, Jonsson H. Evaluation of ergonomic interventions to reduce musculoskeletal disorders of dentists in the Netherlands. Work 2005; 25:211-220.
- Limaye V, Limaye D, Desai R, et al. Prevalence of musculoskeletal disorders among dentists from Mumbai, India. Current Therapeutic Res 2016; 78:11.
- Movahhed T, Ajami B, Soltani M, et al. Musculoskeletal pain reports among Mashhad dental students, Iran. Pakistan J Bio Sci 2013; 16:80-85.
- Rasidi M, Zaki MQ, Gheena S. Awareness on musculoskeletal disorder among dental students in Chennai. Int J Current Res 2016; 8:43868-43873.
- Rehman K, Ayaz H, Urooj W, et al. Work-related musculoskeletal disorders among dental practitioners in Khyber Pakhtunkhwa. Pakistan Oral Dent J 2013; 33:531-534.
- Moosavi S, Desai R, Hallaj S, et al. Ergonomic analysis to study the intensity of MSDs among practicing Indian dentists. Procedia Manufacturing 2015; 3:5419-5426.
- Gupta A, Ankola AV, Hebbal M. Dental ergonomics to combat musculoskeletal disorders: a review. Int J Occupational Safety Ergonomics 2013; 19:561-571.
- Lake J. Musculoskeletal dysfunction associated with the practice of dentistry: Proposed mechanisms and management: Literature review. University Toronto Dent J 1995; 9:7-9.
- Alghadir A, Zafar H, Iqbal ZA. Work-related musculoskeletal disorders among dental professionals in Saudi Arabia. J Phy Therapy Sci 2015; 27:1107-1112.
- Aghahi RH, Darabi R, Hashemipour MA. Neck, back, and shoulder pains and ergonomic factors among dental students. J Educ Health Promotion 2018; 7:1-6.
- Alexopoulos EC, Stathi IC, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskeletal Disorders 2014; 5:16.
- Lalumandier JA, McPhee SD, Parrott CB, et al. Musculoskeletal pain: prevalence, prevention, and differences among dental office personnel. Gen Dent 2001; 49:160-166.
Author Info
Noor Sam Ahmad1*, Asma Alhusna Abang Abdullah1, Ooi Kee Thyng2 and Teong Ling Xin2
1Department of Family Dental Health, Orthodontic Unit, Faculty of Dentistry, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia2Doctor of Dental Surgery (DDS). Ministry of Health, Malaysia
Citation: Noor Sam Ahmad, Asma Alhusna Abang Abdullah, Ooi Kee Thyng, Teong Ling Xin, Musculoskeletal Disorders Among Dental Students, J Res Med Dent Sci, 2020, 8(3): 32-38
Received: 28-Jan-2020 Accepted: 20-Apr-2020
