Research - (2021) Volume 9, Issue 4
Necrotizing Fasciitis: A Clinical and Microbiological Study
J Magesh Kumar, RNM Francis and V Ramalakshmi*
*Correspondence: V Ramalakshmi, Department of General Surgery, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, India, Email:
Abstract
Objective: Necrotizing fasciitis (NF) is a prolong inflammation of the soft tissue and prevalent with higher morbidity and mortality. The treatment would be based on the surgical debridement and antibiotic therapies.
Methods: All cases of Necrotizing fasciitis admitted in Sree Balaji Medical College & Hospital, Chennai-44 between the period of November 2014 and October 2016 were included in the study. The diagnosis was made by combination of clinical and gross anatomical findings, biochemical characterization, and microbiological evaluation.
Results: The male predominance was found among the patients. The pain was presented as most common symptom (95%) and mean duration was 10.08 days. Trauma contributed as most common etiological factors (30%) and Diabetes mellitus was the most common associate comorbid condition (38.3%) in patients, followed by hypertension in 18 patients (30%). The culture was monomicrobial in 37 (61.7%) patients, polymicrobial in 22 (36.7%) patients and sterile in 1.7% of patients. 86.7% of isolates were aerobic and 13.3% were anaerobic in nature. E. coli was the commonest bacteria among the patients.
Conclusions: In severe cases the combination of necrotic skin and soft tissue gas facilitates the correct diagnosis, which should than be followed by immediate - and most often-repeated debridement. The anaerobes are isolated an early and aggressive second look is necessary. The finding of the study would be especially useful for therapeutic planning.
Keywords
Necrotizing fasciitis, Soft tissue infection, Diabetes mellitus, Comorbid condition, Trauma
Introduction
Necrotizing fasciitis is a progressive, quickly spreading inflammatory infection located in deep fascia usually occurring in skin and subcutaneous tissue and could spread over to adjacent soft tissues such as muscles (i.e., necrotizing myositis). It propagates to other sites via the blood vessels and resulting in severe shock, organ failure and death. Its prevalence is higher in adults than the children (0.4 and 0.08/100,000 for adults and children respectively). The incidence is seemed to be increased in recent years due to altered physiology such as immuno deficiency, diabetes mellitus, complement C4 deficiency, AIDS, malignancies, and drugs etc.,
The diabetic patient usually faces complications such as large vessels atherosclerosis, micro vascular disease of diabetes and diabetic neuropathy. The patients with vasculopathy and neuropathy are more prone to predispose for foot ulceration. Prolonged ulcers lead to the microbial contamination at the sites and eventually resulting in deep site necrosis and complex infectious process. The diabetic neuropathy leads to neuron loss, pressure ulceration and inadequate cutaneous blood supply. These change the net results for higher secondary invasive infection. These lesions enter into the deep spaces of the leg; true climbthreatening circumstance exists. Each factor that influences the health and integrity of the skin or mucus membranes can result in penetration of infection. Primary infection can penetrate due to skin trauma, infected needle in intravenous drug abusers or previous dermatological diseases such as psoriasis and Bed sore. Mucosal membranes in gastrointestinal or genitourinary systems are the other routes of infection [1-9].
The present study aimed to identify the frequency of Necrotizing Fasciitis in Sree Balaji Medical College and Hospital, Chrompet, Chennai for determining the effective therapeutic strategy on necrotizing fasciitis.
To analyze the clinical presentation in patients with Necrotizing fasciitis. To determine the predisposing factors related to Necrotizing fasciitis. To define the relationship of Co morbid diseases with Necrotizing fasciitis. To analyze the microbiological parameters on Necrotizing fasciitis. To analyze the Surgical and resuscitative management.
Materials and Methods
The present study is a kind of descriptive study on Necrotizing fasciitis and involved a single group of patients admitted in Sree Balaji Medical College & Hospital, Chennai between the period of November 2014 and October 2016. The study was conducted after the proper ethical approval.
Inclusion criteria
All cases of Necrotizing fasciitis admitted in Sree Balaji Medical College & Hospital, Chennai-44 between the period of November 2014 and October 2016.
Exlcusion criteria
All patients with necrotizing fasciitis leaving before the completion of the treatment.
Methodology
Patients with Necrotizing fasciitis were included in the present study. The diagnosis was made by combination of clinical and gross anatomical findings during the surgery. Demographic data was collected and the pre medical history such as diabetes mellitus, antibiotic usage was recorded. The vital parameters and physical examination was performed to look for any bullae formation. The blood parameters such as Hemoglobin, Platelets, RBS, Urea, creatinine, Sodium and Potassium levels, Radiograph were done to analyze the subcutaneous gas formation. Treatment including hemodynamic stabilization, blood-spectrum antibiotics and aggressive wound debridement were given to the patients. The microbial culture and sensitivities were taken from the infected wound during debridement or fasciotomy, particularly to test for aerobic and anaerobic organisms. The Microbial analyses were adopted from the CLSI (Clinical and Laboratory Standards Institute) guidelines. The tissue sample or the wound swab was inoculated in RCM (Robertson's Cooked Meat) media for further anaerobic culture and identification.
Statistical analysis
The statistical software namely, Statistical Package for the Social Sciences software, SPSS 15.0(SPSS Inc., Chicago, IL), and R environment ver.2.11.1 were used in the study.
Results
The present study was carried out with 60 patients diagnosed with Necrotizing Fasciitis admitted to Sree Balaji Medical College and Hospital, Chromepet. The age of the studied patients was ranged between 29 -81 years. There were 49 males and 11 females, the male: female ratio being 4:45:1. The mean age was 50.42 ± 17.31 years. Maximum cases were above the age of 50 years (Table 1 and Figure 1). The occupation plays a significant role in diseases. In the present study, out of the 60 patients, 17 (28.3%) were farmers by occupation. 10 (16.7%) were housewives (Table 2). The study showed that the disease severity could be correlated with the occupation.
| Male | Female | Total | ||||
|---|---|---|---|---|---|---|
| Age in years | No | % | No | % | No | % |
| <20 | 2 | 4.1 | 2 | 18.2 | 4 | 6.7 |
| 21-30 | 1 | 2.1 | 1 | 9.1 | 2 | 3.3 |
| 31-40 | 10 | 20.4 | 2 | 18.2 | 12 | 20 |
| 41-50 | 7 | 14.3 | 1 | 9.1 | 8 | 13.3 |
| 51-60 | 14 | 28.6 | 3 | 27.3 | 17 | 28.3 |
| >60 | 15 | 30.6 | 2 | 18.2 | 17 | 28.3 |
| Total | 49 | 0 | 11 | 100 | 60 | 100 |
| Mean ± SD | 52.27 ± 17.1 | 42.18 ± 16.71 | 50.42 ± 17.31 | |||
| (P=0.081+, Lower age was statistically significant for female with P=0.081+) | ||||||
Table 1: Age and gender distribution of necrotizing fasciitis in the study.
| Occupation | Number of patients | % |
| Farmer | 17 | 28.3 |
| Housewife | 10 | 16.7 |
| Unskilled | 12 | 20 |
| Service | 9 | 15 |
| Skilled | 10 | 16.7 |
| Not applicable | 2 | 3.3 |
| Total | 60 | 100 |
Table 2: Occupation of patients participated in the study.
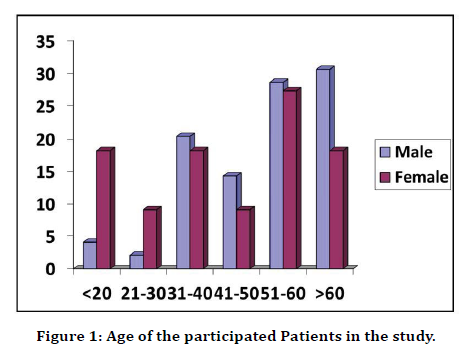
Figure 1. Age of the participated Patients in the study.
The study showed that lower limb was the most common site involved in 32 (53.3%) patients followed by the perineum in 18 (30%) patients and trunk in 5 (8.3%) patients (Table 3 and Figure 2). Regarding symptoms, pain was present in most of the cases 57(95%). Fever and discharge was present in 37(61.7%) & 35(58.3%) respectively. Swelling in 27(45%) and blisters/ skin vesicles in 11(18.3%) were also noted (Table 4 and Figure 3). Thirty-three patients (55%), presented within a week, 19(31.7%) in 2 weeks and 8(13.3%) beyond 2 weeks. Mean duration of symptoms was 10.08 ± 10.09 days (Table 5 and Figure 4). Clinical signs of oedema and ulcer was present in 51(85%) & 46(76.7%) respectively (Table 6 and Figure 5). Trauma was the most common etiological factors comprising of 18(30%) patients. No predisposing factor was present in 4(6.7%) patients. The diversification of etiological factors is mentioned in Table 7 and Figure 6.
| Site | Number of Patients | % | 95%CI |
|---|---|---|---|
| Lower limb | 32 | 53.3 | 40.89-65.37 |
| Perineum | 18 | 30 | 19.90-42.61 |
| Trunk | 5 | 8.3 | 3.61-18.07 |
| Upper limb | 4 | 6.7 | 2.62-15.93 |
| Anterior Abdominal wall | 1 | 1.7 | 0.3-8.96 |
| Total | 60 | 100 | - |
Table 3: Site of infection in the patients (Confidence Interval with lower limit more than 50% was associated with statistical significance).
| Symptoms | Number of patients (n=60) | % | 955CI |
|---|---|---|---|
| Pain | 57 | 95 | 86.30-98.29 |
| Fever | 37 | 61.7 | 49.62-72.91 |
| Discharge | 35 | 58.3 | 45.73-69.94 |
| Swelling | 27 | 45 | 33.09-57.51 |
| Blisters/Skin Vesicles | 11 | 18.3 | 10.56-29.52 |
| Hyper pigmentation/Hard Texture of skin | 8 | 13.3 | 6.91-24.17 |
Table 4: Symptoms at Presentation in the patients.
| Duration of symptoms | Number of patients(n=60) | % |
|---|---|---|
| 1-7 days | 33 | 55 |
| 8-14 days | 19 | 31.7 |
| >14 days | 8 | 13.3 |
| Mean ± SD: 10.08 ± 10.09 | ||
Table 5: Duration of symptoms in the patients.
| Signs | Number of patients (n=60) | % | 95%CI |
|---|---|---|---|
| Pallor | 6 | 10 | 3.61-18.07 |
| Oedema | 51 | 85 | 73.89-91.90 |
| Ulcer | 46 | 76.7 | 64.56-85.56 |
| Lymph Adenopathy | 11 | 18.3 | 10.56-29.92 |
Table 6: Signs in the patients.
| Etiology | Number of patients(n=60) | % | 95%CI |
|---|---|---|---|
| Trauma | 18 | 30 | 19.90-42.61 |
| Alcoholism | 8 | 13.3 | 6.91-24.17 |
| Native drug allergy | 9 | 15 | 8.10-26.11 |
| RTA | 6 | 10 | 4.86-20.15 |
| Insect bite | 6 | 10 | 4.86-20.15 |
| Thorn prick | 4 | 6.7 | 2.62-15.93 |
| Post-surgery | 3 | 5 | 1.71-13.70 |
| Injection | 2 | 3.3 | 0.9-11.36 |
| Abrasion | 1 | 1.7 | 0.3-8.86 |
| Eczema | 1 | 1.7 | 0.30-8.86 |
| Episiotomy sepsis | 1 | 1.7 | 0.30-8.86 |
| Septic abortion | 1 | 1.7 | 0.30-8.86 |
| IR Rays | 1 | 1.7 | 0.30-8.86 |
| Idiopathic | 4 | 6.7 | 2.62-15.93 |
Table 7: Etiology in the patients.
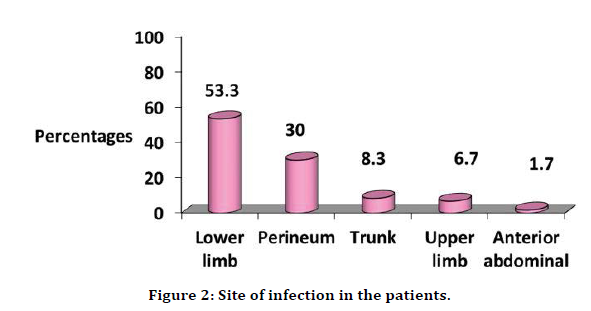
Figure 2. Site of infection in the patients.
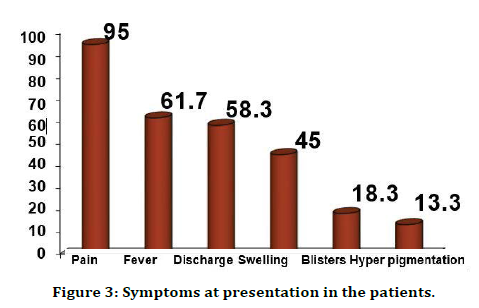
Figure 3. Symptoms at presentation in the patients.
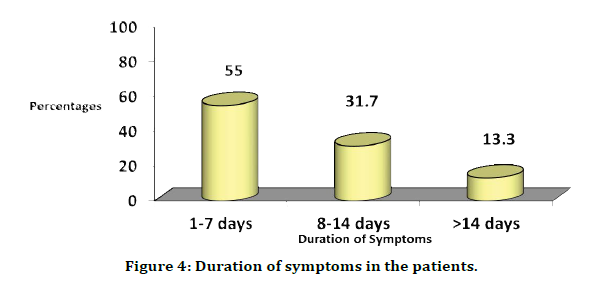
Figure 4. Duration of symptoms in the patients.
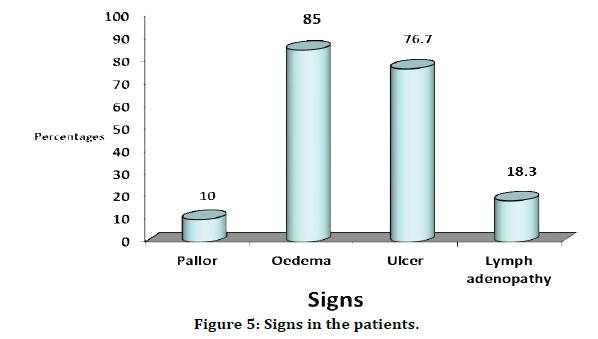
Figure 5. Signs in the patients.
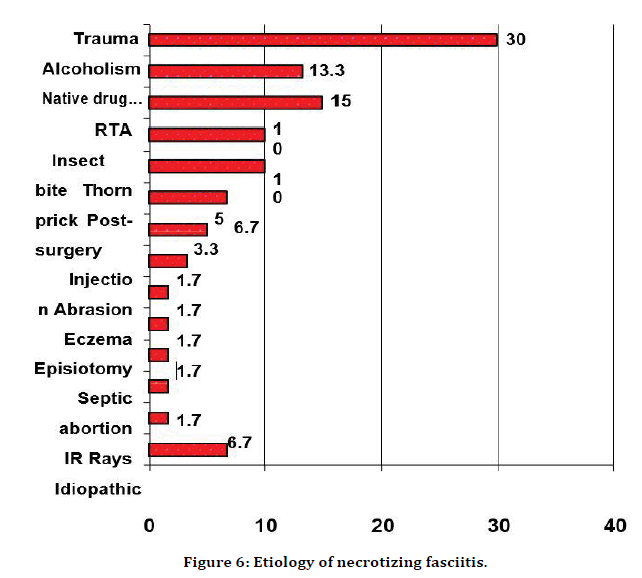
Figure 6. Etiology of necrotizing fasciitis.
Diabetes mellitus was the most common associate comorbid condition comprising of 23(38.3%) patients, followed by hypertension in 18 patients (30%). Two of the patients in this study were HIV positive (Table 8 and Figure 7). The laboratory parameters were evaluated. It was observed that 11(18.3%) patients had hemoglobin <10gm%, 18(30%) has RBS >180md/dl, 14(23.3%) had serum creatinine>1.6mg/dl and 9(15%) with sodium levels. <128mEq/l, which are all risk indicators as describes by a recently developed Laboratory Risk Indicator score for necrotizing fasciitis (LRINEC)by Wong et al. [6] (Table 9 and Figure 8).
| Associated Co morbid conditions | Number of patients(n=60) | % |
|---|---|---|
| 1.DM | 21 | 38.3 |
| 2.Hypertension | 18 | 30 |
| 3.Smoking | 11 | 18.3 |
| 4.CKD | 9 | 15 |
| 5.COPD | 8 | 13.3 |
| 6.CAD | 6 | 10 |
| 7.Cirrhosis | 3 | 5 |
| 8.HIV | 2 | 3.3 |
| 9.Tuberculosis | 2 | 3.3 |
| 10.Anemia | 1 | 1.7 |
| 11.Eczema | 1 | 1.7 |
| 12.Osteo arthritis | 1 | 1.7 |
| 13.Sepsis | 1 | 1.7 |
| 14.Idiopathic | 10 | 16.7 |
Table 8: Associated co morbid conditions.
| Blood parameters | Number of patients (n=60) | % | 95 %CI |
|---|---|---|---|
| Hemoglobin gm% | |||
| <10 | 11 | 18.3 | 10.66-29.92 |
| >=10 | 49 | 81.7 | 70.08-89.44 |
| RBS mg/dl | |||
| <180 | 42 | 70 | 57.49-80.10 |
| >=180 | 18 | 30 | 19.90-42.51 |
| Serum Creatinine mg/dl | |||
| <1.6 | 46 | 76.7 | 64.56-85.66 |
| >=1.6 | 14 | 23.3 | 14.44-35.44 |
| Sodium mEq/L | |||
| <128 | 9 | 15 | 8.10-26.11 |
| >=128 | 51 | 85 | 73.89-91.90 |
Table 9: Laboratory investigations on admission.
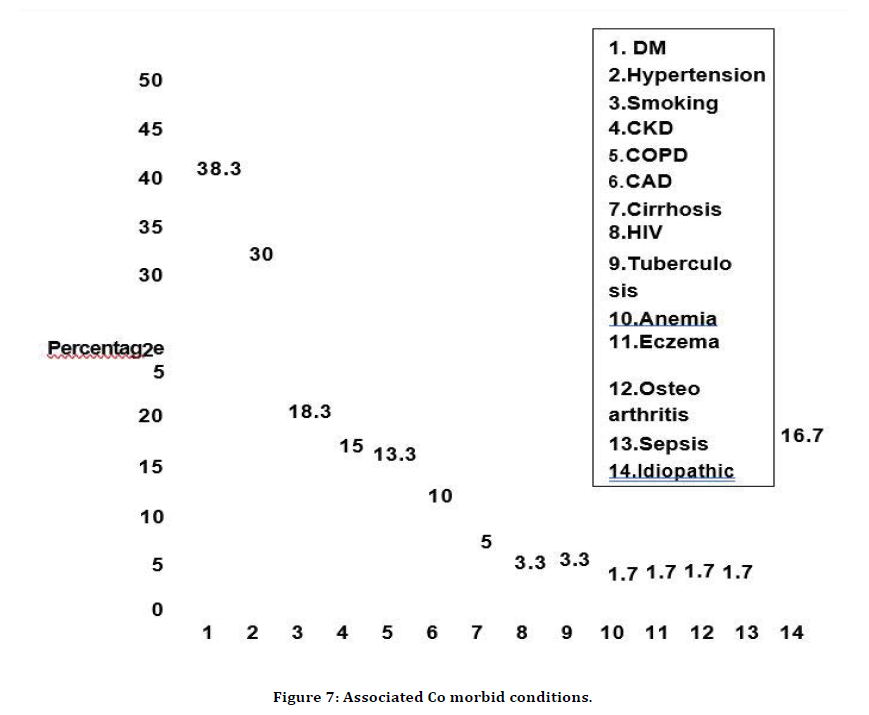
Figure 7. Associated Co morbid conditions.
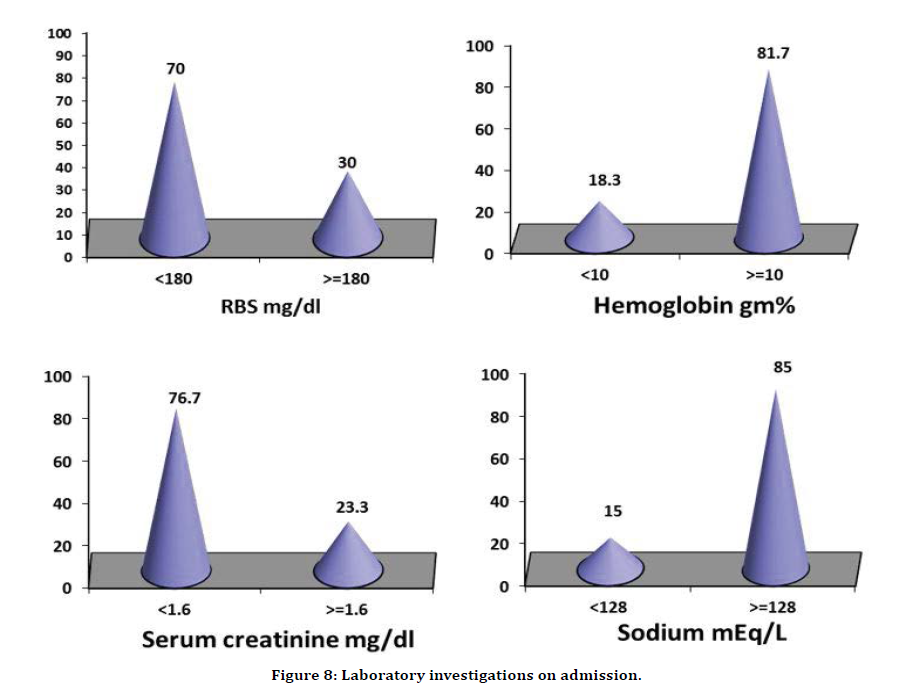
Figure 8. Laboratory investigations on admission.
The culture was monomicrobial in 37 (61.7%) patients, polymicrobial in 22 (36.7%) patients and sterile in (1.7%) patients. Among these 52 (86.7%) isolates were aerobic and 8(13.3%) were anaerobic. (Table 10 and Figure 9). The commonest bacteria isolated were E. coli in 21(35%) patients followed by P. Aeruginosa in 14(23.3%) patients and L. Pneumonia in 11(18.3%) patients (Table 11). Patients were initially given broad spectrum antibiotic combination with second or third generation cephalosporin +/- aminoglycosides+metronidazole followed by culture-based antimicrobials.
| Bacteriological Study | Number of patients(n=60) | % | 95%CI |
|---|---|---|---|
| Monomicrobial | 37 | 61.7 | 49.02-72.91 |
| Polymicrobial | 22 | 36.7 | 25.62-49.32 |
| Sterile | 1 | 1.7 | 0.3-8.86 |
| Aerobic | 52 | 86.7 | 75.83-93.09 |
| Anaerobic | 8 | 13.3 | 6.91-24.17 |
Table 10: Bacteriological study of the specimen tissue.
| Commonly Identified Bacteria | Number of patients(n=60) | % |
|---|---|---|
| E. Coli | 21 | 35 |
| P. Aeruginosa | 14 | 23.3 |
| K. Pneumoniae | 11 | 18.3 |
| P. Mirabilis | 7 | 11.7 |
| Cons | 6 | 10 |
| S. Aureus | 6 | 10 |
| MRSA | 5 | 8.3 |
| P. Vulgaris | 5 | 8.3 |
| Citrobacter | 4 | 6.7 |
| NFGNB | 4 | 6.6 |
| B.H. Streptococci (Gr. A) | 4 | 6.6 |
| Acinetococcus | 3 | 5 |
| Peptococcus | 3 | 5 |
| Fusobacterium | 2 | 3.3 |
| P. Species | 2 | 3.3 |
| Psuedomonas | 2 | 3.3 |
| Anaerobic cocci | 1 | 1.7 |
| Bacteriods | 1 | 1.7 |
| Citrobacter Freundii | 1 | 1.7 |
| Enterobacter | 1 | 1.7 |
| Enterococci | 1 | 1.7 |
| P. Streptococcus | 1 | 1.7 |
| CONS: Coagulase Negative Staphylococcus | ||
| MRSA: Methicillin Resistant Staph Aureus | ||
| NFGNB: Non-Fermenting Gram Negative Bacilli | ||
| Group A BH: Group A Beta Haemolytic Streptococci | ||
Table 11: Commonly identified bacteria.
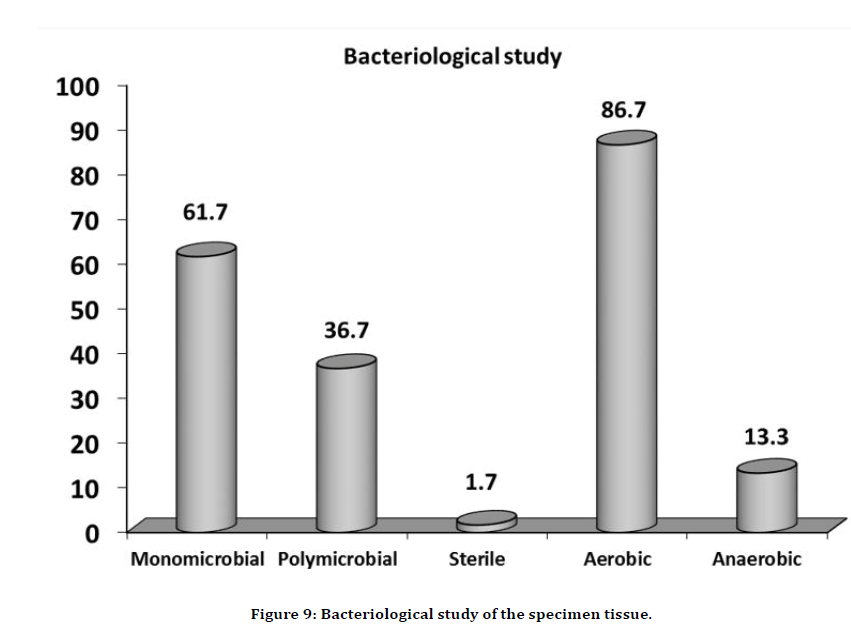
Figure 9. Bacteriological study of the specimen tissue.
Surgical treatment included debridement’s in 57(95%), Fasciotomy 3(5%), followed by Split skin grafting in 21(35%) and secondary suturing in 17(28.3%) (Table 12 and Figure 10). Duration of hospital stay, 9 patients stayed for more than 30 days (Table 13 and Figure 11). The mortality rate was nil (0%).
| Treatment | Number of patients | % |
|---|---|---|
| Debridement | 57 | 95 |
| Fasciotomy | 3 | 5 |
| Split Skin Graft | 2 | 35 |
| Secondary Suturing | 17 | 28.33 |
Table 12: Treatment.
| Hospital stays in days | Number of patients(n=60) | % |
|---|---|---|
| <7 days | 1 | 1.7 |
| 7-14 days | 12 | 20 |
| 15-21 days | 25 | 41.7 |
| 22-30 days | 13 | 21.7 |
| >30 days | 9 | 15 |
Table 13: Hospital stay in days of studied patients.
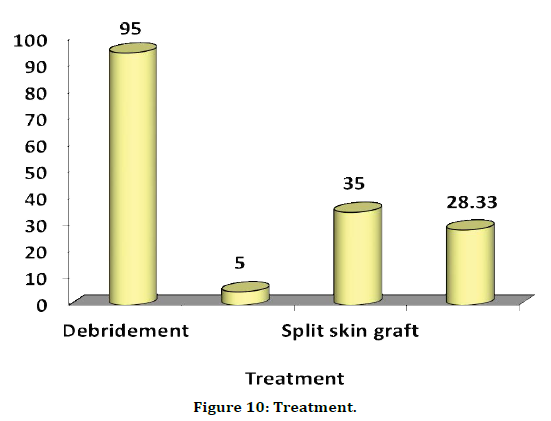
Figure 10. Treatment.
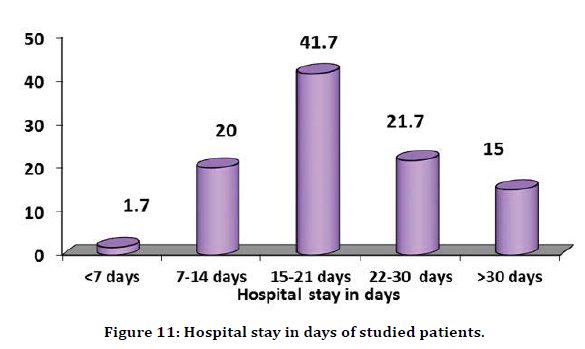
Figure 11. Hospital stay in days of studied patients.
Discussion
The present aimed to analyze the incidence and prevalence of Necrotizing fasciitis in hospitalized patients. Necrotizing fasciitis usually associated with hypotension, fever, tachycardia, tachypnea and laboratory findings of leukocytosis and metabolic acidosis are indices of development of sepsis. Our study showed that age was one of the main factors to determine the severity of the disease. The results also revealed the male predominance, and it might be due to increased incidence of trauma and outdoor activity. Our results coinciding with the previous studies by Wilkerson et al. [10] and Childer et al. [11]. Necrotizing fasciitis is known to follow minor trauma, insect bite, pustule or minor operations, anorectal abscess, instrumentation, septic abortion, genitourinary infection. In our study majority of the patients had a predisposing factor and majority (30%) was due to trauma. No etiological factor was present in the patients. Primary or idiopathic Necrotizing fasciitis occurs in the absence of a known or identificable etiologic factor. The underlying pathogenesis of idiopathic Necrotizing fasciitis is still unknown.
These findings were coincidence with Mukhopadhyay et al. [12]. In our study, lower limb (53.3%) and perineum (30%) were the commonest site involved. Other studies did not show similar results, perineum being the most common site. There may be a difference in the orunary site of infection due to a difference in the hygiene level. But Tian et al. [13] had shown the infection to be more common in the lower limbs, similar to our study. Diabetes mellitus was the most common co-morbid condition in our study (23%) which is co-relating with the previous report by Kobayashi et al. [14]. Other co-morbid factors associated with necrotizing fasciitis include chronic alcoholism, drug abuse, corticosteroid use, immune-suppression, AIDS, malignancy, chronic obstructive lung disease, chronic venous or lymph insufficiency, obesity, malnutrition, peripheral vascular diseases, tuberculosis, and leprosy. In our series, other co - morbid factors noted were: hypertension in 18 patients (30%), CKD in 9(15%), COPD in 8(13.3%), CAD in 6(10%), Cirrhosis in 3(5%), Tuberculosis in 2(3.3%). Two patients were HIV positive. Tian et al. [13] reported similar previously.
In our study majority of the patients (61.7%) had mono microbial infection. This does not correlate with other studies which showed that polymicrobial infection as the main flora. Among these 52 (86.7%) isolates were aerobic and 8(13.3%) were anaerobic. In our study E. Coli was the commonly identified and E. Coli was the most common bacterium isolated from necrotic tissue of diabetic patients. Others also demonstrated that E. Coli was one of the four common organisms isolated from Type I necrotizing fasciitis. Pseudomonas aeruginosa can be a fatal cause of necrotizing fasciitis. According to other studies P. aeruginosa was the most frequently isolated bacteria which represented 85% of 39 patients with necrotizing fasciitis. Broad spectrum antibiotics against gram positive, gram negative and anaerobic bacteria should be started early during treatment before culture reports are available. According to Wipf et al. [15] the single most important determinant of survival is the amount of time elapsed between initial presentation and surgical debridement. The present study had revealed the incidence and precaution measures for effective treatment on Necrotizing Fasciitis.
Conclusion
Necrotizing Fasciitis is a life-threatening soft tissue infection, characterized by severe necrosis and require critical diagnosis is critical to the survival of the patient and must rely on the clinical picture. The present study systematically analyzed the demographic relations, comorbidities, and related pathogenesis. This study showed that effective management of diabetes could be a suitable way to reduce the severity. Further, it showed the role debridement in eradicating the disease. These findings will be useful in treatment of NF.
References
- Sarani B, Strong M, Pascual J, et al. Necrotizing fasciitis: Current concepts and review of the literature. J Am Coll Surg 2009; 208:279.
- Anaya DA, Dellinger EP. Necrotizing soft-tissue infection: Diagnosis and management. Clin Infect Dis 2007; 44:705-710.
- Anaya DA, McMahon K, Nathens AB, et al. Predictors of mortality and limb loss in necrotizing soft tissue infections. Arch Surg 2005; 140:151-157.
- Boyer A, Vargas F, Coste F, et al. Influence of surgical treatment timing on mortality from necrotizing soft tissue infections requiring intensive care management. Intensive Care Med 2009; 35:847-853.
- McHenry CR, Piotrowski JJ, Petrinic D, et al. Determinants of mortality for necrotizing soft- tissue infections. Ann Surg 1995; 221:558-563.
- Wong CH, Chang HC, Pasupathy S, et al. Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am 2003; 85:1454-1460.
- Hsiao CT, Weng HH, Yuan YD, et al. Predictors of mortality in patients with necrotizing fasciitis. Am J Emerg Med 2008; 26:170-175.
- Secil M, Topacoglu H. Retroperitoneal necrotizing fasciitis secondary to colonic diverticulitis. J Emerg Med 2008; 34:95-97.
- Woodburn KR, Ramsay G, Gillespie G, et al. Retroperitoneal necrotizing fasciitis. Br J Surg 1992; 79:342-344.
- Wilkerson R, Paull E, Coville FV. Necrotizing fasciitis. Review of the literature and case report. Clin Orthop Related Res 1987; 216:187-192.
- Childers BJ, Potyondy LD, Nachreiner R, et al. Necrotizing fasciitis: A fourteen-year retrospective study of 163 consecutive patients. Am Surg 2002; 68:109.
- Mukhopadhyay M, Saha AK, Biswas RR, Biswas S. A clinicopathological study of necrotizing fasciitis. Diabetes. 2011; 17:34.
- Tian GJ, Guo Y, Zhang L. Non-invasive treatment for severe complex pressure ulcers complicated by necrotizing fasciitis: A case report. J Med Case Reports 2015; 9:1-4.
- Kobayashi L, Konstantinidis A, Shackelford S, et al. Necrotizing soft tissue infections: delayed surgical treatment is associated with increased number of surgical debridements and morbidity. J Trauma 2011; 71:1400-1405.
- Wipf SA, Greenhagen RM, Mandi DM, et al. Necrotizing soft tissue infection of the foot: A case report. Foot Ankle J 2008; 1:2.
Author Info
J Magesh Kumar, RNM Francis and V Ramalakshmi*
Department of General Surgery, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: J Magesh Kumar, RNM Francis, V Ramalakshmi, Necrotizing Fasciitis: A Clinical and Microbiological Study, J Res Med Dent Sci, 2021, 9 (4):442-451.
Received: 20-Mar-2021 Accepted: 27-Apr-2021
